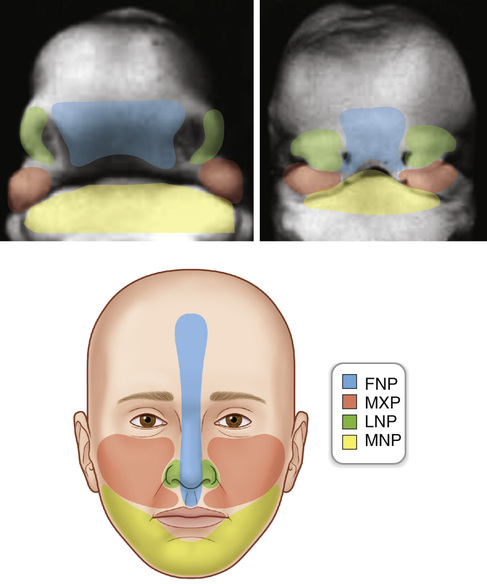
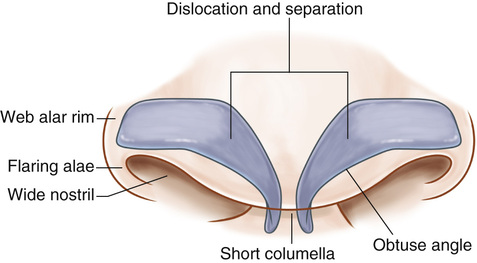
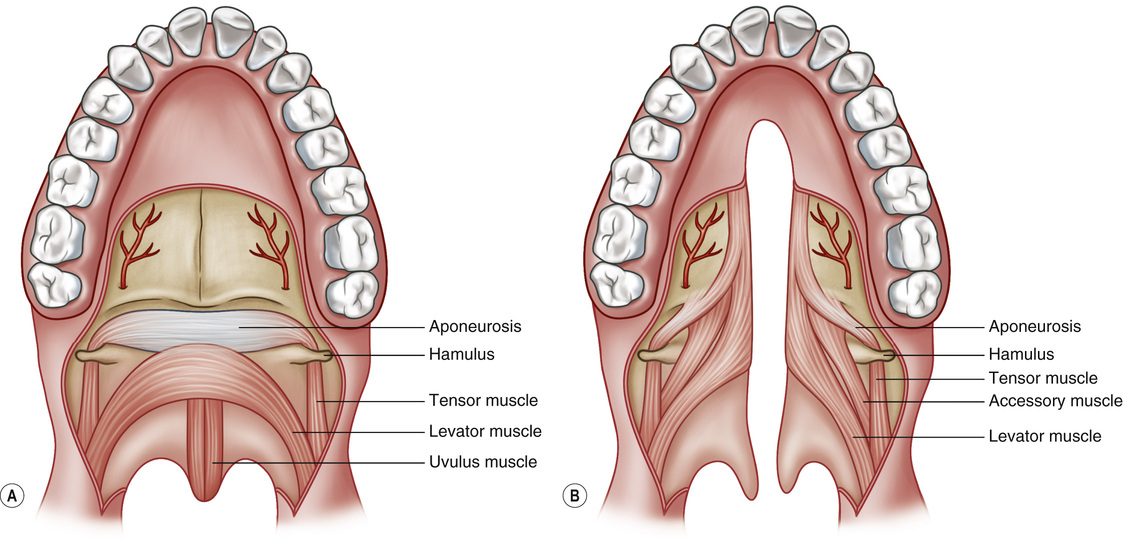
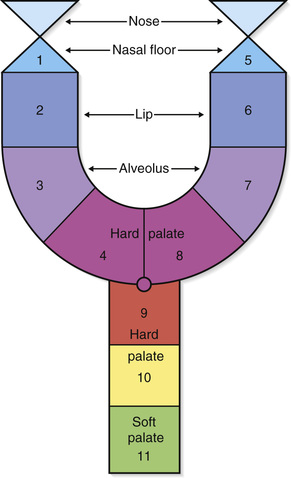
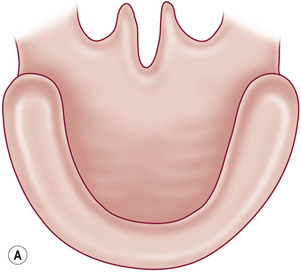
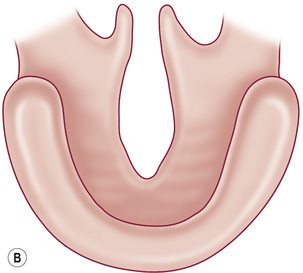
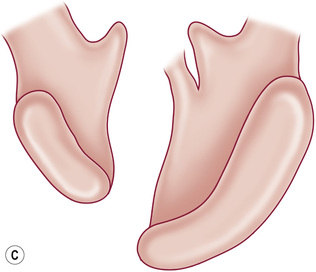
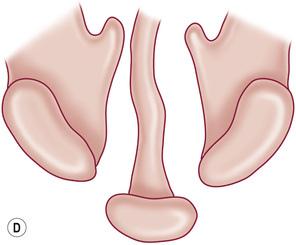
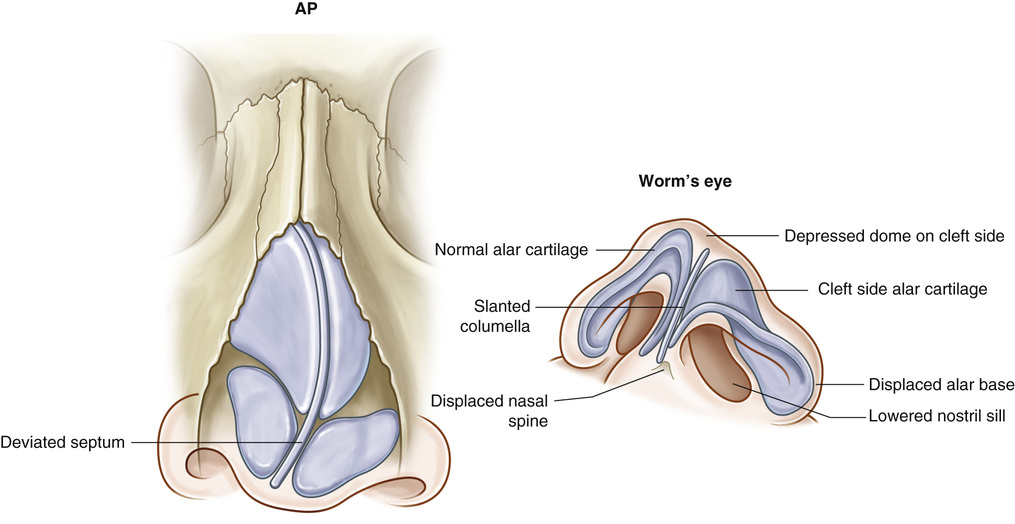
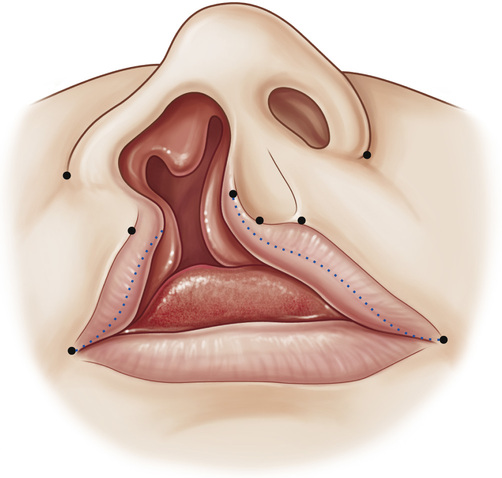
1. The formation of the face occurs between the 4th and 10th weeks of human development, secondary to fusion of the midline frontonasal prominence and the paired maxillary, lateral nasal, and mandibular prominences (see Figure 6.1). ▪ Gives rise to the lateral and medial nasal processes • Lateral nasal prominence/process ▪ Forms the upper jaw, sides of the face, sides of the upper lip, and the secondary palate • From disruptions occurring during the 3rd to 7th weeks of gestation • From disruptions occurring during the 5th to 12th weeks of gestation 1. Isolated cleft palate and cleft lip with or without cleft palate are thought to be two genetically distinct deformities (see Table 6.1). • The incidence of isolated cleft palate is approximately 1:2000 in Caucasians. • Cleft lip/palate is more common in boys. • Isolated cleft palate is more common in girls. • Cleft lip/palate affects the left side more often. Table 6.1 Incidence of Cleft Lip/Palate in Differing Ethnic Groups 2. Isolated cleft palate is associated with a craniofacial syndrome in as many as 50% of patients, whereas only 30% of cleft lip/palate patients have an associated syndrome. ▪ One of the most common syndromes associated with clefts ▪ Characterized by lower lip sinus tracts (“pits”), cleft lip/palate, or cleft palate • 22q chromosomal deletion (“velocardiofacial syndrome”) ▪ Common syndrome associated with clefts (particularly, cleft palate) ▪ Characterized by the triad of micrognathia, glossoptosis, and respiratory distress ▪ 60-90% have associated cleft palate, which is typically of the soft palate and is U shaped or wide ▪ Unaffected parents with one affected child: Recurrence risk of 4% ▪ Unaffected parents with two affected children: Recurrence risk of 9% ▪ One affected parent and no affected children: Recurrence risk of 4% ▪ One affected parent and one affected child: Recurrence risk of 17% ▪ Unaffected parents with one affected child: Recurrence risk of 2% ▪ Unaffected parents with two affected children: Recurrence risk of 1% ▪ One affected parent and no affected children: Recurrence risk of 6% ▪ One affected parent and one affected child: Recurrence risk of 15% • Orbicularis abnormally inserts onto the columella on the noncleft side and the ala on the cleft side • Complete: Cleft includes the nasal sill. • Incomplete: Nasal sill contains some soft-tissue elements (“Simonart’s band”). 2. Bilateral cleft lip (see Figure 6.2) • Orbicularis oris abnormally inserts onto the ala bilaterally. • Prolabium is void of any orbicularis muscle and is often protruded forward. • Severe deficiency of columellar height 3. Cleft palate • Levator palatini abnormally inserts onto the hard palate instead of decussating in the midline. ▪ Leads to severe Eustachian tube dysfunction; chronic otitis media found in 96% to 100% of patients (see Figure 6.3) ▪ Kernahan Y classification (see Figure 6.4) ▪ Veau classification (see Figure 6.5) ▪ Requires speech evaluation to determine symptomatology. 4. Unilateral cleft nasal deformity • Septum is deviated toward the cleft side. • Anterior nasal spine and nasal tip are deviated toward the noncleft side. • Piriform and alveolus on the cleft side are displaced posteriorly. • Ala on the cleft side is flattened and displaced inferior, posterior, and lateral • Columella is deficient (see Figure 6.6). 1. Requires multidisciplinary team care. 2. Initial treatment should focus on parental reassurance and counseling, feeding, and infant growth. 3. General sequence and timing of repair (see Table 6.2). Table 6.2 Surgical Protocol 5. Unilateral cleft lip repair (see Figures 6.7 and 6.8) • Often performed at 3 months of age, following the “rule of 10s”: 10 weeks, 10 g hemoglobin, 10 kg. • C flap is created on noncleft side and used to lengthen the columella. • Complications of unilateral cleft lip repair include ▪ Poor scarring: Treat early scar contracture conservatively because most will settle. ▪ Inadequate rotation: May perform re-repair with rotation-advancement flap technique.
Clefts and Orthognathic Surgery
Embryology
Epidemiology
ETHNICITY
INCIDENCE PER 1000 BIRTHS
Amerindian
3.6
Japanese
2.1
Chinese
1.7
White
1.0
African-American
0.3
General Anatomy
Cleft Care
3 months
Primary cleft lip and nose
8 months
Two-flap palatoplasty
5 years (35%)
Secondary minor lip–nose
7-9 years (100%)
Cancellous iliac bone graft to alveolar cleft
7 years (full growth)
Distraction osteogenesis >12 mm, occlusal class III
Full growth (25-30%)
Orthognathic surgery
12-18 years
Rhinoplasty; other secondary soft tissue
Clefts and Orthognathic Surgery
Chapter 6