24 Contouring of the arms, breast, upper trunk, and male chest in the massive weight loss patient
Synopsis
 Upper body contouring procedures in the massive weight loss (MWL) patient requires accurate assessment of the deformity and sound surgical planning.
Upper body contouring procedures in the massive weight loss (MWL) patient requires accurate assessment of the deformity and sound surgical planning.
 Patients must be willing to exchange improved body contour for lengthy scars in some cases.
Patients must be willing to exchange improved body contour for lengthy scars in some cases.
 Multiple body contouring procedures may be performed in a single stage. Upper body and breast procedures may be done at the same time as lower body procedures in well selected cases with an understanding that significant opposing vectors of pull should be avoided.
Multiple body contouring procedures may be performed in a single stage. Upper body and breast procedures may be done at the same time as lower body procedures in well selected cases with an understanding that significant opposing vectors of pull should be avoided.
 The breast deformity following MWL is complex. The technique of dermal suspension mastopexy with total parenchymal reshaping is a long-lasting and reproducible technique that utilizes the patient’s own tissues to autoaugment breast volume.
The breast deformity following MWL is complex. The technique of dermal suspension mastopexy with total parenchymal reshaping is a long-lasting and reproducible technique that utilizes the patient’s own tissues to autoaugment breast volume.
 Pseudogynecomastia in males following MWL is common, with varying degrees of deformity. For more severe cases, extensive skin envelope excess and nipple descent may be treated with a transverse elliptical excision with repositioning of the nipple areolar complex on a thin dermoglandular pedicle.
Pseudogynecomastia in males following MWL is common, with varying degrees of deformity. For more severe cases, extensive skin envelope excess and nipple descent may be treated with a transverse elliptical excision with repositioning of the nipple areolar complex on a thin dermoglandular pedicle.
Introduction to brachioplasty and axillary contouring
Upper extremity contouring procedures have exploded in popularity in the past decade. According to the American Society of Plastic Surgeons, arm contouring procedures increased by almost 4200% from 2000 to 2009.1 Following massive weight loss (MWL), varying degrees of upper arm deformity are seen, from minor residual fat deposits to large aprons of skin. Patients commonly complain of a “bat wing” deformity that may include the upper brachium, axilla, and lateral chest wall.2 Many techniques to contour the arm have been described. However, the severity of deformity following MWL requires new procedures and technical modifications to existing operations.
History
The first account of brachioplasty was by Correa-Iturraspe and Fernandez, commonly resulting in suboptimal results and frequent complications.3 Clarkson, among others, described further early operations for upper arm flaccidity and adiposity.4 McCraw published a case report on surgical reconstruction following MWL that included a technique of brachioplasty resulting in a posteriorly placed “T” shaped scar with dermolipectomies in the longitudinal and transverse planes.5
Early procedures involved the simple fusiform excision of skin and fat, usually performed on the medial arm.4,6 The result was maximum tightening in the mid-portion of the arm. However, the majority of patients have their maximum excess in the proximal arm. Less than ideal were the skin redundancies at both ends of the ellipse. Modifications of the longitudinal resection, including a technique of flap reduction with T closure by Juri allowed the surgeon to more aggressively contour the proximal arm and tighten the axilla.7 Techniques were further described to add curvilinear excisions around the elbow to deal with large excesses in the distal third of the arm, as well as adiposity in the pre-axillary and axillary regions.8
Results improved as new techniques were developed. Axillary scar contracture was not infrequently seen if excision crossed the axilla. The addition of Z- or W-plasties among other modifications in the area reduced this complication.7,9,10 Scar position is still controversial, but placement on the medial arm in the brachial sulcus allows it to be hidden with the arm at rest.9 Scar migration and widening have been decreased with use of the superficial fascial system, as well as anchorage and suspension of flaps to the clavipectoral fascia.11
Basic science/disease process
Commonly, the posterior axillary fold becomes deflated, causing significant descent, resulting in broadening of the attachment of the arm to the chest wall. This area originates from the lateral chest wall, and by definition, the skin excess merges with this area. The anterior axillary fold is enlarged and elongated. It is formed along the lateral border of the pectoralis major muscle, beginning at the pectoralis humeral insertion and ending at the superior-lateral breast.12 Axillary enlargement may be seen.
Diagnosis/patient presentation
Examination should note position and amounts of residual lipodystrophy, skin excess, along with their relative amounts, and assessment of the lateral thoracic wall. There have been a number of proposed classifications for the arm deformity following MWL.6 The Pittsburgh Rating Scale assesses adiposity, skin tone, and the extent of loose, hanging skin present.13 As a part of a complete history, key points that need to be elicited include:
• Weight loss history, including type of weight loss surgery
• History of lymphedema, or risk factors for upper extremity lymphedema such as prior lymph node dissection, axillary radiation
• Prior surgeries on the upper extremities
• History of nerve compression syndromes
Physical examination of the upper extremities should include:
• Determination of excess skin and fat (pinch test) and their relations – this is important to assess and record in the proximal, middle, and distal arm
• Lateral chest wall deformity (include contiguous rolls with the breasts, back), presence/amount of axillary descent
Patient selection
Choice of procedure is dependent on patient expectations, surgeon preference, as well as physical properties of the arms. The patient’s skin tone, amount of adiposity, and the extent of skin redundancy, all play a role. Patient selection is vital for a good outcome (Table 24.1).14
Table 24.1 Pittsburgh Rating Scale for contour deformities after bariatric weight loss: arm deformities
| Clinical findings | Preferred procedure | |
|---|---|---|
| 0. | Normal | None |
| 1. | Adiposity with good skin tone | UAL and/or SAL |
| 2. | Loose, hanging skin without severe adiposity | Brachioplasty |
| 3. | Loose, hanging skin with severe adiposity | Brachioplasty ± UAL and/or SAL |
(Adapted from Song AY, Jean RD, Hurwitz DJ, et al. Classification of contour deformities after bariatric weight loss: the Pittsburgh Rating Scale. Plast Reconstr Surg 2005; 116:1535–1546.)
In patients with good skin tone and adiposity with minimal skin excess, liposuction alone may be adequate, thus improving contour while omitting lengthy scarring. Ultrasound assisted liposuction is an excellent technique for arm contouring and may lead to greater postoperative skin contraction than traditional liposuction.15,16 Patients unwilling to have scars on the arms may be given the option of having conservative ultrasound assisted liposuction of the arms, followed by a dermolipectomy procedure to correct skin redundancy if retraction does not occur satisfactorily.
Patients with adiposity and moderate skin redundancy in the proximal arm may benefit from liposuction in conjunction with an excisional procedure (mini-brachioplasty) in the inner proximal arm.17–19 This may be in the form of an ellipse, or a T-shape. Patients with isolated horizontal laxity may require an elliptical excision in the axilla that results in a well-concealed scar. The addition of vertical laxity requires a T-type excision.
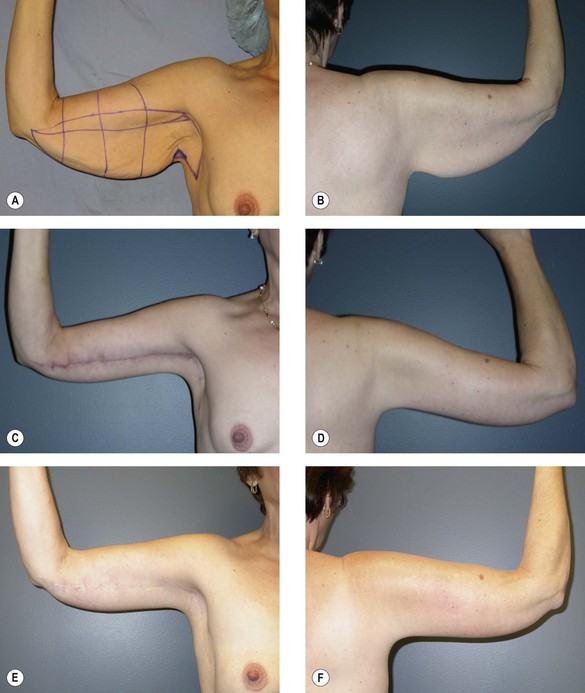
A mini-brachioplasty alone may be all that is necessary to treat mild to moderate skin redundancy in the proximal arm in the absence of significant adiposity, although this is a rare situation after massive weight loss.17 Patients with loose hanging skin down the length of the arm, without severe adiposity and with poor skin tone, good contour results can be obtained using excisional brachioplasty from axilla to elbow. Extension of the excision to the level of and distal to the elbow is sometimes necessary to deal with significant proximal forearm laxity. Extension into the axilla and down to the lateral chest directly contours these areas. Alternatively, a technique described by Goddio involves correction of ptosis, without excision based on rolling a de-epithelialized flap around from posterior to anterior.20
The ideal patient for a full-scar traditional brachioplasty procedure is one with loose hanging skin that more than doubles the width of the upper arm. In patients with severe adiposity and hanging skin, liposuction in conjunction with brachioplasty is necessary. The aggressiveness of brachioplasty is dependent on the extent of skin excess. Brachioplasty is commonly done in conjunction with other body contouring procedures and rarely performed in isolation.21
Numerous procedures have been described in the treatment of arm deformities following MWL.2,7,8,10,11,20,22–27 Controversy exists among surgeons regarding the position of the arms scar in full brachioplasty. Some advocate placement posteriorly on the arm, while some prefer placement in the brachial groove.9,22,27–29 While a posteriorly placed scar remains hidden to the patient looking in the mirror, others may see it from behind. The more anteriorly situated scar allows it to be hidden between the arm and chest wall with the arm at rest. Therefore, it is the preference of the authors to place the final scar in this position.
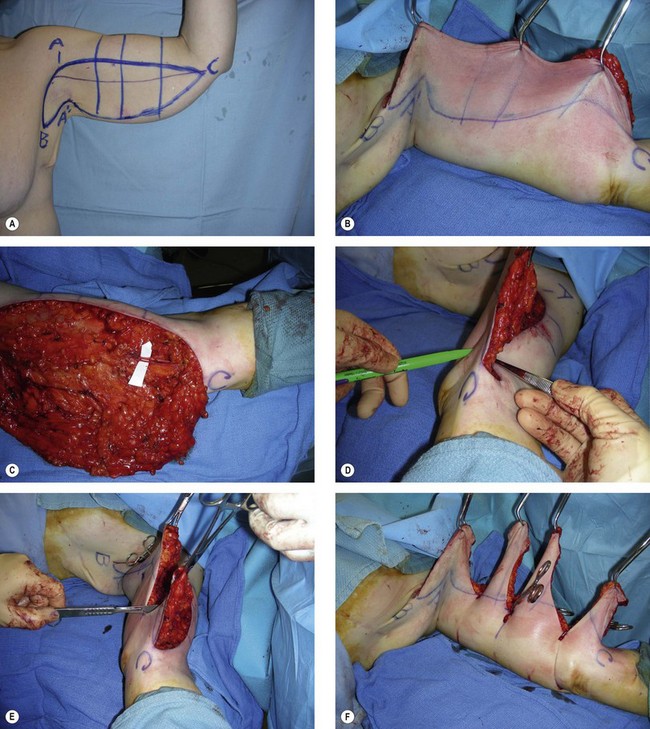
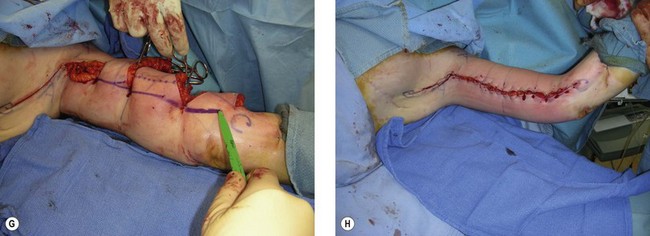
Treatment/surgical technique
With arms prepped and draped circumferentially to the lateral chest wall, the superior excision line is incised and carried into the axilla (Figs 24.1, 24.2). A posteriorly based flap is elevated superficial to brachial fascia. Care is taken to preserve any sensory nerves encountered. Medially, the flap is elevated just superficial to brachial fascia. Dissection in the axilla is more superficial.
Distally, the dissection becomes more superficial to protect the medial antebrachial cutaneous (MAC) nerve, which is usually found in conjunction with the basilic vein at the distal upper arm. A cadaveric study by Knoetgen and Moran demonstrated that although variable, the MAC nerve pierced the deep fascia at approximately 14 cm proximal to the medial epicondyle. They also noted that the MAC nerve did not always run in conjunction with the basilic vein, with some instances where the nerve was >5 cm anterior to the vein in the midarm.21 The medial brachial cutaneous (MBC) nerve is vulnerable during surgical flap elevation in the medial arm. It runs with the basilic vein and sends 2–4 branches to the skin 7 cm proximal to the medial epicondyle, and another few branches that pierce fascia to innervate skin 15 cm proximal to the medial epicondyle.30
Hints and tips
Arm contouring
• Communication with the anesthesiologist is imperative to avoid fluid overload that may increase edema and make closure excessively tight, or not possible.
• Various techniques may be performed to contour the arms. The surgeon must assess the amount of lipodystrophy, skin quality, and skin excess. The patient must be willing to trade possible extensive scars for improved contour.
• Prevent a tight or impossible closure of skin flaps during excisional brachioplasty by keeping IV fluid volume to the minimum necessary in order to reduce the soft tissue edema, double check excision markings of the flaps prior to incising flaps, performing excision immediately after liposuction of the arm (if liposuction is needed) and closing flaps as quickly as possible after excision.
• Leave a carpet of soft tissue over the brachial fascia in the distal third during flap elevation to protect sensory nerves.
• Brachioplasty procedures may safely be combined with other body contouring procedures in well-selected patients.
Outcomes, prognosis, and complications
Complication rates following brachioplasty have been reported to range from 25% to 40%.21,28 The majority of these complications were considered minor. A major disadvantage with a full-scar brachioplasty is a visible scar with variable scar quality and prolonged scar maturation.8,28,31 The scar may be red and raised for up to a year postoperatively. Other adverse events include edema, seroma and lymphoceles, paresthesias, neurapraxia or transection of the MAC or MBC nerves (possible neuroma formation), wound infection, suture extrusion or abscess, under-resection, and wound dehiscence.21,28 Possible over-resection of tissue with the inability to close is a complication that is generally avoidable with intraoperative confirmation of markings.
Hypertrophic scarring may be reduced by SFS approximation. Scar treatments may include silicone based products, scar massage, and other scar modalities. Injection of dilute steroid may be helpful.32 The surgeon should have a lower threshold for scar revision in the arm areas. At times, significant and poorly formed scars may occur and are difficult for the patient to conceal. Scar revision rates following brachioplasty range from 3–12%.21,24,28
Injury to the MAC and MBC nerves also may occur during excisional brachioplasty.30 A 5% rate of injury has been reported for the MAC nerve. On average, the MAC nerve became superficial in at a point approximately 14 cm proximal to the medial epicondyle.21 Depth of resection, with dissection more superficial in the distal arm region will leave an important amount of soft tissue coverage over this nerve and prevent injury.
Mastopexy and breast reshaping in the MWL patient
The youthful breast has been a symbol of femininity and beauty throughout the ages. Nipple descent and loss of parenchymal volume is suggestive of aging and loss of attractiveness. Regnault described a widely utilized classification for breast ptosis relying on nipple position relative to the inframammary fold.33 However, the breast deformity following MWL is more complex.
Basic science/disease process
Characteristic changes in the breast typically follow massive weight loss (Box 24.1). Volume deflation resulting in a stretched skin envelope, significant ptosis, and flattening of the overall breast shape occur. The nipple areola complex is medialized, and lateral chest rolls develop contiguous with the breast. The chest roll is a difficult area to treat and obscures the lateral curvature of the breast, blunting its shape. Breast asymmetry is the norm. A significant amount of skin excess occurs, while parenchymal volume may be deficient. The skin envelope may be thin and relatively inelastic. Internal supporting structures of the breast may be attenuated. Traditional techniques for breast ptosis are usually inadequate for these deformities.34,35
Traditional classification schemes to describe breast ptosis fall short in the MWL patient.33 To better describe deformities following MWL, the Pittsburgh Rating Scale was developed to classify contour deformities in this group of patients.13 Specific to breasts, the scale combines the Regnault grade of breast ptosis with volume loss, loose skin, and the presence or absence of lateral chest wall skin rolls (Box 24.2).
Diagnosis/patient presentation
Goals in mastopexy after massive weight loss are listed in Box 24.3.
Box 24.3
Goals in mastopexy after massive weight loss
• Elevation and repositioning of the nipple areola complex to the breast meridian
• Breast reshaping and tightening of the skin envelope
• Development of a natural and aesthetic curve of the lateral breast
• Volume recruitment, if possible, from the lateral thoracic roll
• Restoration of superior pole fullness
• Minimization of scar and proper scar placement
Variations in technique have been described, many using local flaps to autoaugment breast volume. Parenchymal suspension to chest wall structures, including pectoralis fascia, or rib periosteum have also been included.36–39
As in any breast procedure, a complete breast and medical history collected:
• Weight history (including history of weight loss surgery, lowest, highest, and current weight and BMI, recent weight fluctuations, length of time weight has been stable)
• Bra size: largest, current, ideal
• Personal, family history of breast cancer
• Prior breast abnormalities, masses
• Prior breast surgeries or biopsies
• Previous mammographic history
• Breast-feeding history, future plans for breast-feeding
• Genetic pre-disposition to breast cancer, history of ovarian, colon cancer.
Mammography should be performed according to American Cancer Society guidelines.40
Operative planning/patient selection
Many approaches to mastopexy have been described.41–47 After weight loss, the breasts usually are lacking in upper pole fullness, and it is difficult in the MWL to produce and maintain upper pole fullness with some techniques. Traditional breast reduction (Wise pattern or vertical) using a variety of pedicles to carry the nipple areola complex (inferior, lateral, superior, medial), augmentation with implant, and augmentation mastopexy may fall short in the MWL patient. Some methods to reshape the breast include dermal suspension techniques, while others discuss techniques to use local tissues for autoaugmentation. Graf et al. describe using a lateral thoracic wall flap suspended with a loop of pectoralis muscle to reshape the breast and add upper pole fullness.37
Grade III changes are best treated with parenchymal reshaping techniques with dermal suspension and autoaugmentation if volume deficient. Ignoring deformities of structures adjacent to the breast in the MWL patient (axillary fold, lateral chest wall) tends to lead to aesthetic disharmony and unsatisfactory results.36 Techniques dealing with grade III changes include the recruitment of laterally based thoracic flaps, the rotation-advancement of a supero-medial pedicle, as well as the simultaneous use of implants for additional parenchymal volume.48
The addition of a lateral thoracic flap based on intercostal perforators allows the recruitment of soft tissue to augment insufficient breast volume, along with simultaneous removal of commonly found lateral thoracic soft tissue excess. The intercostal perforators that require preservation are located along the anterior axillary line, parallel to the lateral border of the breast.49 It is not possible to preserve perforators through the latissimus muscle however. Dissection is generally carried out in a plane deep to the fascia.
A Wise pattern technique with use of a variety of pedicles, including the supero-medial pedicle may be utilized in patients with adequate parenchymal volume in order to provide parenchymal reshaping. The addition of implants to supplement volume and improve upon upper pole fullness may be considered. In any patient with inelastic skin, the size of implant should remain conservative. Larger implants will not be adequately supported by the remaining breast structures and lead to implant descent and recurrent ptosis. If mastopexy with augmentation is planned, the safest method to manage more severe cases of breast ptosis is to stage the procedure. If larger implants are considered, additional support with cadaveric dermal products may be used to minimize the risk of implant descent.50,51
A de-epithelialized inferior pedicle used in conjunction with a separate pedicle to carry the nipple areola complex may also reshape the breasts with addition of superior pole fullness.47 Parenchymal tissues may be either suspended to stable chest wall structures (pectoralis fascia, rib periosteum) or by a loop of pectoralis muscle.37,52 Plication of parenchymal or de-epithelialized dermis allows for increased projection and reshaping of the underlying glandular structure.34,48
Choice of technique is dependent on breast morphology, patient desires and expectations, and surgeon preference (Table 24.2). An important assessment is whether or not the patient is happy with the current volume of the breasts in a bra. This will guide the surgeon as to the need for only parenchymal reshaping, breast reduction, or addition of volume (autoaugmentation or implant placement).53
Table 24.2 Surgical options for the breast after massive weight loss
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree