Chronic bullous disease of childhood (CBDC) is the most common acquired autoimmune blistering disorder of childhood and is characterized by linear IgA staining of the basement membrane zone on direct immunofluorescence. This autoimmune attack on structural proteins, usually proteolytic fragments of collagen XVII, renders the dermal-epidermal junction prone to blistering. Diagnosis is confirmed by characteristic histology and direct immunofluorescence. Prognosis is generally favorable, with spontaneous remission usually occurring by puberty; however, cases with severe morbidity and cases persisting into adulthood have been reported. This article discusses the clinical features, diagnosis, and pathogenesis of CBDC in more detail.
Chronic bullous disease of childhood (CBDC) is a nonfamilial, autoimmune blistering disease that occurs in prepubertal children and is characterized by linear IgA staining of the basement membrane zone (BMZ) on direct immunofluorescence. The condition has been recognized since the late nineteenth century, when it was initially thought to be a variant of dermatitis herpetiformis (DH). CBDC was recognized as clinically distinct from DH by Kim and Winkelmann in 1961 and ultimately differentiated as a unique disorder in 1970 by Jordon and colleagues who proposed the term benign chronic bullous dermatosis of childhood. In 1988, CBDC was recognized as the childhood counterpart of the adult linear IgA disease. The historical confusion regarding the distinction of CBDC is reflected in the nomenclature. The terms bullous DH, juvenile DH, bullous pemphigoid of childhood, and linear IgA dermatosis of childhood have been used to describe the entity now known as CBDC.
Disease presentation
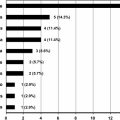
CBDC is the most common acquired autoimmune blistering disorder of childhood, and it occurs without preference to race or gender. CBDC is often initially diagnosed as bullous impetigo and may even temporarily improve with the brief course of antibiotics prescribed by the primary provider. It is when the eruption recurs or persists that the initial diagnosis of bullous impetigo is questioned. Disease onset usually occurs at the age of 6 months to 10 years with a mean age of 4.5 years. However, disease onset has been reported as early as within 24 to 48 hours after birth and up to the age of 12 years. Children present with the abrupt onset of tense, clear, or hemorrhagic vesicles and bullae on normal or erythematous skin. New lesions often arise around resolving lesions, and these arciform or annular bullae surrounding a central crust have been described as a string of pearls, cluster of jewels, or rosette pattern ( Fig. 1 ). The eruption occurs on the face, trunk, and extremities. There is a predilection for the lower trunk, genital area, and medial thighs; disease onset in the perineum has been mistaken for sexual abuse. On the face, lesions tend to occur in a perioral pattern. Younger children more often have the classic distribution of facial and perineal lesions, whereas older children are more likely to present with a generalized eruption ( Fig. 2 ). Mucous membranes may be involved, and the severity ranges from mild oral ulcers to severe oral and conjunctival disease. Clinical symptoms are variable, ranging from asymptomatic to severe pruritus, sometimes with a burning sensation. The disease generally remits spontaneously several months to 4 years after onset, leaving dyspigmentation but not scars. A subset of patients manifest clinically as those with CBDC but show a mixed pattern of IgA and IgG antibodies on immunofluorescence testing; this entity has been termed mixed immunobullous disease of childhood and is similar to CBDC in terms of target antigens, disease presentation and course, and response to treatment.


Diagnosis
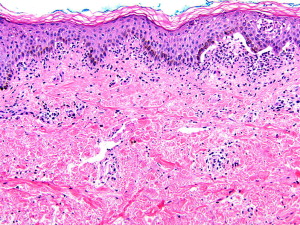
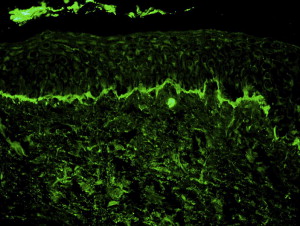
CBDC is diagnosed by hematoxylin-eosin–stained biopsy and immunofluorescence testing. Histology is characterized by a subepidermal blister with a primarily neutrophilic infiltrate in the papillary dermis, although mononuclear cells and occasional eosinophils are also seen ( Fig. 3 ). Immunofluorescence testing of perilesional skin is the gold standard for diagnosis and shows linear IgA staining along the BMZ ( Fig. 4 ). For unclear reasons, the volar forearm seems to be an inferior site for biopsy because immunofluorescence testing may give a negative result. Circulating autoantibodies are of the IgA1 subclass and can be found in more than 90% of patients. Autoantibodies bind the epidermal side of salt-split skin in most patients; however, antibody binding to the dermal side of salt-split skin or to both the epidermal and dermal sides occurs in some. The heterogeneous indirect immunofluorescence pattern is explained by the variety of antigenic epitopes, as described later. The lesions are sterile unless they have become secondarily colonized or superinfected with bacteria.
In addition to the common initial clinical suspicion for bullous impetigo, the differential diagnosis of CBDC includes epidermolysis bullosa acquisita and other autoimmune bullous disorders.
Diagnosis
CBDC is diagnosed by hematoxylin-eosin–stained biopsy and immunofluorescence testing. Histology is characterized by a subepidermal blister with a primarily neutrophilic infiltrate in the papillary dermis, although mononuclear cells and occasional eosinophils are also seen ( Fig. 3 ). Immunofluorescence testing of perilesional skin is the gold standard for diagnosis and shows linear IgA staining along the BMZ ( Fig. 4 ). For unclear reasons, the volar forearm seems to be an inferior site for biopsy because immunofluorescence testing may give a negative result. Circulating autoantibodies are of the IgA1 subclass and can be found in more than 90% of patients. Autoantibodies bind the epidermal side of salt-split skin in most patients; however, antibody binding to the dermal side of salt-split skin or to both the epidermal and dermal sides occurs in some. The heterogeneous indirect immunofluorescence pattern is explained by the variety of antigenic epitopes, as described later. The lesions are sterile unless they have become secondarily colonized or superinfected with bacteria.