Common Congenital Hand Anomalies
Robert J. Havlik
Congenital anomalies of the hand and upper extremity constitute one of the most frequent disorders that afflict newborn children. The cumulative incidence is often underappreciated because of the large variety of anomalies. Although the exact incidence is difficult to establish because of methodology issues, variability in reporting, and also the racial variations of the individual disorders, the most commonly occurring congenital anomalies of the upper limb are polydactyly, syndactyly, and camptodactyly. To frame this discussion, it is important to remember that approximately 95% of all pregnancies carried to term are “normal.” Overall, the incidence of syndactyly is estimated to be approximately 1 in 2,000 births.1,2,3 In England and Wales, where detailed population-based comprehensive health statistics are available, the incidence of syndactyly has been established as 1 in 2,400 births.4 Polydactyly shows considerable racial variation and is autosomal dominant in many African Americans. However, if one assumes a relatively similar incidence of syndactyly, camptodactyly, and polydactyly across the broader population, then the combined incidence of these three congenital anomalies of the upper limb would be approximately 1 in 750 births. This places the combined incidence of congenital upper limb anomalies within the same range as that of the most common major congenital anomaly—orofacial clefting, which has an incidence of approximately 1 in 700 births.5 The more complex congenital hand anomalies are less frequent. As a point of reference, Apert syndrome, one of the less frequent anomalies, has an approximate incidence of approximately 1 in 100,000 births. Expanding this incidence figure to the birth rate of the United States, with 4 million births per year, there would only be expected to be 40 children born per year with Apert syndrome in the entire United States.
Optimal management of the child with a congenital anomaly of the hand is a challenging undertaking. Unlike the adult patient, the child is not able to effectively communicate or participate in an examination. The planning for operative treatment must be communicated with the parents. The surgeon must recognize that there is a burden on the family to take time off of work and accompany the child to office visits and the hospital, and therefore should try to maximize clinical progress with each visit. Operative care can be challenging from several perspectives. Appropriate anesthesiology expertise must be available. Of course, one of the most challenging aspects of the more complex hand anomalies is that the anatomy can be, and is often, atypical. A complete and thorough understanding of “normal” anatomy is essential before undertaking the more complex congenital cases. Postoperative care can potentially be limited by noncompliance, both on the part of the child and also by his/her family. Particular care and attention is paid to the postoperative dressing because it can be dislodged. Despite these considerations, the management of congenital hand anomalies represents one of the most gratifying experiences for hand surgeons.
Detailed classification criteria have been developed for congenital hand anomalies. Perhaps, the most recognized comprehensive classification is that developed by the International Federation of Societies for Surgery of the Hand (IFSSH). The IFSSH classification classifies congenital hand anomalies based upon seven categories: (1) failure of formation; (2) failure of differentiation; (3) polydactyly; (4) overgrowth; (5) undergrowth; (6) amniotic band syndrome; and (7) generalized skeletal syndromes.6 The fine details of this classification lie outside the scope of this chapter, but the classification is useful for clarity in communication. The focus of this chapter is upon diagnosis and management of the common congenital anomalies of the hand.
EXAMINATION
Examination of the child’s hand requires some special considerations. The examination is one component of a comprehensive examination, including the torso, head and neck, and lower extremities. Often, the hand surgeon will be the first to recognize important findings that can have significant implications for the child’s overall growth and development. Examination includes a catalog of all components of the upper extremity, from torso to fingertips. Specific attention should be directed toward the musculature of the torso and upper extremities, and to the size of the upper extremity relative to the contralateral side. Passive range of motion is carefully assessed over a full range of motion of the entire upper extremity. Often, this requires that the child be distracted in some manner to accomplish a detailed examination. Although the child may not be able to follow directions, careful examination should be made for the presence or absence of digital flexion and extension creases on the hand and upper extremity. Absence of these creases indicates the absence of motion, which can be secondary to joint, tendon, or neuromuscular anomalies. If the surgeon has questions about the extent of innervation of the hand, the hand can be immersed in lukewarm water for 10 to 15 minutes to assess for “pseudomotor activity,” manifested as wrinkling of the skin over the digital fingertips (Figure 89.1). This can provide significant information regarding digital innervation and denervation.
EMBRYOLOGY OF THE HAND
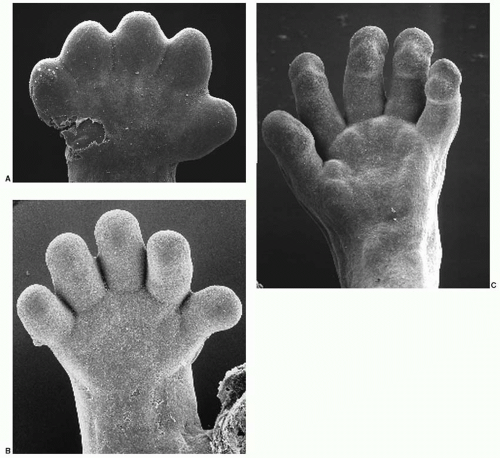
In “normal” development, the hand “plate” develops between the fifth and eighth weeks of intrauterine growth.7,8,9 Hand development is largely driven by concentration gradients of growth factors in local tissues. The hand “plate” develops five ridges through the process of apoptosis, or programmed cell death, between the ridges at 48 days of gestational age.7,9 The process of apoptosis starts distally and progresses proximally. An elegant series of micrographs by Sulik has elucidated this process (Figure 89.2). Digital separation is completed by 51 days of intrauterine age. During the time of digital separation, the ridges undergo progressive proliferation of the mesenchymal tissue, and by 56 days of gestational age, the digits have undergone segmentation and the development of “touch pads.” The appearance of the hand has largely been defined between 48 to 56 days of gestational growth. The failure of apoptosis to occur leads to the occurrence of syndactyly. This pattern of morphogenesis accounts for the relatively low occurrence of thumb-index finger syndactyly, because the first ray is known to separate early in the sequence of differentiation of the hand.
SYNDACTYLY
Syndactyly is derived from the Greek “syn”—meaning together, and “dactylos”—meaning digits. As noted above, the incidence of syndactyly is approximately 1 in 2,000 live births. Syndactyly occurs approximately twice as frequently in males as in females. The most frequently afflicted web space is the long-ring web in the hand, and the second-third toe web in the foot. The long finger-ring finger web space accounts for approximately 50% of all cases of syndactyly,3 whereas the ring finger-little finger syndactyly accounts for approximately 30%, the index finger-long finger syndactyly about 10%, and the thumb-index finger fusion is relatively rare and accounts for only 5% of all cases of syndactyly.1 The majority of syndactyly cases present as isolated occurrences, but 10% to 40% of cases are familial in origin, depending on the series.1 All patterns of genetic inheritance have been postulated based upon pedigree analysis, but the most common pattern seems to be autosomal dominant inheritance with incomplete penetrance.2 Syndactyly is classified by many schemes, but the most direct description classifies syndactyly as complete (extending through the finger
tips) or incomplete (extending only partially along the length of the digit), and simple (soft tissue only) or complex (bone or joint fusion).
tips) or incomplete (extending only partially along the length of the digit), and simple (soft tissue only) or complex (bone or joint fusion).
Depending upon the location within the hand, syndactyly may cause little functional impairment or may cause severe impairment with growth disturbance. The most common syndactyly, with long finger-ring finger involvement, shows little impact on growth because of the similarity in length of the mature digits. In contrast, involvement of the border digits (ring-little or long-index) can cause significant impact on growth, and the uncommon thumb-index fusion causes both severe functional and growth disturbance. Developmentally, the abilities to establish the position of the thumb in space (a cortical function) and to grasp are established by 1 year of age, with further refinement of skills occurring up to 3 years of age.10 Therefore, in cases with thumb-index fusion, separation should be accomplished before 6 months of age. Those cases with involvement of the border digits also require earlier separation because of the inherent length discrepancy of the long-index and ring-little fingers, and the potential for growth disturbance of the afflicted digits. The tethering can cause angular deformity of the longer digit. These digits should certainly be separated by 6 to 9 months of age. Complex syndactyly that involves bony fusion should also be separated by 6 to 9 months of age to prevent growth irregularities. In complex syndactyly with multiple digits involved, such as Apert syndrome, there exists a therapeutic imperative to plan a sequence of operations for completion of digital separation early in life. The timing for surgical release should recognize that maintaining a dressing on the upper extremity to protect the surgical site can become challenging after 12 to 18 months of age.
Surgical planning for separation of syndactyly must observe the three primary goals of hand surgery: (1) enable the patient to position the hand and fingers in space; (2) provide adequate and sensate skin cover; and (3) provide a satisfactory power grasp with the ability to handle objects precisely.1 In the surgical correction of syndactyly, there exist six primary tenets that are observed to obtain these goals: (1) complete separation of all osseous and soft tissue; (2) optimal preservation of both nerves and blood supply; (3) the development of an adequate web space between the digits through the use of an appropriate flap(s) inset without tension; (4) interdigitating flap coverage over the proximal interphalangeal (PIP) joint; (5) development of appropriate distal phalanges and finger tips; and (6) the use of perforated full-thickness grafts for digital resurfacing to minimize the effects of secondary contractures.
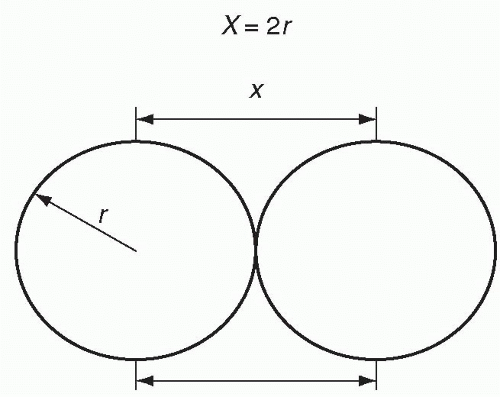
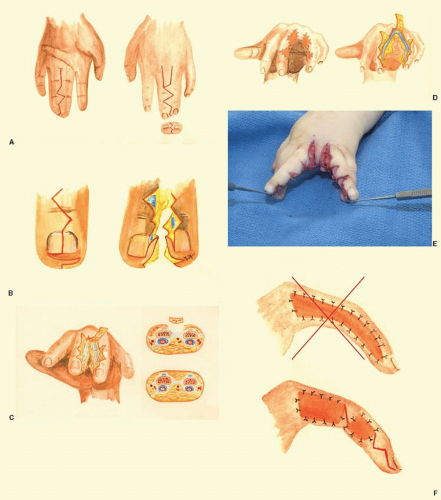
In separating the digits, it is generally accepted that for reasons of vascular safety, only one side of a digit should be separated at any given operative procedure. All skin must be meticulously preserved and utilized, but it must also be recognized that skin grafting will be necessary, because there is always a definite deficiency of skin (Figure 89.3). A flap(s) must be created for web space resurfacing, as it provides superior characteristics in terms of healing and suppleness in the web space compared with grafting, which is reserved for shorter segments overlying bony phalanges. One of the most widely used techniques is that using a dorsal skin flap, which was first described by the Indiana plastic surgeons Bauer, Tondra, and Trusler.11 The dorsal flap is designed to extend two-thirds of the distance from the metacarpal heads to the PIP joint (Figure 89.4A). Following this, the second step is designing triangular flaps to cover the PIP joints and break up the grafted area on the lateral finger surface to smaller areas. These flaps provide a more favorable aesthetic result if the dorsal flap is based on the ulnar digit, and the palmar flap is based on the radial digit. Once these PIP flaps are designed, the adjacent triangular flaps extending proximally and distally on both the palmar and dorsal surfaces can be designed (Figure 89.4A). Interdigitating flaps are designed and elevated from the finger tips to create the paronychial folds, as described by Buck-Gramcko12 (Figure 89.4B). The dorsal flap is then elevated en bloc with the underlying fat off of the conjoined Cleland’s ligaments (Figure 89.4C). These ligaments normally provide points of attachment for the lateral digital skin to the bony phalanx, but in syndactyly these ligaments are conjoined. The neurovascular bundles lie palmar to these conjoined ligaments. Following elevation of the dorsal web space flap, the distal dorsal skin flaps are incised and elevated. Once these dorsal flaps are elevated, the conjoined Cleland ligaments can be isolated through limited blunt dissection, freeing the digital neurovascular bundles off of the palmar surface of the conjoined ligaments, and the ligaments cut under direct vision with scissors. The neurovascular bundles are identified and preserved. Following division of Cleland ligaments, the palmar flaps are incised (Figure 89.4D). If there is a distal bifurcation of the blood supply, a microvascular clamp should be applied to assess digital perfusion before any vessel is divided. The tourniquet is released at this point to assess perfusion, so all steps requiring a bloodless field should be completed prior to tourniquet release. If there is no distal bifurcation of the vessels, the palmar skin incisions can be made, preserving the underlying neurovascular bundles. Nerves can be “teased” apart bluntly as indicated. Following digital separation, flaps are transposed and sewn in place, making sure that the inset is not too tight to limit perfusion. If this happens, the flaps are recessed to allow for improved perfusion and larger areas will need to be grafted. The goal is to provide flap coverage in the web space and over the PIP joint. Flap coverage over the PIP joint provides more supple coverage and avoids large sheets of grafted skin that are prone to graft loss (Figure 89.4E, F). Templates can be fashioned and full-thickness grafts harvested from an appropriate site (groin, lower abdominal wall, etc.). The grafts are defatted to the dermal layer, perforated, and then sewn in place. Interrupted sutures allow serum and blood to drain from beneath the graft. Appropriate dressings are meticulously placed and consist of bridal veil (Interface, Dermanet, etc.) with petrolatum, followed by petrolatum-laden gauze (Vaseline gauze or Xeroform gauze) and then cotton batten. A light gauze wrap, or a formal tie-over bolster, is then placed to anchor the web space dressing in place. Next, immobilization of the digits, hand, and extremity is performed. In infants, this can include either a “soft cast” or a long arm cast with the elbow maintained in 90° of flexion to prevent dislodgement. The dressing should be placed with the understanding that if it becomes dislodged, it often requires a return to the operating room under general anesthesia to appropriately replace the dressing and minimize the chance of graft loss. Effective immobilization is crucial to successful graft “take” and survival, which in turn is crucial to the success of the operation. Loss of the graft can lead to distal migration of the web space due to cicatricial contracture of the digit.
APERT SYNDROME: ACROCEPHALOSYNDACTYLY
Comprehensive treatment of the hand anomalies of Apert syndrome is beyond the scope of this chapter. Apert syndrome consists of both craniofacial and hand anomalies and is associated with a disturbance in the cell surface receptor for fibroblastic growth factor13 (Chapter 23). Hand involvement varies in severity, but has been characterized into three discrete types: (1) type I—obstetrician’s or Spade hand, in which the four fingers are fused and the thumb is largely free; (2) type 2—mitten or spoon hand, in which the thumb is
typically joined to the thumb mass by a simple syndactyly; and type 3—rosebud or hoof hand, in which the thumb is joined as a tight osseous or cartilaginous fusion of the thumb to the finger mass.13 Apert is a complex anomaly, with abnormal bones, nerves, joints, and tendons, and represents the severe end of the syndactyly spectrum.
typically joined to the thumb mass by a simple syndactyly; and type 3—rosebud or hoof hand, in which the thumb is joined as a tight osseous or cartilaginous fusion of the thumb to the finger mass.13 Apert is a complex anomaly, with abnormal bones, nerves, joints, and tendons, and represents the severe end of the syndactyly spectrum.
SYMBRACHYDACTYLY
Symbrachydactyly is a frequent component of Poland syndrome, an uncommon deformity of the hand, upper extremity, and chest wall seen in approximately 1 in 25,000 births.14,15 The chest wall deformity includes an absence of the sternal head of the pectoralis major muscle, with preservation of the clavicular head.16,17 In addition, there can be other rib and muscular abnormalities present. In females, there is a hypoplasia or an absence of development of the breast. The severity is variable. The hand can be relatively normal, but is frequently characterized by shortened hypoplastic digits with soft tissue fusion between them. The thumb is frequently involved and may demonstrate syndactyly or a constrained first web space.12 Surgical treatment of these digits requires special considerations. First, if the digits are very hypoplastic, they may be unstable, and separation may not produce significant gain and may actually be a detriment until the child is slightly older and the hand has grown further. Second, the digital neurovascular bundles may divide distally, and this must be taken into consideration in operative planning. Finally, these considerations do not generally apply to the first web space syndactyly/constrained web in symbrachydactyly, and so this surgery should be released and resurfaced earlier.
POLYDACTYLY
Polydactyly, or the presence of an extra digit, is one of the most common congenital anomalies of the hand, with an incidence of approximately 1 in 1,000 births. Polydactyly can occur on either the radial side of the hand (preaxial) involving duplication of thumb, central polydactyly involving any of the central three rays, or polydactyly involving the ulnar side of the hand (postaxial polydactyly).
Preaxial polydactyly, or duplication of the thumb, is classified according to the Wassel classification system.18 In this system, the number of the duplication corresponds to the axial level of the duplication. A Wassel type I duplication involves the distal phalanx (Figure 89.5); a Wassel type II classification involves the interphalangeal joint and distal phalanx; a Wassel type III involves the proximal and distal phalanges; a Wassel type IV involves duplication at the metacarpophalangeal (MCP) joint level and the proximal and distal phalanges, a type V involves duplication at the metacarpal level and the proximal and distal phalanges; and a type VI thumb has two separate metacarpals with articulating phalanges—Wassel even numbers involve duplication at the joints and odd numbers involve duplications at a level of conjoined bone, physis, or epiphysis. Most thumb duplications are symmetrical, and in these cases, the surgeon will generally try and preserve the ulnar thumb, thereby preserving stable ulnar collateral ligaments for pinch against the index finger. This decision regarding which digit to preserve must also consider the integrity of the flexor and extensor systems, as this may alter the decision. Surgery may also involve tendon and musculotendinous realignment. In most cases of surgical correction, the radial collateral ligaments are maintained on a proximally based flap of periosteum and secured to the radial aspect of the retained ulnar distal segment. In duplications at the Wassel type IV level and higher, the thenar musculature is advanced and attached to the radial side of the proximal phalanx as well. In some cases of duplication at the Wassel IV level, there may be a pollex abductus deformity present, with fusion of the extensor and flexor tendons on the radial side of the retained ulnar thumb, necessitating release and realignment of these tendons for optimal function. The surgeon must be aware of this possibility and carefully inspect the anatomy of the flexor and extensor tendons prior to deletion of a digit. As noted previously, it is essential to establish the integrity of the flexor and extensor systems prior to deciding which digit to ablate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree