Compression
 INTRODUCTION AND HISTORY
INTRODUCTION AND HISTORY
To excel in phlebology, the physician must understand the basic concepts of compression, including physiologic effects, common terms, rationale for the use of compression in the prevention and treatment of varicose and telangiectatic veins, as well as the rationale and use following sclerotherapy, ambulatory phlebectomy, and endovenous ablation. Although modern compression stockings have been an invention of twentieth-century medicine, the concept of compression for varicose veins dates back to antiquity. Compression therapy for treatment of venous disease was mentioned in the Old Testament (Book of Isaiah, chapter 1, verse 6).1 Roman soldiers noted that the application of tight bindings to the legs could reduce leg fatigue. In the late 1700s, Theden used modified lace-up dog leather stockings, originally described by Fabrizio d’Aquapendente (1537–1619), in the treatment of varicose veins of pregnancy.
Nelson Goodyear developed elastic medical compression bandages and stockings, made possible by the invention of vulcanization in 1842. Rubber harvested from the rain forests of Brazil was turned into elastic threads to weave stockings. Although uncomfortable, stockings made from rubber threads were utilized until Jonathan Sparks patented a method for winding silk and cotton around the rubber threads. This allowed more widespread use of elastic compression.2
As technical advances in the manufacturing process were made during the late 1800s and early 1900s, ultrafine rounded latex yarns (particularly with the later advent of circular-knitting versus flat-knitting techniques) became available that permitted the construction of modern compression stockings. Two-way stretch stockings were then developed. Rubberless compression stockings became available with the development of synthetic elastomers in the 1960s, giving rise to the modern seamless, relatively comfortable compression hose available today.
 PHYSIOLOGIC EFFECTS
PHYSIOLOGIC EFFECTS
Normal force generated within the venous system by muscle contraction is additive with external applied pressure (Table 15-1). This augmentation of the calf-muscle pump occurs by external application of graduated compression and increases the return flow upward from the leg.3 In ambulatory patients with superficial venous insufficiency, improvement can be demonstrated with graduated compression stockings with an ankle pressure of as little as 18 mmHg.4 After 90 days of elastic compression with a 30- to 40-mmHg graduated compression stocking, patients with cutaneous manifestations of venous stasis demonstrate noteworthy improvements in the structural pattern of dermal connective tissue.5 Compression reduces the edema which separates the skin and dermal tissues from direct contact with the superficial capillary network as this edema resides primarily in the papillary dermis.6
TABLE 15-1
Physiologic Effects of Compression
1. Mechanically externally enhances the calf-muscle pump
2. Diverts flow into competent veins by closing incompetent superficial veins
3. Makes incompetent valves work by decreasing diameter between leaflets of valves in varicose veins
4. Reduces edema which separates the skin from capillaries
5. Augments lymphatic flow
Graduated compression hose leads to normalized nutritional exchange and waste product removal. External “graduated” compression counterbalances the lost elasticity of the tissues to augment lymphatic flow. This flow is also expanded through an increase in hydrostatic pressure that prevents reaccumulation of edema.7 Compression, particularly inelastic, also decreases the size of deep muscular veins, thus increasing pressure within them and augmenting venous return.8
 TERMINOLOGY
TERMINOLOGY
For the sake of understanding external compression, the process of walking is arbitrarily divided into a working phase (calf-muscle contraction with plantar flexion) and an alternate resting phase (relaxed). Resting pressure is the pressure arising from the compression bandage pushing against the skin without muscular action. The greater the tension and stretch of the bandage, the greater the resting pressure. Working pressure is the compression that occurs from the bandage during muscle contraction. This pressure is the counterpressure of the stocking exerted on the calf during foot flexion phase of walking. This should not be confused with end pressure or end resting pressure, which is the additive effect of multiple compression stockings or bandages placed on top of one another to increase the resting pressure. Typically, the application of external compression leads to an increase in the working pressure, which leads to an increase in the ejection of venous blood from the leg.
To make compliance with compression easier for an elderly individual, it is possible to place two compression stockings on top of one another. For example, two 20-mmHg stockings can be worn to roughly equal the end pressure of a single 40-mmHg compression stocking. Resting pressure and working pressure are important when evaluating the types of bandage or compression stocking to be employed for appropriate applications. Typically, the application of external pressure results in reduced venous stasis.
The terminology of the types of compression bandaging includes nonelastic, short stretch, and long stretch. Nonelastic bandages are totally rigid, unyielding to the expanding leg, and capable of providing high working pressures. This is transmitted directly to the deep compartment of the leg, where the deep veins are compressed with increased pressure and proximal flow is increased. These bandages are most useful when edema of the leg is marked and muscular movement provides very little change in the shape of the leg. The typical example is a zinc gel (Unna boot, Gelocast) which dries to an inflexible “cast” around the leg. The edema must give way under a rigid, inflexible bandage since the bandage itself is unyielding. Application of inelastic compression must occur carefully to avoid overcompression that causes arterial ischemia and/or increased compartmental pressure. Inelastic compression must be reapplied frequently as edema decreases, since working pressure rapidly drops with decreasing edema.
Short-stretch bandages are also important to treat edema and have high working pressures similar to inelastic compression. The fabric of these bandages is usually extensible, primarily because of the weave pattern; they can stretch by expanding the distance between loops without the presence of rubber, nylon, or polyurethane. Therefore, they can be made entirely of comfortable natural fibers, e.g., Comprilan (Beiersdorf, Norwalk, CT), which is 100 percent cotton. Short-stretch compression is applied with fabric stretch of only 30–50 percent. Short-stretch bandages exert pressure when the calf muscles are relaxed and prevent expansion in calf diameter when the muscles are contracting (“working”). They have a low-to-slight resting pressure and a very high working pressure, exerting effect mainly within the deep venous system.9 Short-stretch bandages are comfortable when patients are recumbent (low resting pressure) and act to decrease superficial venous pressure mainly with ambulation (high working pressure). They increase deep venous flow more than they impede reflux at rest and can be worn at night. They are recommended to clear severe edema.10
Long-stretch bandages can be stretched 100–200 percent in at least one direction, (usually longitudinally) and 30–40 percent in the other direction (transversely). Long-stretch materials are most commonly known as graduated compression stockings. These have a high resting pressure because elastic recoil exerts high pressure on the leg as it attempts to return to the resting position.11 Graduated compression stockings move easily during muscle contraction (the working phase) but exert significant resting pressure on the superficial venous system, which minimizes reflux when the limb is at rest. Because of the ability to compress veins at muscular rest, compression stockings are useful for patients with superficial venous insufficiency who work in jobs requiring limited leg muscular contraction. However, when the patient is recumbent, these may be uncomfortable and cause arterial constriction due to the high resting pressure. Compression stockings slow the progression of disease, provide maintenance therapy, and are highly valued for post-sclerotherapy compression of superficial varicosities.12 In addition, even lightweight compression has been shown to reduce symptoms of venous hypertension.13
In contrast with the uniform compression provided by medical stockings, the compression provided by wrapped bandages depends greatly on the experience of the practitioner. Skilled clinicians can apply bandages with a pressure that ranges from 25 mmHg to 50 mmHg, while the bandages applied by less-skilled clinicians exert a pressure that ranges from 15 mmHg to 70 mmHg.14 Poor control over the amount of pressure applied can be a serious clinical problem, as compression that is too high can cause arterial occlusion and can also produce trophic skin breakdown over bony prominences. Application of wrapped bandages requires a technique which applies greater compression distally and less compression advancing up the leg.
 CLASSES OF COMPRESSION
CLASSES OF COMPRESSION
Compression stockings have empirically been divided into four compression classes (Table 15-2) by the Compression Stocking Commission of the German Working Group on Phlebology, based on the counterpressure at complete rest at the ankle and on the indications for that counterpressure. Class I compression is approximately 20 mmHg at the ankle. The indications for class I compression are leg fatigue or heaviness, mild early varicose veins without associated edema, and early varices of pregnancy. Class II compression is roughly 30 mmHg at the ankle. The indications for class II compression include more severe symptoms, marked varicosities, mild-to-moderate edema, and marked varicose veins of pregnancy. Class II compression is also indicated following sclerotherapy, ambulatory phlebectomy, and other venous surgery, and in patients with superficial thrombophlebitis or with healing venous ulcers.
TABLE 15-2
Counterpressure Exerted by Various Compression Classes
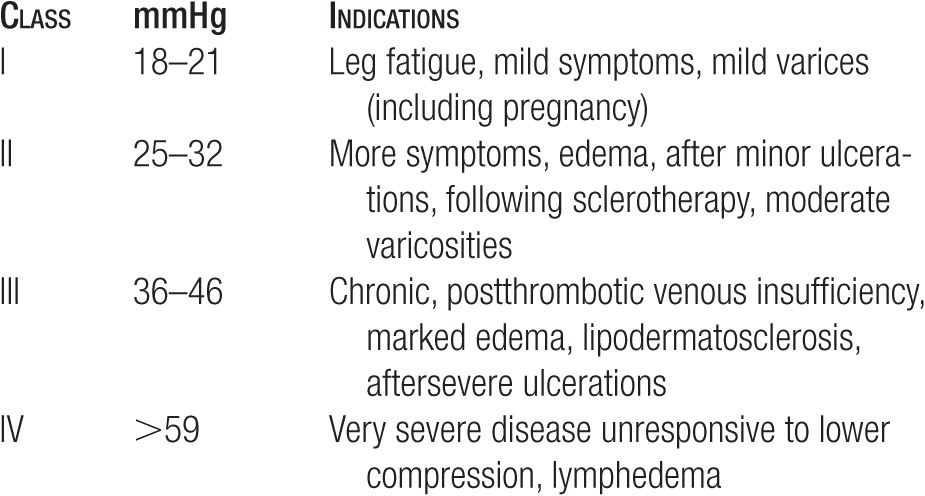
Class III compression, which is roughly 40-mmHg counter-pressure at the ankle, is indicated for marked edema, lipodermatosclerosis, and all serious sequelae of chronic, postthrombotic venous insufficiency. Class IV compression, greater than 60-mmHg compression, is reserved for severe diseases unresponsive to the previous classes of compression and for patients with lymphedema. Class IV stockings must be specially fitted, are not routinely available without special order, and have a high risk of causing arterial occlusion.
Full-leg stockings are preferred in every patient, although with elderly patients, some compromise may be necessary. Some compression is better than no compression. A patient with thigh varicosities and ankle edema who refuses to wear a thigh-high stocking will still benefit from knee length compression, because venous return will be improved with increased efficacy of the calf-muscle pump. Some stasis may be observed at the upper (proximal) edge of compromised compression. This includes edema, swelling, and erythema, but the patient should be informed that these changes are not harmful, but that full-leg compression would mitigate these changes.
 PRACTICAL APPLICATIONS OF LAPLACE’S LAW
PRACTICAL APPLICATIONS OF LAPLACE’S LAW
Laplace’s law (Pressure = Bandage tension/Radius of surface) describes the distribution of pressure of an elastic sleeve stretched over a cylindrical surface. This principle is more clearly stated as the smaller the radius (the tighter the turn), the higher will be the applied pressure. Stockings that are perfectly fitted will have a constant amount of stretch at every level of the leg; thus, the greatest pressure will be in the ankle, where the radius of curvature is small, and the least pressure will be in the thigh, where the curvature is most gentle.
Irregular contours around the knee and at the malleoli of the ankles make it difficult to maintain evenly graduated compression. To make irregular areas of the leg as cylindrical as possible, protruding surfaces (such as malleoli) must have their curve lessened with padding on each side, and flat areas must have their curve increased (with pads or cotton rolls) to produce a slight bulging, a smaller radial circle with increased pressure (Figure 15-1). Laplace’s law allows us to increase compression selectively over treated varicose veins: a foam pad or cotton roll over the vein will cause a smaller radius curve at the site and will produce a greater force.
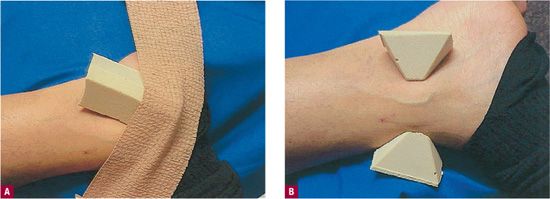
![]() FIGURE 15-1 Practical application of Laplace’s formula. Padding is applied beneath a compression stocking to approximate the profile of a cylinder. This allows for the most even application of pressure. Pressure is most evenly distributed when approaching a cylinder. A. Flat areas are rounded and B. projecting areas are made less round. Laplace’s formula (Pressure = Compression/Radius, i.e., the greater the curve or the smaller the radius, the greater the pressure).
FIGURE 15-1 Practical application of Laplace’s formula. Padding is applied beneath a compression stocking to approximate the profile of a cylinder. This allows for the most even application of pressure. Pressure is most evenly distributed when approaching a cylinder. A. Flat areas are rounded and B. projecting areas are made less round. Laplace’s formula (Pressure = Compression/Radius, i.e., the greater the curve or the smaller the radius, the greater the pressure).
 COMPRESSION BANDAGES AND GRADUATED COMPRESSION STOCKINGS
COMPRESSION BANDAGES AND GRADUATED COMPRESSION STOCKINGS
The primary differences between bandages and stockings are summarized in Table 15-3. Unlike stockings, the compression supplied by bandages is dependent on bandaging technique, as varying the amount of stretching force used during wrapping can alter pressure. The proper technique is illustrated in Figure 15-2. Principles of compression bandage application are listed in Table 15-4. A popular technique is the four-layered compression bandage.15
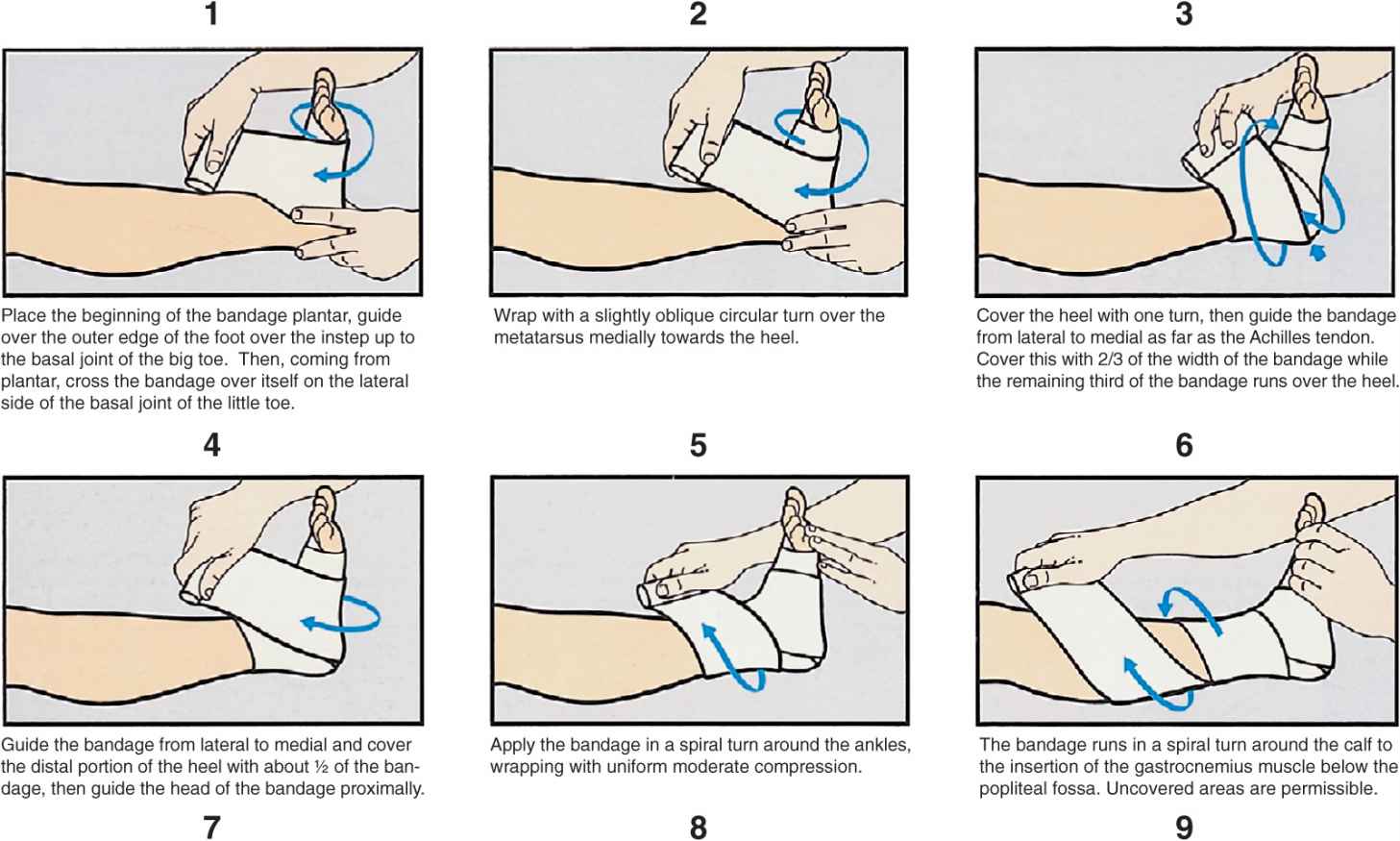
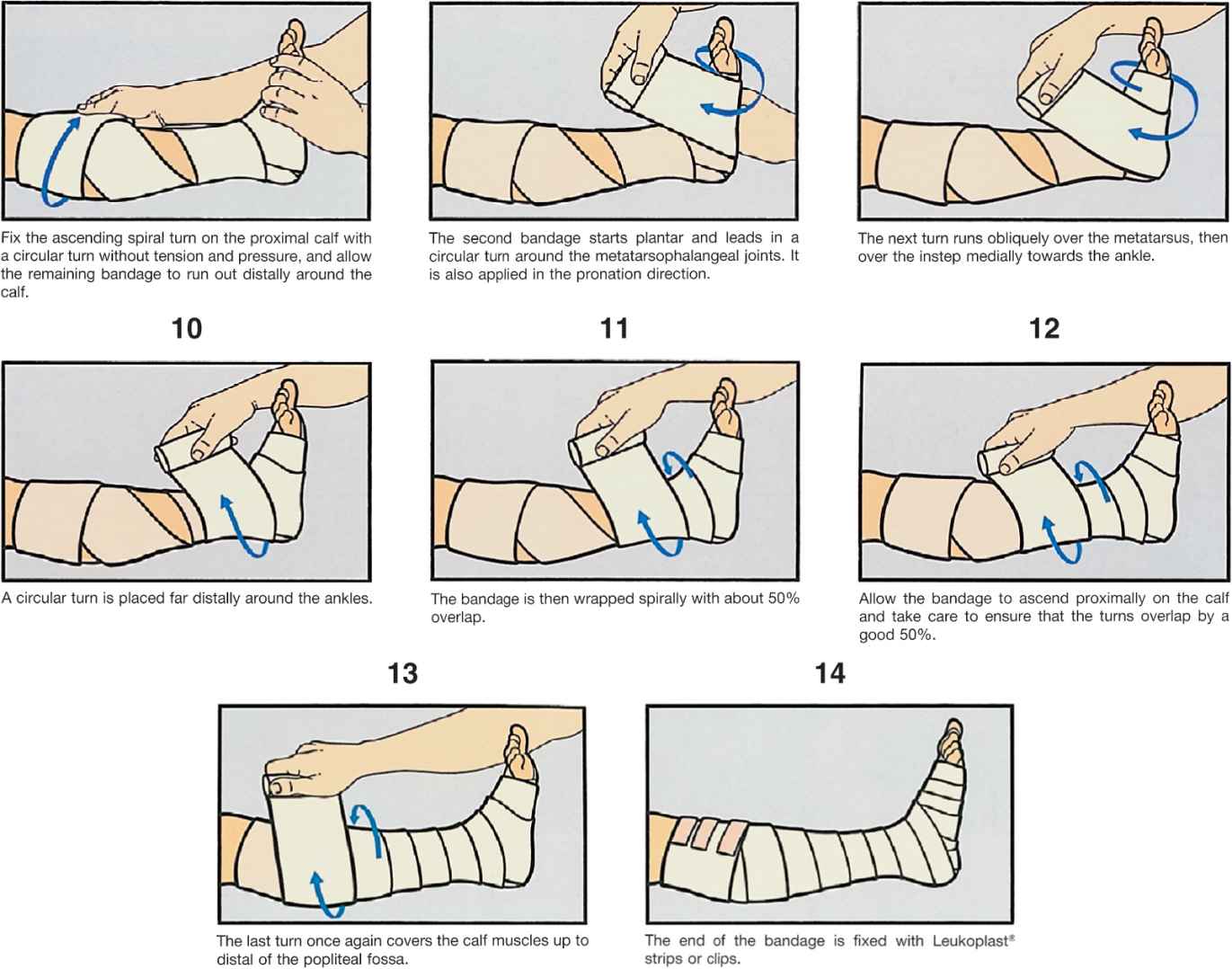
![]() FIGURE 15-2 Proper application of compression bandage (printed with permission from Beiersdorf Medical Bibliothek, Nurnberg, Germany).
FIGURE 15-2 Proper application of compression bandage (printed with permission from Beiersdorf Medical Bibliothek, Nurnberg, Germany).
TABLE 15-3
Comparison of Medical Compression Bandaging with Medical Compression Stockings
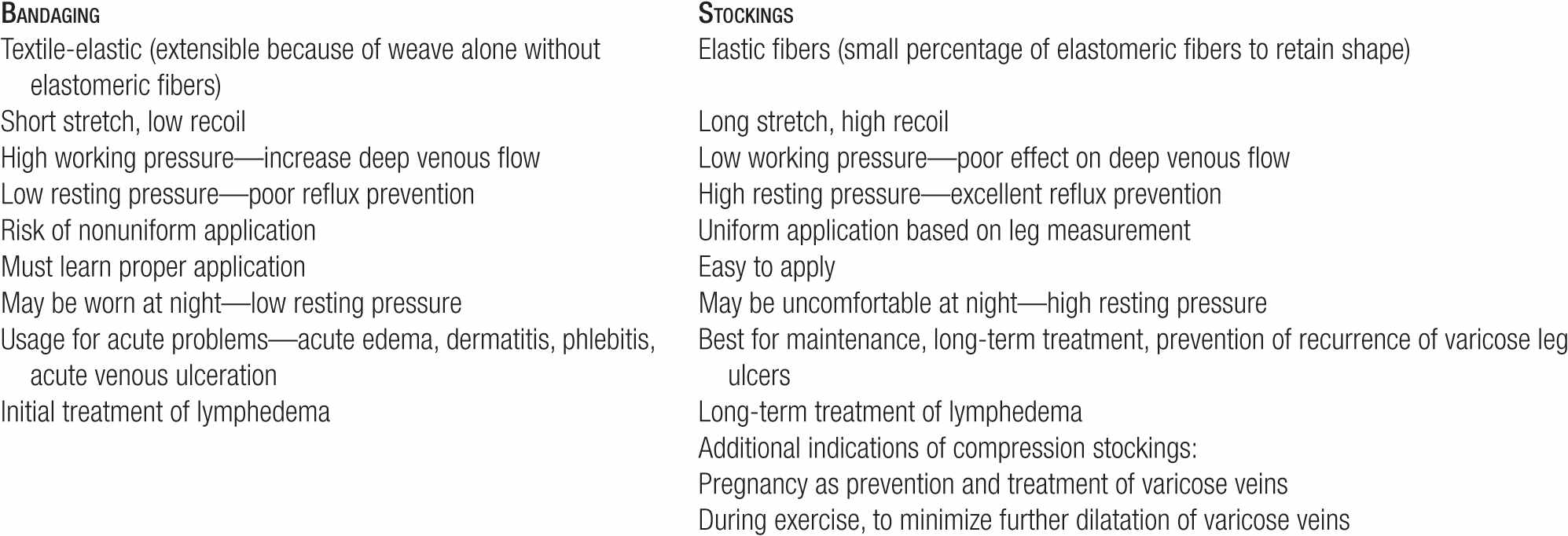
TABLE 15-4
Principles of Compression Bandage Application
1. Usually no greater than 50% stretch is applied to bandage during application.
2. No gaps are maintained so that each turn overlaps 50–70% of the previous turn to avoid skin pinching.
3. Oblique (not circular) turns of the bandage minimize constriction of the skin
4. At the ankle and the knee, a two-way stretch elastic bandage better conforms to the shape of the joints and is thus more comfortable than short-stretch (one-way) elastic bandages, which are preferred on the rest of the leg.
5. The ankle joint should be maximally extended dorsally when the bandage is applied.
6. Some form of padding or foam should be placed on the anterior tibial and retromalleolar area to both protect thin-skinned areas and evenly distribute pressure.
7. A rough-textured underwrapping (such as Medi-Rip) may be applied to minimize slippage of the compression bandage.
8. Local compression should be applied 5–10 cm beyond affected areas to avoid bruising, hematoma, edema. and inflammatory reactions.
9. Graduated compression is achieved by applying even pressure on the bandage, which is stretched to a uniform degree while wrapping from distal to proximal direction. This occurs because Laplace’s law governs that smaller diameters have increased pressures as long as tension remains constant and the leg increases in diameter from a distal to proximal direction.
10. Pressure may be increased by application of multiple layers of compression bandage.
In order to minimize slipping of compression bandages, rough-textured elastic gauze can be utilized as a supplemental underbandage. When patients apply compression bandages at home, they require detailed instruction and supervised practice before they leave the physician’s office, as well as explicit written instructions and diagrams for use as a home reference.
Because bandages loosen themselves over time, the principal indication for compression bandages is for temporary compression, such as in patients with marked edema or inflammatory conditions in which an improvement can be expected in a relatively short time period. Bandages are useful in edema because they can be continually reapplied as the edema in the affected limb is reduced. Unlike stockings, which must be long stretch in order to fit over the foot and ankle, limited-stretch bandages can be continually reapplied and tightened as edema is reduced. Additionally, the deep venous system increases both working pressure and efficiency by wrapping with nonstretch bandage.8 There are few published studies comparing compression bandages with compression stockings for overall use, but one study has shown a greater success with treatment, improved patient acceptance, and reduced complications with stockings compared with bandages.16
Unless periodically rewrapped expertly, compression bandages only maintain significant compression for 6–8 hours while patients are ambulatory and lose up to 50 percent of their initial compression pressure in recumbent patients at 24 hours.17 Due to lack of training in techniques and reduced patient compliance, compression bandaging usually is reserved for patients who simply cannot be fitted with compression stockings. Most of the time, both physicians and patients opt for the most convenience and use compression stockings, even though bandages might work best in a particular clinical situation.
 CLINICAL APPLICATIONS OF COMPRESSION
CLINICAL APPLICATIONS OF COMPRESSION
Prevention and Therapy of Venous Insufficiency
Veins with a high unopposed filling pressure have a tendency to become distended, causing secondary valvular incompetence. If valves are allowed to remain incompetent for prolonged periods of time, fibrosis of the cusps may cause irreversible damage. Bandages and graduated compression stockings provide external support that can constrict dilated veins and restore competence to incompetent valves. To prevent valve fibrosis, external compression is important from the earliest stages of venous insufficiency.
Compression in Pregnancy
The best use of compression hose as preventive therapy is for patients with varicose veins of pregnancy.18,19 When the factors responsible for dilation of pregnancy-induced varicose veins (excessive blood volume, hormonally induced relaxation of the vein wall, etc.) resolve, the veins often return to normal, but after repeated pregnancies, the varicose veins often become permanent. Graduated compression stockings can minimize dilatation of superficial vessels during pregnancy and can maintain valvular competence in many patients, reducing the likelihood of permanent valvular damage. The risk of deep-vein thrombosis (DVT) is also reduced.20
At the first indication of pregnancy, genetically susceptible patients should initially be fitted with 20- to 30-mmHg graduated stockings as thigh highs or panty hose. In multiparous women, or in those with a previous history of varicose veins, stronger 30- to 40-mmHg compression stockings should be worn. In women with large legs or in patients who are too uncomfortable with 30- to 40-mmHg stockings, calf-length 20-to 30-mmHg compression stockings can be worn over 20- to 30-mmHg thigh highs or panty hose. Even 25-mmHg graduated compression stockings can significantly decrease subjective discomfort and ankle edema during the third trimester of pregnancy.21
Compression After Vein Treatments Including Endovenous Ablation
Compression has been used as an adjunct to vein sclerotherapy since the 1940s22,23 and achieved widespread acceptance during the 1950s and 1960s. The addition of compression to sclerotherapy is regarded by many as the most important advance in the treatment of varicose veins since the introduction of the first relatively safe synthetic sclerosing agents in the 1940s. Postsclerotherapy compression reduces the thrombophlebitic reaction and substitutes a “sclerophlebitis”’ with production of a firm fibrous cord.24 Interestingly, compression works to prevent the appearance of new varicose veins even after surgery: regular use of compression can reduce the one-year recurrence rate after surgery from 70 percent to just 7 percent.25 Our experience has shown that three days of compression following endovenous ablation reduces discomfort and enhances closure rate, although comparison data with no compression are lacking. After using compression stockings in over 1000 endovenous ablation patients with the longest follow-up for 10 years, we recommend the use of 30- to 40-mmHg compression stockings worn for three days after the procedure.
Value of Postsclerotherapy Compression
When used after sclerotherapy, compression serves several important functions (Table 15-5). Compression of the treated vessel decreases the amount and extent of thrombus formation after endothelial injury, reducing the likelihood of subsequent recanalization.26 A decrease in thrombus formation also reduces the incidence of postsclerosis pigmentation and helps to minimize inflammation that can lead to telangiectatic matting.27 Compression stockings produce a marked increase in blood flow through the deep venous system and this helps to prevent DVT, whether from direct endothelial injury or from extension of thrombus through perforating veins.28 Immediate compression may produce direct apposition of the treated vein walls to produce more effective wall damage with a smaller concentration of the sclerosing solution. A recent study demonstrates the statistical significantly improved results of 20- to 30-mmHg compression hosiery after sclerotherapy. Significant clinical benefit is shown as well as reduction in hyperpigmentation postsclerotherapy.12 Foam sclerotherapy increases the necessity of compression as foam has a tendency to spread beyond treated sites, which can be minimized by immediately compression. Clearance of foam leaking into the deep system is enhanced by the increased pumping pressure of the deep venous system with compression.
TABLE 15-5
Rationale for Use of Compression Stocking Following Sclerotherapy
1. Decreases risk of recanalization of treated vein by decreasing thrombus
2. Decreases incidence of posttreatment pigmentation by decreasing thrombus
3. Minimizes telangiectatic matting (reducing venous pressure)
4. Improves calf-muscle pump, decreases pooling and side effects such as pigmentation
5. Increases apposition of vein following treatment to promote more sealing and faster resolution of treated veins
6. Keeps foam in treated veins, prevents spread to adjacent normal veins
 AMOUNT OF COMPRESSION
AMOUNT OF COMPRESSION
The amount of pressure needed to fully compress a varicose vein after sclerotherapy depends on the situation. An external pressure of 30 mmHg will produce a 96 percent reduction in the capacity of dorsal foot veins carrying an internal pressure of 50 mmHg.29 Classic compression bandaging produces an average compression of 54 mmHg at the upper calf, and this is sufficient to reduce by 94 percent the size of a vessel that is distended by an internal pressure of 90 mmHg.30
 DURATION OF COMPRESSION
DURATION OF COMPRESSION
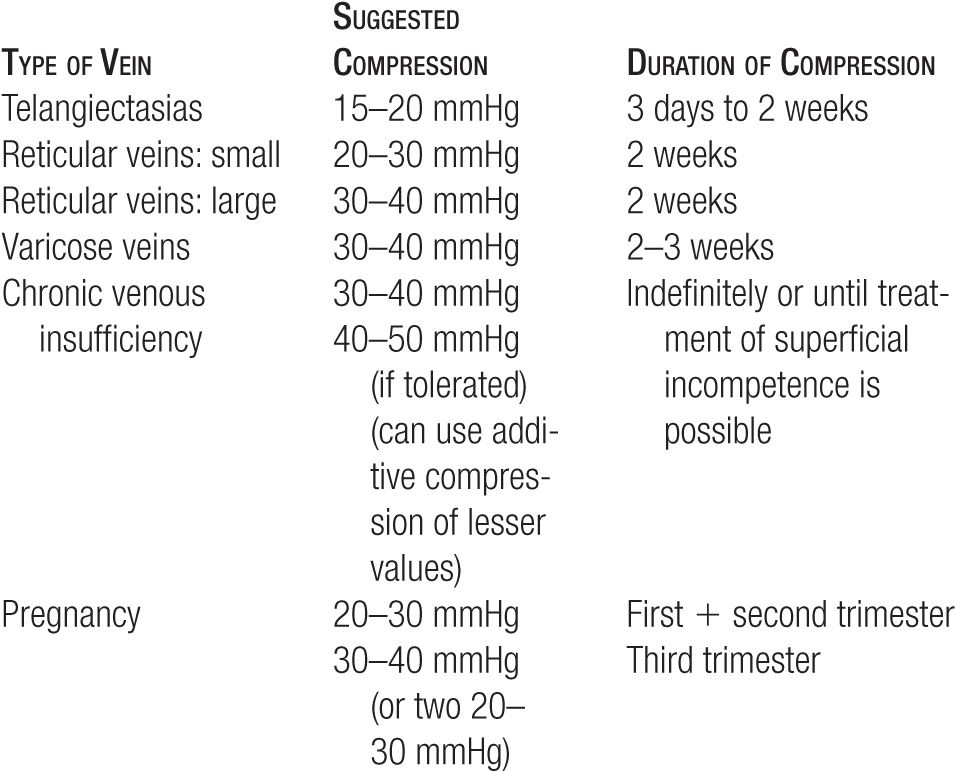
The duration of compression needed after sclerotherapy is still a matter of controversy, although most recommend two to three weeks. The classic descriptions of sclerosis of varicose veins by Fegan, Hobbs, and Doran and White recommend compression for six weeks.23,31,32 A few small randomized studies have suggested that most of the value of compression may come in the early phase, and that results may be comparable, no matter whether compression is maintained for six weeks, for three weeks, or only for three days.33,34 A recent well-controlled study concluded that three weeks of compression may be ideal; however, one week and three days of compression are sufficient to improve results.12 In the United States, few patients can tolerate six weeks of uninterrupted compression, but most are able to comply with two weeks of compression stockings, and nearly all can tolerate a protocol that uses relatively uninterrupted compression for the first three days, then continues compression interrupted only for showering for the next two weeks. Suggested compression pressures and durations for types of veins treated are outlined in Table 15-6.
TABLE 15-6
Guidelines for Use of Compression Stockings After Sclerotherapy and in Clinical Conditions
 COMPRESSION FOR SPIDER VEINS
COMPRESSION FOR SPIDER VEINS
Compression is a well-accepted part of the treatment of large varicose veins, but the use of compression when treating smaller telangiectasia is less widely accepted. In a 1997 survey of European research colleagues, it was found that many did not use any kind of compression after small-vein sclerotherapy.35 However, a multicenter, bilateral comparison study found that three days of compression improved the effectiveness of treatment in telangiectasia greater than 0.5 mm in diameter on the proximal leg and in telangiectasia of any size on the distal leg.36 Compression also reduced the rate of postsclerotherapy hyperpigmentation from 40.5 percent to 28.5 percent and reduced the incidence of posttreatment ankle edema. A study of flight attendants demonstrated statistically significant reduction in symptoms using only over-the-counter (OTC) ready-to-wear panty-hose compression stockings of 12–15 mmHg or 15–20 mmHg.13 We recommend compression for all patients with spider veins to help reduce symptoms of leg fatigue for any flights longer than 1 h. The use of compression may also theoretically reduce the risk of developing in-flight DVT.
We favor compression as adjunctive therapy for all vein sclerotherapy, because the theoretical justification for compression applies equally well to small veins as to large ones, and because a significant percentage of smaller spider veins on the lateral thigh occur in direct communication with larger varicose or reticular superficial veins.37,38 If one treats only minuscule telangiectasias (<0.3 mm) without visualization or treatment of reticular veins, the duration of compression can be reduced to three days without adverse outcome.
 CONTRAINDICATIONS TO COMPRESSION MODALITIES
CONTRAINDICATIONS TO COMPRESSION MODALITIES
Not all patients can tolerate compression stockings, and not all will benefit from them. Patients with edema may benefit more from intermittent therapy than from constant compression. Patients with arterial insufficiency may suffer more from restriction of arterial flow than they benefit from enhancement of venous flow. Patients with unusual anatomy or with severe cutaneous sensitivity may be unable to tolerate placement or removal of a compression garment.
Edema
Marked edema, weeping stasis dermatitis, and new venous leg ulcers will benefit from bandaging or pneumatic compression rather than from compression stockings in the acute phase. When edema of the leg is due to cardiac failure, constant external compression may increase venous return to the detriment of the patient. It is essential to know the entire clinical situation and the cause of leg edema before instituting compression.
Arterial Insufficiency
Arterial insufficiency, although not an absolute contraindication to compression, must be thoroughly evaluated before compression stockings are recommended for any concomitant venous insufficiency. When patients experience leg pain following the application of a stocking, it must be removed immediately and further examination such as Duplex ultrasound must be performed.
It is important to check arterial pulses before and after application of compression bandages or stockings, particularly in older patients. Approximately 21 percent of older patients with venous disease also have decreased arterial pressure.39 Palpable pulses of the posterior tibial and dorsal foot arteries do not exclude increased intracompartmental pressure, because arterial pulsations may be normal at up to 80 mmHg of intracompartmental pressure.40 Sensory disturbances may be the earliest warning sign indicating excessive compression.
Even in normal limbs, arterial flow is diminished at rest, and ankle compression pressures greater than 20 mmHg can impair calf muscle and cutaneous blood flow in bedridden patients.41 When 30- to 40-mmHg compression stockings are worn to bed, some patients may have hypoperfusion-induced discomfort in the foot, heel, and ankle that occurs during sleep and resolves with standing or walking. When double stockings are used to obtain higher compression pressures, patients must be warned to remove the outer stocking when not walking.
Fitting Difficulties
When the ankle diameter is less than 17 cm, it may be difficult to get the correct-size stocking to fit over the wider portions of the foot and heel, and in this case, a lower compression class may be substituted. Elderly patients with less physical strength may require assistance from a visiting nurse. A compromise solution is the use of two stockings of lower compression, one over the other, to have an additive effect. Special stockings with zippers have been developed for use in physically debilitated patients who cannot pull on an ordinary compression stocking.
 HOW TO USE COMPRESSION STOCKINGS Measurement
HOW TO USE COMPRESSION STOCKINGS Measurement
Nearly all stocking manufacturers have adopted the reference table of the GZG (Quality Seal Association for Medical Compression Stockings), which was created in 1972 by the German Association for Phlebology. Measurements of circumference are taken at eight points on the leg using a non-stretchable tape measure and patients are separated into six different sizes (Figure 15-3A). All ready-made stockings include the ankle as one of the measuring points because a graduated stocking exerts 100 percent of its rated pressure here (Figure 15-3B, Point b). Although fitting is primarily based on ankle diameter, a custom-constructed stocking will be required if the other leg measurements are not within one size of the “best fit” as determined at the ankle. Simplified measurement methods use circumferential measurements at the ankle and at the largest diameters of the calf and upper thigh. The length of the leg is measured from the heel to the gluteal fold for panty hose and thigh-high stockings. The length from the heel to the popliteal fossa is used for knee-high stockings. Actual gradient percentages of compression are shown in Figure 15-4.
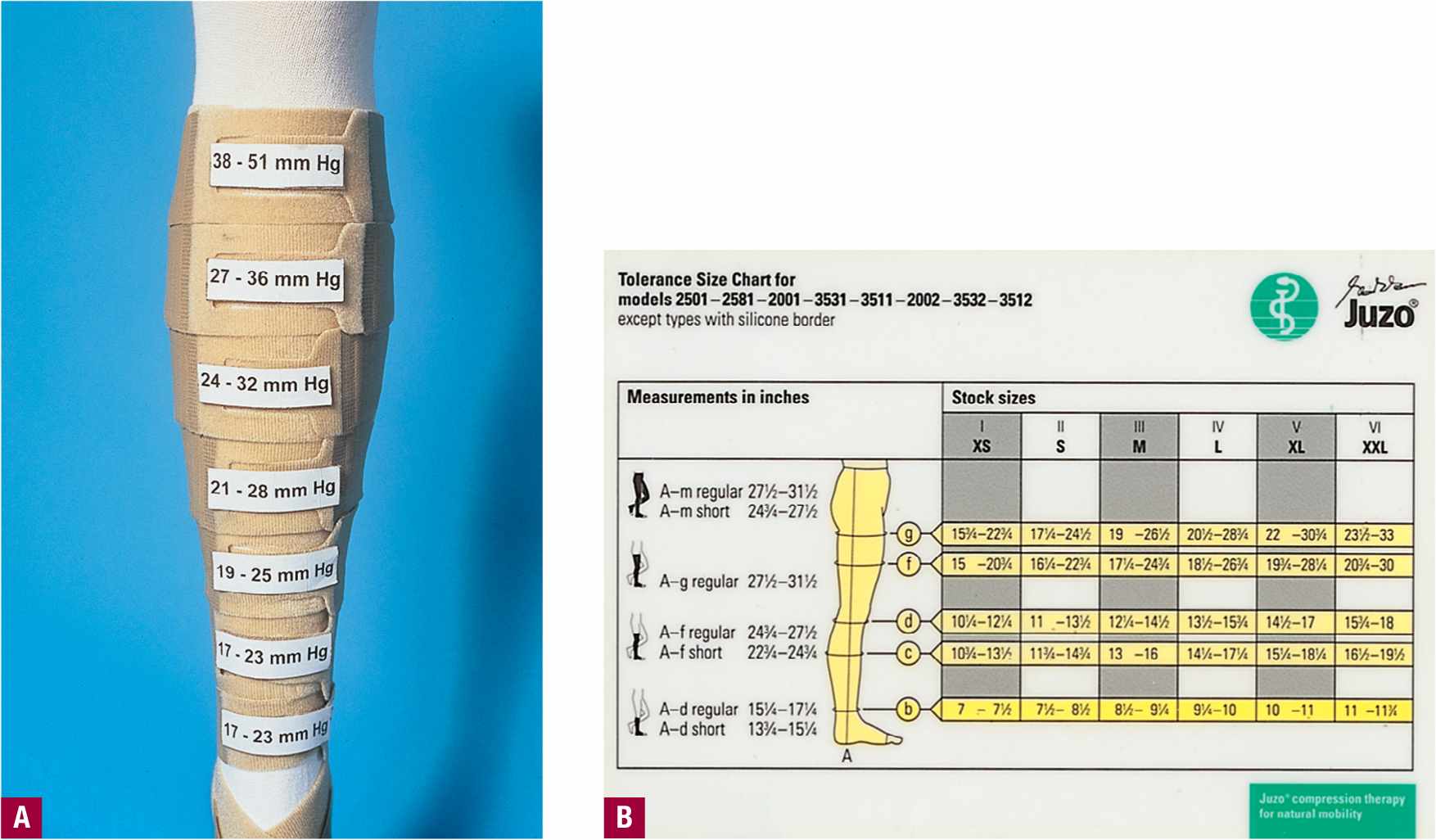
![]() FIGURE 15-3 Important points of measurement for compression stockings. A. Measurements of circumference are taken at eight points on the leg using a non-stretchable tape measure. B. Points to measure for fitting ready made compression hose.
FIGURE 15-3 Important points of measurement for compression stockings. A. Measurements of circumference are taken at eight points on the leg using a non-stretchable tape measure. B. Points to measure for fitting ready made compression hose.
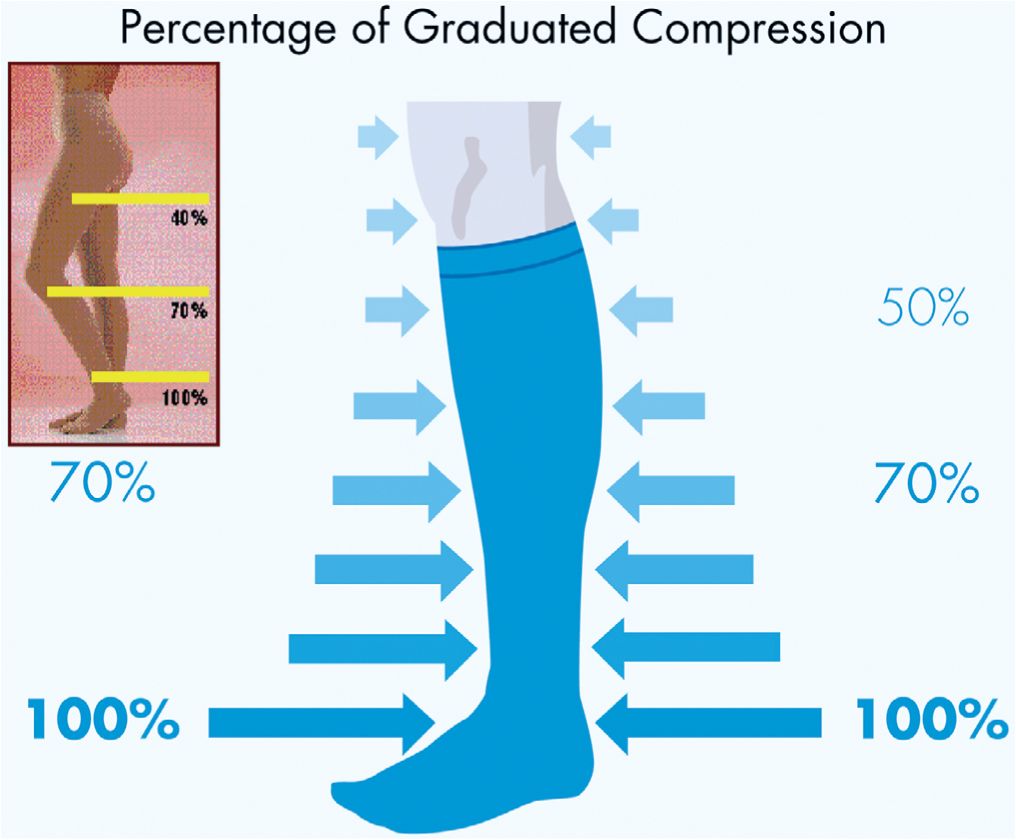
![]() FIGURE 15-4 Schematic of actual gradient percentages of compression stockings.
FIGURE 15-4 Schematic of actual gradient percentages of compression stockings.
To minimize the distorting effects of edema, fittings should be performed in the morning or immediately after the removal of a compression bandage. For lymphedema, the fit will need to be adjusted frequently once the lymph begins to be mobilized. Patients who have a wide foot do not tolerate higher classes of compression, as they often develop nocturnal foot pain if over-compressed. Up to six styles of medical compression stockings are available depending on the manufacturer; knee-, mid-thigh, thigh-high panty hose or leotard; one-legged panty hose; thigh-high with waist attachment; and maternity panty hose. Regardless of the style, most stockings are available in three lengths: knee length, mid-thigh, and thigh length. According to the standardized figure, a knee-length stocking is designated as A D, a mid-thigh stocking as A F, and a thigh-length stocking as A G.
With single-leg, thigh-high, or calf stockings, various inexpensive objects such as adhesive tape, glues, clips, or garter belts serve to ensure proper positioning. Disadvantages of tapes or glues include the pain on removal of tape from hairy legs, and irritation or allergy caused by the adhesive portion of the tape. For some patients, the use of garter belts is a desirable method for ensuring correct positioning of thigh-high stockings. A new type of silicone beaded top band on thigh-high or mid-thigh stockings is now available from some manufacturers, and in some patients, this can prevent slippage without the use of glues, waist straps, or garter belts.
Proper Application Technique
Measures must be taken to avoid poking a hole through the stocking while pulling them onto the leg. Hand jewelry should be removed and fingernails should be smooth and relatively short. Rubber dishwashing gloves or simple nitrile examination gloves are recommended to prevent damage to the stockings from long fingernails and to improve the grip on the stocking. Latex gloves should not be used since it exposes patients to risks of latex allergy such as itching, burning, and urticaria (American Academy of Dermatology publications: http://www.skincarephysicians.com/eczemanet/contact_dermatitis.html) which may be confused with an allergic response to sclerosants. Talcum powder or cellulose powder may be applied to the leg, or a light perlon panty hose or stocking may be worn under the compression stocking to create a smoother leg over which to slide the stocking. Smooth fabric foot “socks” provided by some stocking manufacturers are helpful in getting an open-toe stocking over the ankle. This also helps to avoid damage from abrasive toenails and calluses.
The proper technique for putting on a compression stocking is illustrated in Figure 15-5. After taking the precautions mentioned above, the stocking is turned inside out with the foot portion tucked into the stocking. The foot opening is stretched with the fingers or thumbs of both hands and the stocking is pulled up to the instep. The stocking is drawn upward over the heel until pulling becomes difficult, and a fold that forms across the instep and the heel of the stocking are pulled over the patient’s heel. Finally, the stocking is pulled up in small sections, proceeding only in small steps and taking care to avoid any creases or “bunching up” of the stocking material. It is very helpful for the physician or nurse to instruct and observe the patient wearing the stocking for the first time.
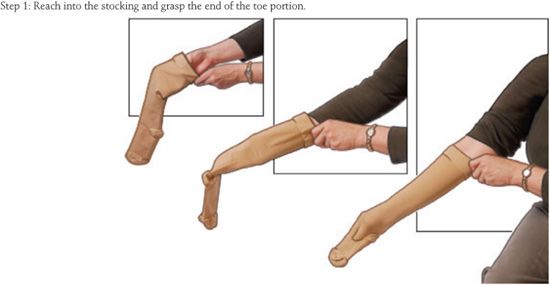
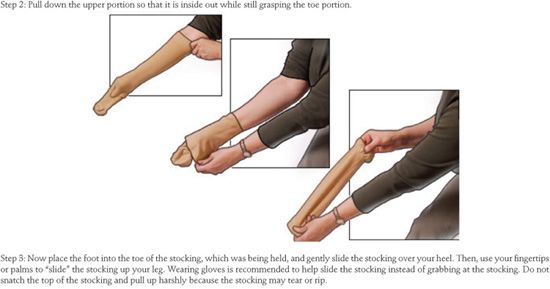
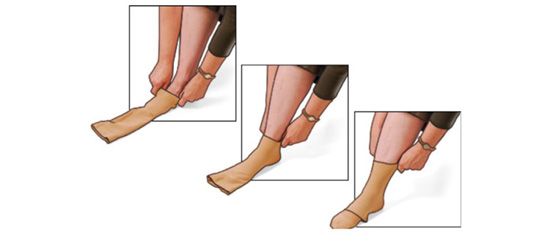
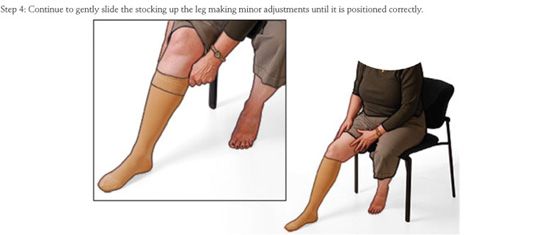
![]() FIGURE 15-5 Schematic diagram illustrating recommended method for application of a compression stocking.
FIGURE 15-5 Schematic diagram illustrating recommended method for application of a compression stocking.
Simple metal frames to aid the application of a stocking are made by various manufacturers (Figure 15-6). The compression stocking is pulled over the half-circle bracket located on the front (open) side of the device so that the heel portion of the stocking is 2–3 inches below the top on the inner-circle bracket. The heel portion is positioned facing the user, and the toe of the stocking is facing toward the open side of the device. The foot is then placed into the foot part of the stocking until the foot is completely on the floor or until the heel is in place. The metal grips on either side are then used to pull the rest of the stocking onto the leg. Once the stocking is above the calf, the metal frame may be pulled away and the remainder of the stocking can then be easily pulled up.
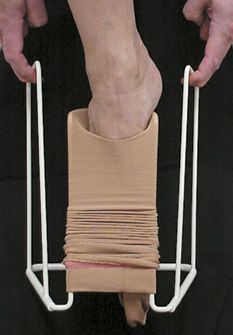
![]() FIGURE 15-6 Open frame to aid in the application of single leg compression stockings (Medi Butler). The compression stocking is loaded into the bracket by stretching over the inner frame. The foot is inserted into the prestretched stocking until it is in contact with the floor. The metal side frame is pulled up which allows the stocking to ride up the leg. The entire frame is then pushed down to release from the stocking.
FIGURE 15-6 Open frame to aid in the application of single leg compression stockings (Medi Butler). The compression stocking is loaded into the bracket by stretching over the inner frame. The foot is inserted into the prestretched stocking until it is in contact with the floor. The metal side frame is pulled up which allows the stocking to ride up the leg. The entire frame is then pushed down to release from the stocking.
 CARE OF COMPRESSION STOCKINGS
CARE OF COMPRESSION STOCKINGS
Chemical stresses from sweat, soaps, creams, and body oils, in addition to the physical stresses of near continuous stretch and relaxation with movement of the leg, result in a relatively rapid decline in the compressive effect of the stockings. Under normal usage and proper care, compression stockings should have an effective lifespan of 4-6 months. Thin nitrile gloves should be worn when the stocking is put on to avoid tearing the threads with fingernails. Likewise, toenails should be trimmed, and hard calluses, verruca, or other rough spots on the feet should be softened or removed. The stocking should not come into contact with ointments, creams, stain removers, or other solvents, especially if it is composed of rubber threads. These substances can damage the fine elastic yarns by causing them to swell and thus can reduce the strength and elasticity of the fabric.
Regular and careful washing is necessary to maintain the elastic properties of the fabric. This is because of the harmful effects of sweat, skin oils, and environmental dirt that accumulate in the fabric while the stocking is worn. Compression stockings may be washed every day using a mild hand-washable soap.22 Whenever possible, the patient should have two pairs that can be alternated between washings. Most compression stockings incorporating Spandex can be machine-washed on a fine/gentle cycle with warm (40°C) water in a mesh laundry bag (consult the manufacturer’s guidelines for specific instructions). Gentle detergents without bleach or alkali are best. Gentle spinning after the washing cycle expedites the drying process. Rather than being hang-dried from a line, compression stockings should be laid flat on a drying rack or towel to help maintain shape. Heat drying will cause a rapid loss of elasticity.
 SUMMARY
SUMMARY
Compression serves many important purposes in patients with venous insufficiency syndromes. Compression is extremely valuable as adjunctive therapy after endovenous ablation or sclerotherapy for leg veins of all sizes. Compression alone serves as primary conservative therapy for patients with otherwise untreatable deep system insufficiency and for those with superficial insufficiency who cannot undergo ablation or other treatment of the superficial sources of reflux. Compression is an important method of prevention in pregnancy and other high-risk settings. Perhaps the most valuable role of compression is as a form of prophylaxis against DVT. It is a rare patient (usually with confounding arterial insufficiency) who will not benefit in some way from compression as part of a treatment for venous insufficiency.
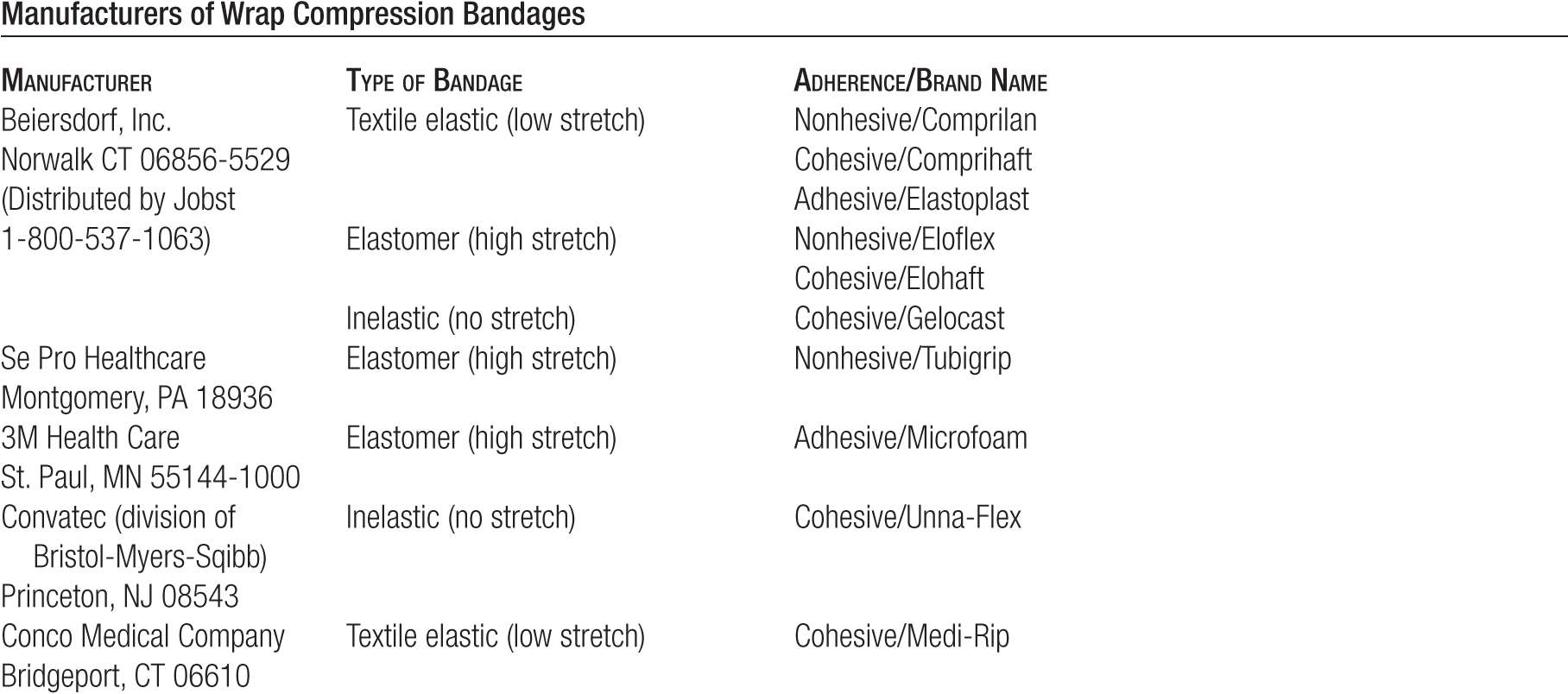
Sample instructions for patients are listed in Figures 15-7, 15-8, 15-9, and 15-10. A list of compression stocking and compression bandaging manufacturers is provided in Table 15-7A and 15-7B (see also Chapter 25). Popular websites for patients to order compression stockings include www.foryourlegs.com, and www.compressionstockings.com
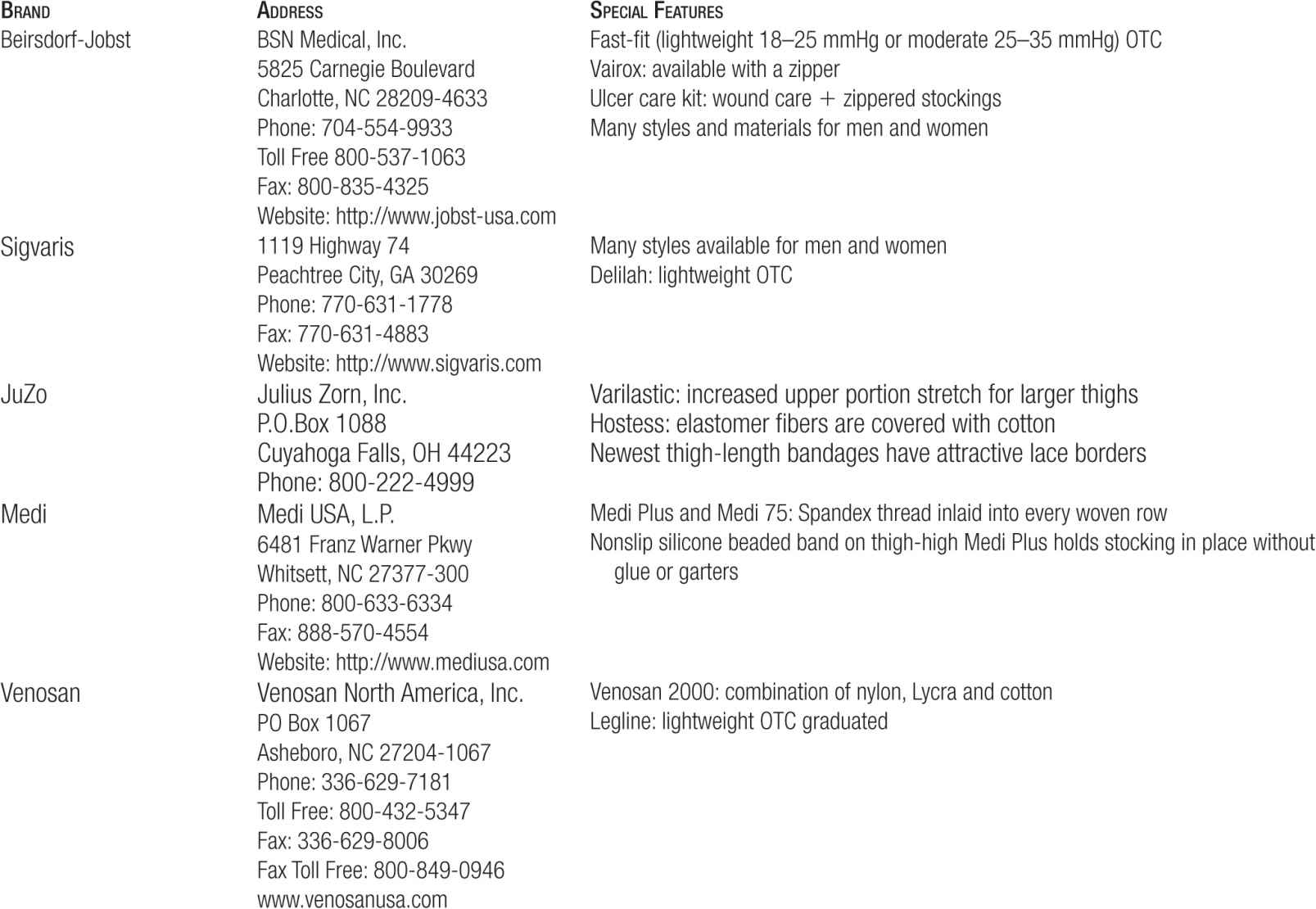
TABLE 15-7
Manufacturers of Compression Stockings (Limited List)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


