Fig. 18.1
(a) Congenital clasped thumb with lack of extension of MCP joint only and active extension of the IP joint. (b) Palmar contracture of the thumb
Clinical Picture
Congenital clasped thumb has heterogeneous presentations. The main finding is lack of active extension of the metacarpophalangeal (MCP) joint of the thumb. Anderson and Breed suggested that the Moro reflex might be a useful way to detect congenital clasped thumb early. The thumb normally extends during the Moro reflex [6].
Lack of active extension may involve also the interphalangeal (IP) joint of the thumb (Fig. 18.2). There may be callosities on the dorsum of the IP joint secondary to grasping objects against that side of the thumb (see Fig. 18.2). The carpometacarpal (CMC) articulation may be mobile and show active extension or may be stiff, especially in cases of severe deformity or generalized disorders. Full passive range of movement of the thumb indicates absence of soft tissue contractures. Passive limitation of extension of the thumb with full wrist extension may reveal hidden shortening of the flexor pollicis longus (FPL) muscle. Limitation of passive extension of the thumb with the wrist in neutral position indicates the presence of palmar soft tissue contractures that may be associated with skin webbing at the level of MCP joint (see Fig. 18.1b). The first web space may show variable degrees of narrowing and skin deficiency (Fig. 18.3). The MCP joint may show variable degrees of instability that may become evident only after release of flexion contracture. In severe cases, the thumb may appear very short, stumpy, adducted, flexed, and externally rotated (see Fig. 18.3). The thenar muscles may show some degree of mild hypoplasia. Severe thenar muscle hypoplasia or aplasia points to the diagnosis of congenital hypoplastic thumb type III [7] with predominant deficiency of extrinsic extensor tendons rather than clasped thumb. Meticulous examination and analysis of deformities are mandatory to plan treatment accordingly.
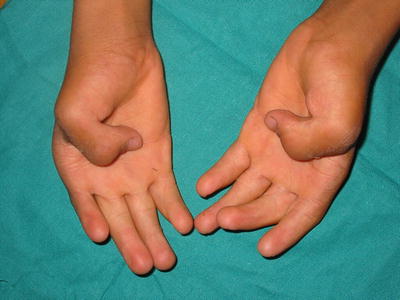

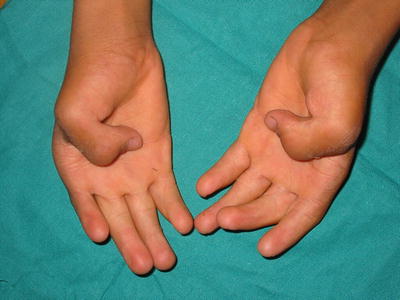
Fig. 18.2
Congenital clasped thumb with flexed IP joint indicating combined deficiency of both EPL and EPB. Callosities are evident on the dorsum of IP joint

Fig. 18.3
Clasped thumb with severe narrowing of the web space and extension contracture of the wrist
Associated deformities of the hands with clasped thumb include abnormal skin creases (see Fig. 18.2), stiffness of the fingers with incomplete flexion (see Fig. 18.2), wrist extension deformity (see Fig. 18.3), camptodactyly (Fig. 18.4), radial deviation of index finger (Fig. 18.5), lack of extension of the index finger (Fig. 18.6), and ulnar drift hand (Fig. 18.7).





Fig. 18.4
Clasped thumb with camptodactyly of the four fingers

Fig. 18.5
Radial deviation of the index finger at the level of the MCP joint in association with clasped thumb

Fig. 18.6
Clasped thumb associated with deficient extensors of the index finger

Fig. 18.7
Ulnar drift hand
Ulnar drift hand is characterized by ulnar deviation of the fingers at the level of the MCP joints with or without flexion contracture of the MCP joints. Although ulnar deviation of the fingers is the most common feature of ulnar drift hand, webbing of the thumb to the palm is the most limiting disability [8].
Clasped thumb could be diagnosed in radial club hand in the presence of well-developed thenar muscles and flexed thumb (Fig. 18.8) [9].


Fig. 18.8
Radial dysplasia with congenital clasped thumb evident by the presence of well-developed thenar muscles and flexed thumb
Some cases show lack of extension or severe hypoplasia of index finger or index and middle fingers and the only active functioning fingers are the ring and little ones (see Fig. 18.6). After correction of thumb deformity, the patients continue to grasp with the thumb against the ulnar most fingers.
Congenital clasped thumb commonly manifests as part of generalized disorder especially multiple joint contractures syndromes collectively called arthrogryposis, which is a purely descriptive term [2, 9–12]. Arthrogryposis is defined as the presence of two or more joint contractures in multiple body areas [2]. Wood considered ulnar drift hand representing a conglomerate of syndromes and different anatomical causes. Probably all of these cases represent a forme fruste of arthrogryposis [8].
Arthrogryposis with CNS involvement includes chromosomal abnormalities and other syndromes [13].
Congenital clasped thumb should be differentiated from trigger thumb, where a palpable nodule of the flexor pollicis tendon is present at the level of the MCP joint. When locked, the IP joint is flexed with extension of the MCP joint and a palpable clunk is felt on unlocking the trigger thumb and extending the IP joint.
Pathoanatomy and Classification
Many authors have suggested that flexor extensor imbalance is central to the development of clasped thumb. The long extensor tendons are not totally absent, but vestigial strands or hypoplastic extensor tendons are always present [9, 10, 14–16]. Flatt [16] found that in the course of tendon transfer, the vestigial tendon narrows proximally and eventually ends in fibro fatty tissues rather than muscular tissue. Crawford et al. [15] found that on releasing the flexion contractures, all tissues were involved, including skin, subcutaneous fascia, and periarticular structures. They also found an increase in fibrous tissue present in the form of numerous subcutaneous strands in the digits, palm, and forearm, making dissection, mobilization, and transfer of the tendons more difficult than anticipated [15, 17].
Weckesser et al. [11] classified congenital clasped thumbs into four groups. Group I consisted of isolated clasped thumb. The extensor pollicis brevis (EPB) or extensor pollicis longus (EPL) muscles and tendons are either weak or attenuated. In addition to the deformities seen in group I, group II patients have associated flexion contractures of the fingers. These deformities are believed to be the result of mild to moderate arthrogrtyposis. Group III deformity is related to radial ray hypoplasia with findings of hypoplasia of extensor, flexor, and thenar muscles as well as associated osseous elements. Group IV patients are a miscellaneous category that include polydactyly. The authors believe that this classification includes cases that should not be considered as clasped thumbs.
McCarroll [10] classified congenital clasped thumbs into supple and complex types. The former is characterized by lack of active thumb extension with ability to fully reverse the deformity passively. The latter group may demonstrate soft tissue contractures, lax ligaments, and tight skin in addition to the lack of active thumb extension.
Tsuyuguchi et al. [12] designed a classification consisting of three groups: Group I: The supple clasped thumb, where the thumb is passively abductable and extendable against the resistance of thumb flexors, without other digital anomalies. Group II: The clasped thumb with hand contractures, where the thumb is not passively extendable and abductable, with or without other digital anomalies. Group III: The clasped thumb, which is associated with arthrogryposis or windblown hand.
The authors have not found any anatomical differences or different outcome between Tsuyguchi’s types II and III, so we prefer using the McCarroll subtypes [9].
In complex cases, abnormal articular surface of the first MCP joint was described with hypoplasia of the volar aspect of the first metacarpal head. The dorsal capsule of the MCP joint may be adherent to the cartilage of the metacarpal head and sharp dissection was needed to separate it [9, 15]. The flexion contracture of the MCP joint is secondary to skin deficiency, abnormal subcutaneous fibrous tissue, and contracted periarticular structures including volar plate, collateral ligaments, and capsule [9, 10]. Shortening of the FPL may add to the flexion contracture. Narrowing of the web space is secondary to contracture of one or more of the following structures: palmar fascia, adductor pollicis, and first dorsal interosseous muscles [9]. The pathology of complex clasped thumb could be summarized as hypoplastic or attenuated thumb extensors, flexion contracture of MCP joint, ulnar collateral laxity or global instability of the MCP joint, adduction contracture of the CMC joint, and contracture of the first web space. We noted that the severity of these pathological findings is variable, and dependent on the age of the patient at the time of surgery [9, 16].
Prevalence and Etiology
Congenital clasped thumb occurs twice as often in males as in females and it is bilateral in more than 80 % [9, 11, 16, 18]. Positive family history of 32–36 % was reported [9, 11]. Positive consanguinity was reported as high as 60 % [9]. The high incidence of bilateral deformity implies that a defect is present in the zygote before the first cell division. In supple deformity, the very limited and specific nature of the defect also suggests that the cause is a genetic defect rather than some environmental influence on the zygote which would be much more likely to produce widespread defects. The familial occurrence of this anomaly in a number of cases adds to the evidence for genetic defect [9, 11].
The high incidence of defect in the EPB may have a phylogenetic basis in that this phylogenetically new muscle is found only in the gorilla and in man [11].
Most of the cases of congenital clasped thumbs are part of generalized disorders. Abdel-Ghani et al. [9] reported associated congenital malformation in 77.5 % of cases, incidence of 15 % of associated malformations of the hand [9, 19], and 68 % incidence of associated syndromes [9]. The most common associated anomalies are manifestations of congenital contractures: congenital hip dislocation, congenital knee dislocation, knee stiffness, congenital clubfeet, congenital vertical talus, scoliosis, elbow stiffness, and limited shoulder movement. Rarely reported associated anomalies were ventricular septal defect and congenital blindness [9]. There were no reported abdominal anomalies in association with clasped thumbs [9, 19, 20].
In the majority of cases, congenital clasped thumb is part of congenital multiple contractures loosely termed arthrogryposis. Arthrogryposis, as defined before, describes the multiple congenital contractures that are part of more than 200 different disorders. Arthrogryposis could be classified into three major categories: amyoplasia, distal arthrogryposis, and syndromic arthrogryposis [13].
Amyoplasia is also called arthrogryposis multiplex congenital (AMC) or classic arthrogryposis. It is the most common form, seen in approximately 1/3,000 live births [9], and has sporadic incidence with no genetic or hereditary predisposition [20].
The second group is distal arthrogryposis syndromes, which are a group of autosomal dominant syndromes with congenital contractures primarily involving the hands and feet, which often are associated with abnormal facies without primary neurological and/or muscle disease affecting limb function [13]. Many affected individuals present in an orthopedic setting. There are at least 10 different types of distal arthrogryposis that include a large number of syndromes [13, 21]. The most common distal arthrogryposis syndromes that are linked to clasped thumbs are Freeman–Sheldon syndrome, multiple pterygia syndrome, digitotalar dysmorphism, clasped thumb clubfoot syndrome, and congenital contractural arachnodactyly [21]. In amyoplasia and distal arthrogryposis, neurological examination is normal.
The third group of congenital multiple contractures include a great number of genetic syndromes and chromosomal anomalies. This group is characterized by abnormal neurological examination secondary to central nervous system or peripheral neuromuscular disorders. This group is a common cause of arthrogryposis and responsible for the most severe forms. Central nervous system disorders can be suspected on clinical examination if hyperreflexia, unilateral arthrogryposis, or cognitive deficits are present and can be anatomically localized by magnetic resonance imaging of the brain or spinal cord [13]. This group includes a great number of genetic syndromes and chromosomal anomalies. Examples from this group are COFS (cerebro-oculo-facio-skeletal) syndrome, congenital muscular dystrophy, Miller–Dieker (lissencephaly), lethal multiple pterygium syndrome, Pena-Shokeir phenotype, Potter syndrome, Zellweger syndrome, trisomy 8/mosaicism, trisomy 18, and many others. This group includes lethal syndromes and syndromes with severe disabilities due to central nervous system malfunction.
Mental retardation/CNS involvement is found in approximately 25 % of individuals with arthrogryposis [13, 22].
The features of these syndromes are described to allow diagnosis, establish prognosis, provide family counseling, and treatment. Increased recognition will lead to improved knowledge of the natural history [21].
Arthrogryposis appears to occur secondary to fetal akinesia (lack of movement), which is the common endpoint of several different in utero processes. The causes of arthrogryposis include conditions that are intrinsic to the fetus, such as neuromuscular disorders, skeletal dysplasias or aneuploidy, as well as those resulting from influences extrinsic to the fetus [23].
While the pathoanatomy and pathophysiology vary and continue to be investigated, it appears that the joints initially have full developmental potential but fail to form mobile articulations secondary to the absence of movement in utero. This theory has been supported by a number of chick embryo studies, in which paralytic agent were administrated during development, resulting in abnormal joint morphology and stiffness [24]. The lack of joint motion results in articular cartilage abnormalities, failure of joint cavitation, and secondary fusions.
Amyoplasia has an increased prevalence in twins and in extrinsic conditions that would lead to decreased limb movement, such as a bicornuate uterus, oligohydramnios, or intrauterine crowding [25]. Also it may be secondary to major vascular insult to the fetus [22].
Treatment
Supple Clasped Thumb
Most of these cases respond to non-operative treatment. In young infants, especially those with shortening of FPL muscle, they respond well to manipulation by the mother. Manipulation entails bringing the thumb out of the palm and holding it in an extended position. Stretching exercises should be done while the wrist is in extension to effectively stretch the short FPL muscle. Mothers are instructed to do exercises with every feeding and diaper change.
Splinting is used if there is no active thumb extension after trial of manipulation. We find difficulty in applying splints in very young infants or small hands. Different forms of splints were used. We use a rigid splint that keeps the wrist in full extension and the thumb in full abduction and extension of the MCP joint. There is no solid protocol for splinting; almost similar protocols were followed by Weckesser et al. [1], McCarroll [10], Lipskeir and Weizenbluth [32], and Abdel-Ghani et al. [9]. Currently, we start exercises at the time of presentation if splinting cannot be started. Once we can use splints, full-time splinting is adopted until observing active thumb extension. This is followed by daily exercises and night splinting for further 6 months. Flatt [16] mentioned that if there is no improvement of the posture of the thumb or absolute lack of any active extension after 3 months of splinting, then it is reasonable to assume that the EPB is non-functional. He assumed that there is no harm in continuing splinting for further 3 months, but it is unlikely to have active thumb extension after this extra time of splinting [16].
Lin et al. [18] reported successful treatment of supple form with splinting in patients below 1 year of age. Tsuyuguchi et al. [12] and Abdel-Ghani et al. [9] reported excellent results of splinting in all patients with supple clasped thumbs in all their patients with an average time of splinting more than 3 months. In our practice, most of the patients presented early, before age of 6 months, with shortening of FPL respond well and restore full active thumb extension with proper stretching exercises.
The long-term results of treatment with corrective splinting have been shown to be good if the response to primary treatment was good. No adverse effects on growth of the hand have been noted [16].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







