Clinical Manifestation
Morphology of Hidradenitis Suppurativa Lesions
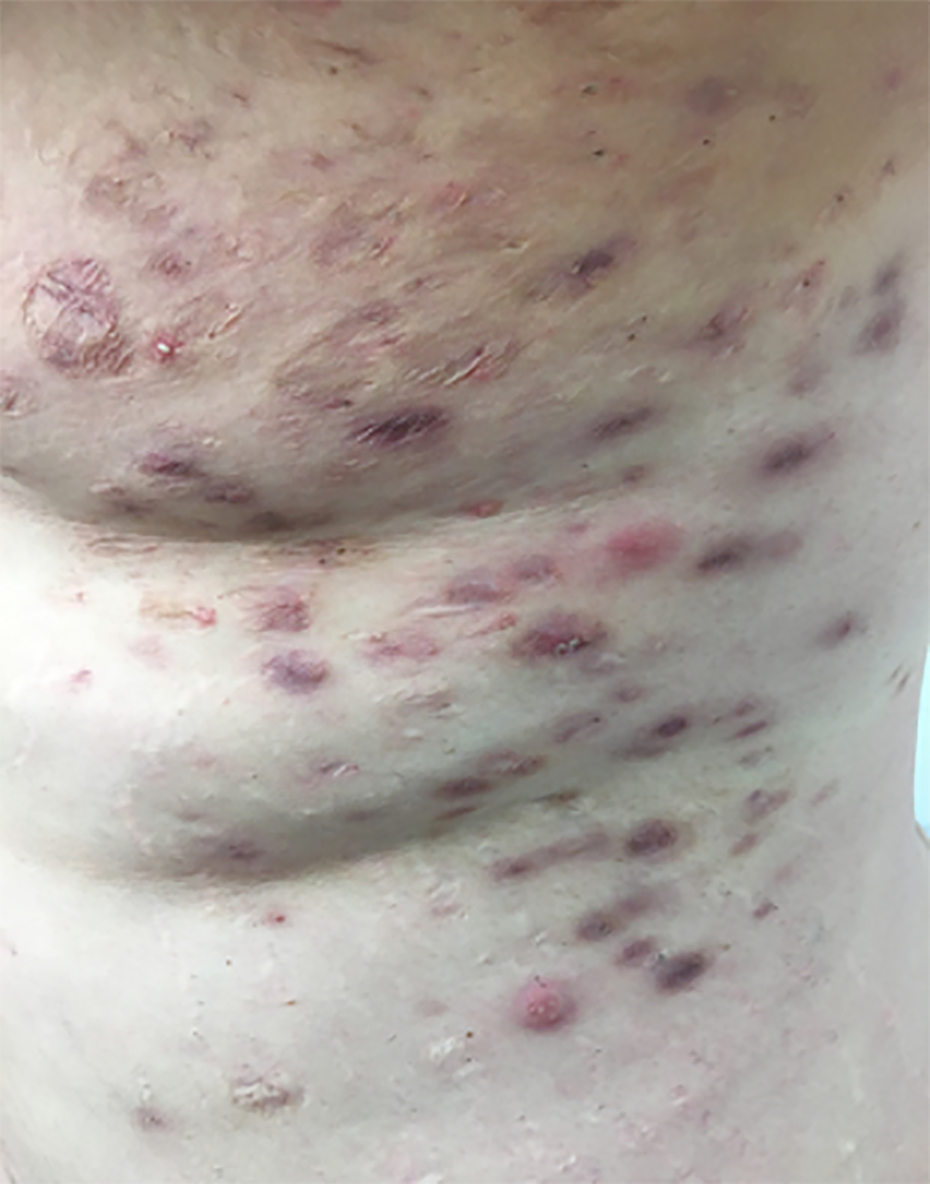
A key component of the diagnosis of an individual with hidradenitis suppurativa (HS) involves examining for the presence of typical HS morphology. The quantity and location of lesions indicate the severity of HS. It is important to consider the possibility of multiple lesion types coexisting simultaneously, together contributing to the severity of HS. Certain lesions (e.g., open comedones, small atrophic scars) suggest quiescent disease, while others (e.g., inflammatory papules, nodules) indicate active inflammation. Additionally, recent research has shown that tunnels (described below) are immunologically active. This chapter will provide an in-depth look at common HS lesions including inflammatory nodules, cysts, abscesses, comedones, draining tunnels or sinus tracts, scars, and several others ( Fig. 3.1 ).
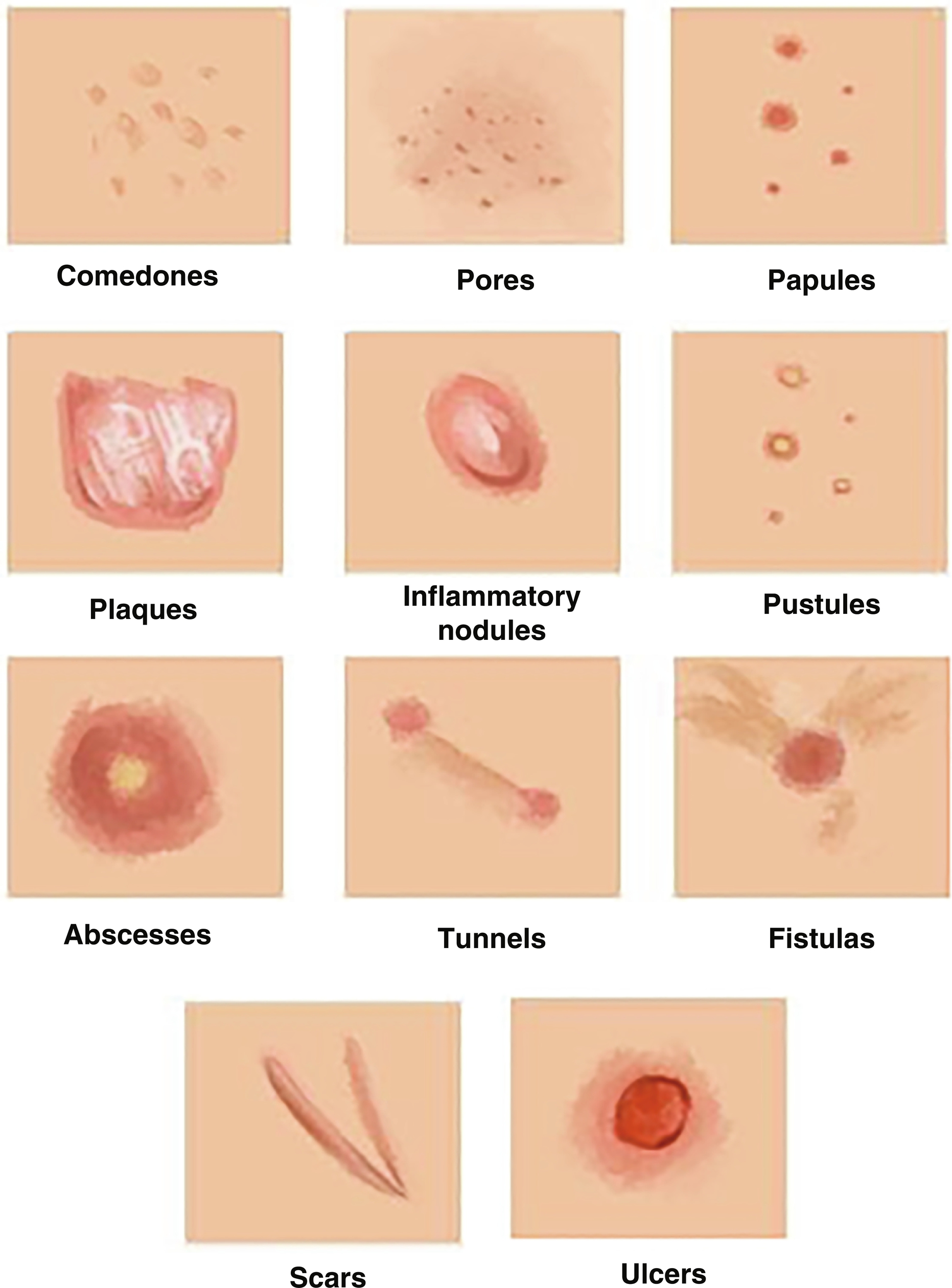
Comedones ( Fig. 3.2 ): Comedones are the skin-colored, small bumps representing dilated hair infundibulum with oxidized black or white keratinous debris (open comedones). There are two main types of comedones: blackheads, due to the oxidation of the pigment melanin; and whiteheads, in which the hair follicle is completely clogged and covered by a thin upper layer of stratum corneum, inhibiting exposure to air (hence the alternate name of “closed”). Double-ended comedones are characteristic for HS, most likely resulting from the keratinization of the residual stump of two adjacent follicles undergoing cicatricial rearrangements ( Fig. 3.3 ).


Pores: Pores are normally 1-mm wide dots that appear on the surface of the skin to indicate the opening of hair follicles. Each hair follicle contains a sebaceous and apocrine gland, which produces the skin’s oils and sweat, respectively. When these pores become clogged and full of debris, they become comedones. The dilation of pores may facilitate the accumulation of debris, giving rise to comedones.
Papules ( Fig. 3.4 ): Papules are small, raised cutaneous lesions. They often present as numerous, firm, typically non-scaly lesions, smaller than 1 cm in size. Papules can be the same color as the surrounding skin, yellow-brown, red-brown, or purple-brown, depending on the patient’s skin color phenotype. They arise when clogging in a pore causes inflammation of a hair follicle.

Nodules ( Fig. 3.5 ): Inflammatory nodules are one of the first defining characteristics of HS and probably the most characteristic lesion of HS. These tender, deep-seated, rounded lesions more than 1 cm last a mean duration of 7 to 15 days. Patients with inflammatory nodules usually report a burning or stinging sensation, pain, pruritus, a warm feeling, and/or tenderness. Over time, the nodules may rupture, erode, and ulcerate, resulting in painful draining or non-draining tunnels.
Plaques ( Fig. 3.6 ): Plaques in HS are elevated, solid, indurated lesions. Plaques may be flat topped or rounded and may have a cribriform-like surface. They are typically more than 1 cm in diameter and may or may not have defined borders. Plaques can take on many different shapes including circular (round), linear, and polygonal (not geometric).

Pustules ( Fig. 3.7 ): Pustules are superficial pus-filled lesions ≤ 1 cm. They are collections of neutrophils located superficially, usually just below the stratum corneum or in a hair follicle. The pus contents can indicate the presence of an infection or can be sterile inflammation, with the latter commonly seen in HS patients.

Abscesses ( Fig. 3.8 ): An abscess, or a boil, is a fluctuant, commonly painful lesion that appears within or below the skin’s surface. The abscess is usually full of pus, or dead white blood cells. The surrounding erythema is a result of increased blood flow to the area of the abscess as part of the body’s immune response to fight infection or inflammation. If left untreated, they can open and lead to a draining lesion. Without proper application of coverings, this presents as an infection-prone site where environmental pathogens may enter freely and inflict more infection.

Tunnels or tracts ( Figs. 3.9 and 3.10 ): A tunnel or sinus tract is a linear connection that forms beneath the epidermis connecting two sites and may open to the skin surface: skin to skin (both sides open), blunted tunnel (one side open to skin), and closed tunnel (not open to skin). They often contain pus and other bodily fluids rich in bacteria that can aggravate the pain, itchiness, and inflammation associated with HS. They often occur in the later stages of HS and commonly contain biofilms. These tunnels are usually treated by deroofing the tunnel and debriding the base to remove the gelatinous tissue, or by complete surgical excision. Tunnels/tracts are also immunologically active, with a study by Jorgensen et al. demonstrating their immunological profile consisting of increased levels of matrix metalloproteases and tumor necrosis factor (TNF)-positive cells.


Scars ( Figs. 3.11 to 3.14 ): Irreversible tissue damage commonly associated with retraction. The progression of HS is often indicated by significant scarring that could be cordlike, hypertrophic, keloidal, atrophic, or cerebriform. In many cases, scarring and active lesions are mixed and connected.




Ulcers ( Fig. 3.15 ): Skin ulcers are open wounds that develop on the skin following an injury, poor circulation, and pressure. The poor blood flow delays healing of the injured epidermis and dermis. They differ from erosions in that erosions only involve the superficial epidermis, whereas ulcers have full thickness, impacting the dermis as well. Knife-like ulcers, also known as fissures, are characteristic of Crohn’s disease that can sometimes be present in HS patients without underlying irritable bowel disease (IBD).

Fistulae: Fistulae are tunnels extending from skin to a hollow organ such as rectum, bladder, or vagina. .
Another key feature of HS lesions is their heterogeneity, which can lead to a range of clinical presentations. Recently, clinicians have begun stratifying patients into subtypes to better classify and study HS. The most currently used subtype classification goes by the body structure affected: axillary-mammary, follicular, and gluteal. This classification system was implemented to study any correlation between genotype and phenotype, if one exists.
Primary lesions versus secondary lesions: Primary lesions occur simultaneously with the onset of disease, while secondary lesions occur as a disease progresses and is often are the result of certain treatments. There are ongoing debates regarding the classification of HS lesions in that some are primary lesions (such as comedones and nodules), while secondary lesions include scars and ulceration.
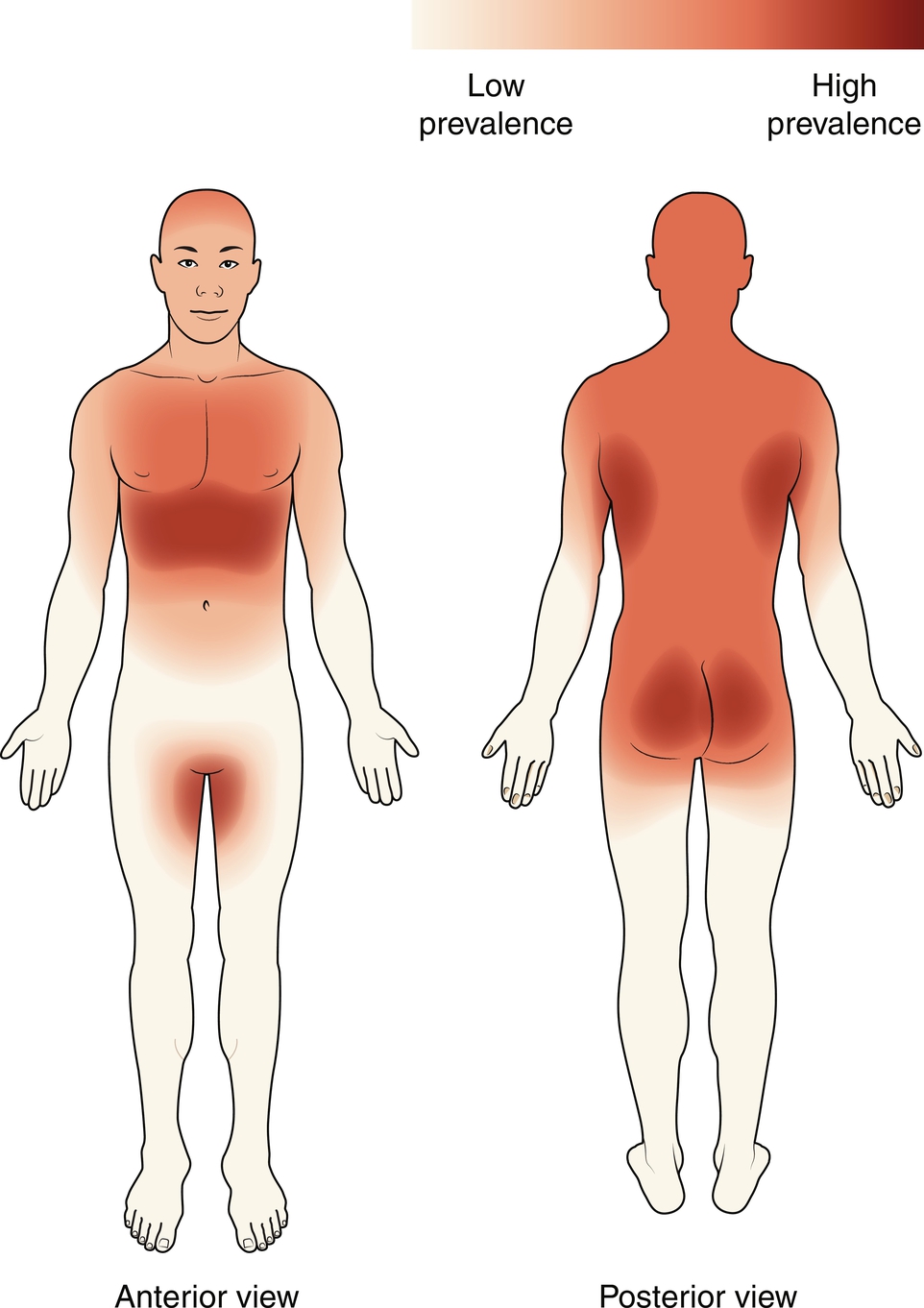
Common Locations
HS typically affects the areas of the body where skin touches skin and areas of skin rich in apocrine glands. These include the axilla, groin, buttocks, and others, which are described below ( Fig. 3.16 ). Furthermore, in females, the most commonly impacted areas are the groin (56.9%), axilla (44.8%), and under the breasts (25.9%). In males, the most commonly impacted areas are the groin (43.3%), anal region (36.7%), and axilla (30%).