I. OVERVIEW
A. Cleft lip (CL) and cleft lip and palate (CLP) versus cleft palate (CP) only
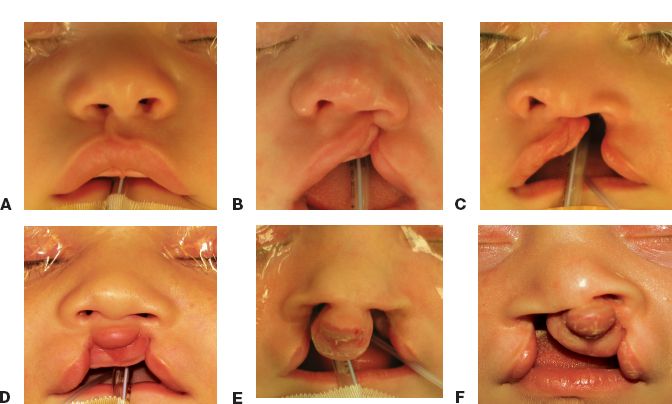
1. CL and CLP are the same entity along a morphologic continuum (Fig. 25-1)
2. “CP only” is a distinct entity (see Chapter 26)
3. In addition, CLP has a separate pathophysiology from Tessier facial clefts (see Chapter 27)
B. Surgical treatment
1. Directed at restoring lip form and function, correcting nasal deformity
2. Goals
a. Lengthen medial lip element (in unilateral deformity)
b. Restore nasal width
c. Reconstitute orbicularis oris muscle
C. Cleft care requires a collaborative multidisciplinary team
II. EPIDEMIOLOGY
A. *Incidence of CL with or without CP
1. Caucasian ancestry: 1:1,000 live births
2. Asian ancestry: 1:500 live births
3. African ancestry: 1:2,000 live births
B. Demographics
1. Male:female = 2:1
2. Left:right:bilateral = 6:3:1
3. Risk factors
a. Fetal exposure to substances including phenytoin, EtOH, steroids, phenobarbital, diazepam, and isotretinoin
b. Maternal smoking
c. Parental age, especially advanced paternal age
d. Family history of clefting
C. *Genetics
1. Risk of clefting in subsequent children
a. If one child or one parent has CLP, there is a 4% chance of subsequent clefting in successive pregnancies
b. If two children have CLP: 9%
c. If one child and one parent both have CLP: 17%
2. Most cases are sporadic, multifactorial, and no genetic cause is identified
3. CLP is syndromic in <15% of cases
a. Van der Woude’s syndrome
i. Is the most common syndrome associated with CL
ii. *Autosomal dominant, with variable penetrance
iii. *Associated with lip pits (accessory salivary glands)
iv. May also have absent second molar, syndactyly, abnormal genitalia, and popliteal pterygia
______________
*Denotes common in-service examination topics
Figure 25-1. The spectrum of cleft lip—A: microform unilateral cleft lip; B: incomplete unilateral cleft lip; C: complete unilateral cleft lip; D: incomplete bilateral cleft lip; and E: complete bilateral cleft lip with “flyaway” premaxilla; F: right complete cleft and left incomplete cleft lip.
b. Waardenburg syndrome (sensorineural hearing loss, iris pigment abnormality, hair hypopigmentation, and lateral displacement of medial canthi)
c. Trisomy 21 (Down syndrome)
d. Trisomy 13 (Patau syndrome)
e. Trisomy 18 (Edward syndrome)
III. EMBRYOLOGY
A. *Critical developmental period: 4 to 6 weeks
B. *CL is caused by failure of union between medial nasal process and maxillary prominence
C. Variable extent of clefting of the primary palate occurs (Fig. 25-1) in CL, including
1. Upper lip
2. Nasal floor (or nostril sill)
3. Alveolus
4. Hard palate (anterior to incisive foramen)
D. May involve the secondary palate (posterior to incisive foramen), and this combination is termed “cleft lip and palate”
IV. PATHOPHYSIOLOGY/EMBRYOLOGY
A. Interrupted mesenchymal migration and fusion of frontonasal, maxillary, and mandibular processes
B. Week 3
1. Genesis of branchial arches and growth of frontonasal prominence
2. Streaming of neural crest cells into mesoderm of early facial and frontonasal prominences and laterally in first and second branchial arches
3. These neural crest cells are responsible for the fusion of facial prominences
C. Week 4 to 7
1. Medial nasal processes fuse with maxillary prominences to form philtrum and primary palate (failure causes CL)
2. Maxillary prominences become the lateral upper lip and maxilla and secondary palate
3. The two lateral palatine shelves that initially lie in a vertical plane adjacent to the tongue move into horizontal plane and fuse at midline along with the primary palate (failure causes CP)
4. Nasal septum forms from fusion of medial nasal prominences and grow downward to join the fused palatal shelf
V. CLASSIFICATION OF CLEFT LIP
A. Severity/extent (Fig. 25-1)
1. Microform CL (“forme fruste” or “minor cleft lip”; Fig. 25-1A)
a. Vermilion notching, scar-like line or depression, lip shortening
b. ± Nasal deformity, usually mild
c. Surgery may or may not be indicated based on severity
2. Incomplete CL (Fig. 25-1B)
a. Intact nasal sill (termed “Simonart band”)
b. Intact alveolar ridge
3. Complete CL (Fig. 25-1C)
a. Clefting of the lip, nostril sill, and alveolus
b. Wider than incomplete clefts with greater cleft nasal deformity
4. Complete CLP
a. CL deformity is same as above
b. Includes CP (posterior to incisive foramen)
B. Unilateral versus bilateral
1. Unilateral CL
a. Greater segment
b. Lesser segment collapse, with medial and posterior displacement
2. Bilateral CL (Fig. 25-1D-F)
a. Central prolabium and premaxilla
b. May have “flyaway” premaxilla (Fig. 25-1E) and collapsed bilateral lesser segments
c. Variable severity per side (Fig. 25-1F)
d. More likely to be complete, wide clefts
VI. ANATOMY
A. Normal lip anatomy (see Chapter 21—Fig. 21.1)
1. Central philtrum demarcated laterally by philtral columns and inferiorly by Cupid’s bow and tubercle
2. Above the junction of vermilion–cutaneous border is mucocutaneous ridge (“white roll”)
3. Within red vermilion, noticeable junction demarcating dry and wet vermilion (“wet–dry border”)
4. Vertical height of upper lip = peak of Cupid’s bow to nasal sill
a. Newborn—10 mm
b. 3 months—13 mm
c. Adult—17 mm
5. Musculature
a. Orbicularis oris—primary muscle of lip, has two well-defined components (CN VII)
i. Deep (internal)
a) Fibers circumferentially from modiolus to modiolus
b) Functions as the primary sphincter for feeding
ii. Superficial (external)
a) Fibers run obliquely, interdigitating with the other muscles of facial expression to terminate in the dermis
b) Provide subtle shades of expression and precise movements of lip for speech
c) Fibers decussate in the midline and insert into the skin lateral to the opposite philtral groove forming the philtral columns
d) Philtral dimple is depressed centrally because no muscle fibers directly insert into the dermis in the midline
e) Pars marginalis—portion of orbicularis along the vermilion forming the tubercle of the lip with eversion of the muscle
b. Levator labii superioris
i. Fibers arise from medial aspect of infraorbital rim, insert near vermilion–cutaneous junction
ii. Medial-most fibers insert near the corner of the ipsilateral philtral column and vermilion–cutaneous junction helping to define the lower philtral column and peak of Cupid’s bow
c. Nasal muscles
i. Levator labii superioris alaeque nasi arises along the frontal process of maxilla and inserts on the mucosal surface of the lip and the ala
ii. Transverse nasalis arises along the nasal dorsum and sweeps around the ala to insert along the nasal sill from lateral to medial and into the incisal crest and anterior nasal spine (ANS)
iii. These join with the oblique fibers of orbicularis and depressor septi
iv. Depressor septi arise from alveolus between the central and lateral incisors to insert into the skin of the columella to the nasal tip and the footplates of the medial crura
6. Blood supply
a. Superior labial arteries, bilaterally; columellar branch centrally
b. Branch off from bilateral facial arteries
7. Sensory innervation: Upper lip, maxillary division of trigeminal nerve (CN V2)
8. Motor innervation: Zygomatic and buccal branches of the facial nerve (CN VII)
B. Unilateral CL anatomy
1. Muscles
a. *Pathological insertion of orbicularis oris
i. Runs parallel along the edge of cleft and inserts on alar base (cleft side), base of columella (noncleft side)
ii. Responsible for nasal distortion and widening of cleft with smiling
b. Hypoplasia and disorientation of pars marginalis associated with disappearance of vermilion–cutaneous ridge (white roll) at cleft margin
c. Deep fibers interrupted at the level of submucosa in both complete and incomplete clefts
d. Levator labii and nasalis muscles are similarly distorted
e. Incomplete cleft: If cleft is less than two-thirds of lip height, some superficial orbicularis fibers may traverse superior lip across the cleft
f. Simonart’s band: Skin bridge (contains no muscle) in nasal sill across incomplete cleft
2. Vertical lip height is decreased on noncleft side
3. Disrupted Cupid’s bow
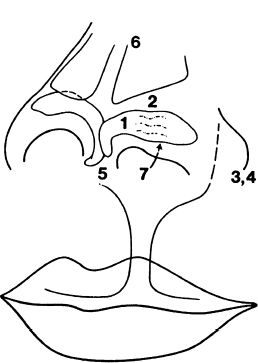
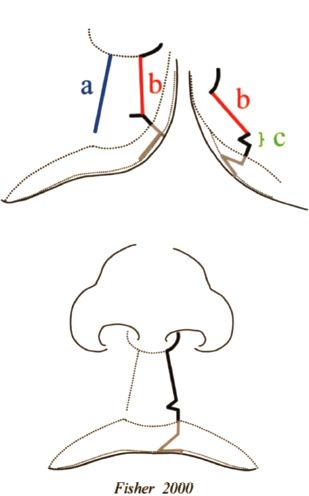
4. *Nasal abnormalities (Fig. 25-2)
a. Hypoplastic, flattened alar dome on the affected side
b. Lack of upper lateral cartilage overlap of lower lateral cartilage
c. Subluxed lower lateral cartilage with alar base displaced cephalad and posteriorly
d. Hypoplastic bony foundation (maxilla)
e. Caudal septum is pulled toward the noncleft side by aberrant insertion of orbicularis oris
f. Flattening of the nasal bones
g. Shortened columella, especially in bilateral cases
C. Bilateral CL anatomy
1. Two lateral components (lesser segments) of lip–alveolus–palate with an intervening prolabium and premaxilla that varies in its degree of protrusion (mild vs. “flyaway”)
2. Widened alar bases, with laterally flared alar domes and malpositioned cartilages
3. Shortened columella (hallmark of cleft nasal deformity)
4. Obtuse nasolabial angle
5. Hypoplastic prolabium
Figure 25-2. The cleft nasal deformity. The lower lateral cartilage on the cleft side is abnormally shaped and improperly positioned. Numbers 1 and 7, hypoplastic, flattened alar dome on the affected side; 2, lack of upper lateral cartilage overlap of lower lateral cartilage; 3, subluxed lower lateral cartilage with alar base displaced cephalad and posteriorly; 4, hypoplastic bony foundation (maxilla); 5, the caudal septum is pulled toward the non-cleft side; and 6, flattening of the nasal bones.
6. Absence of normal labial–gingival sulcus in premaxillary segment
7. Total absence of orbicularis muscle in prolabial segment results in the absence of philtral dimple/columns/white ridge and median tubercle
8. Absence of Cupid’s bow
9. Aberrant insertion of lateral lip orbicularis oris muscle into alar bases
10. Aberrant dry and wet vermilion on prolabial segment
VII. INTERVENTION
A. Initial evaluation
1. Reassure parents and family
2. Explain surgical goals and timing of interventions
3. Evaluate for associated anomalies (especially with isolated CP)
4. Consultations
a. Genetics
b. Social work
c. Feeding/nutrition
i. Monitor for appropriate weight gain
ii. May require Haberman bottle or cross-cut nipple to reduce the work of feeding, especially with CP
d. Otolaryngology
i. Eustachian tube dysfunction (see Chapter 26) often requires myringotomy tubes
ii. Repeat otitis media affects hearing and speech development
B. Preoperative molding may be used to bring cleft segments together to minimize tension during repair
1. Taping
a. Applied across both segments of the lip
b. Requires compliant and reliable parents
2. Lip adhesion: Suturing cleft margins together
a. Incisions should be made in region that will be discarded at subsequent operation (mark key landmarks)
b. Goal: Turn a complete CL into an incomplete CL
c. Definitive lip repair performed several weeks to months later
3. Nasoalveolar molding (NAM)
a. Custom fabricated oral appliance with nasal stents adjusted weekly
b. Goals of NAM are similar to the above methods; NAM positions nasal cartilages and alveolar processes to facilitate closure
c. *NAM can lengthen deficient columella
d. Takes advantage of increased plasticity of neonatal cartilage
i. First 2 to 3 months of life
ii. High circulating maternal estrogen
4. Active presurgical infant orthopedics
a. Orthodontic appliance (Latham device) rigidly fixed to palatal segments
b. Parents adjust daily to bring alveolar segments into alignment
c. Removed at the time of definitive lip repair
C. Timing of CL repair
1. 3 months of age, generally accepted
2. “Rule of Tens” (historical criteria) for suitability for surgery
a. 10 weeks old
b. 10 pounds
c. Hemoglobin10 mg/dL
3. May delay in syndromic patients with systemic concerns
4. CP repair and secondary alveolar grafting (see Chapter 26)
VIII. OPERATIVE TREATMENT
A. Goals of unilateral repair
1. Lengthen medial lip element
2. Reconstitute orbicularis oris
3. Restore Cupid’s bow, aligning white roll and wet–dry vermilion
4. Correct nasal deformity (primary rhinoplasty)
a. Upright caudal septum
b. Narrow alar base on the cleft side
c. Establish convexity of lower lateral cartilage on the cleft side
d. May use nasal conformers to maintain shape
B. Goals for bilateral repair
1. Symmetry
2. Reconstitute orbicularis oris across premaxilla
3. Achieve proper prolabial size and shape
a. ~10 mm height
b. ~3 mm from midline to each Cupid’s bow peak
4. Formation of median tubercle from lateral lip vermillion–mucosa (see “Techniques” later)
5. Correct nasal deformity (primary rhinoplasty)
a. Narrowing alar base is key difference in emphasis from unilateral technique
b. Nasal conformers also used
C. Key landmarks: Intraoperative tattooing (e.g., with methylene blue and quill pen)
1. Alar bases (i.e., subalare: Alar insertion point onto upper lip)
2. Columellar–labial junction
3. White roll
a. At the peak of Cupid’s bow on non-CL
b. At the trough of Cupid’s bow (tubercle) on non-CL
c. Additional mark equidistant from the trough to the peak on medial cleft element
i. Define peak of Cupid’s bow for CL segment
ii. Peaks are approximately 3 mm from the trough on each side
d. Noordhoff’s point: Vanishing point of white roll on CL segment
i. Most critical and difficult point to identify
ii. Should correspond to region of thickest vermillion and robust white roll
iii. In bilateral cases, this is marked on each cleft segment
D. Mark lines for preferred repair type
E. Infiltrate tissue with local anesthetic + epinephrine
F. Cut on the inside of your marks so they remain visible
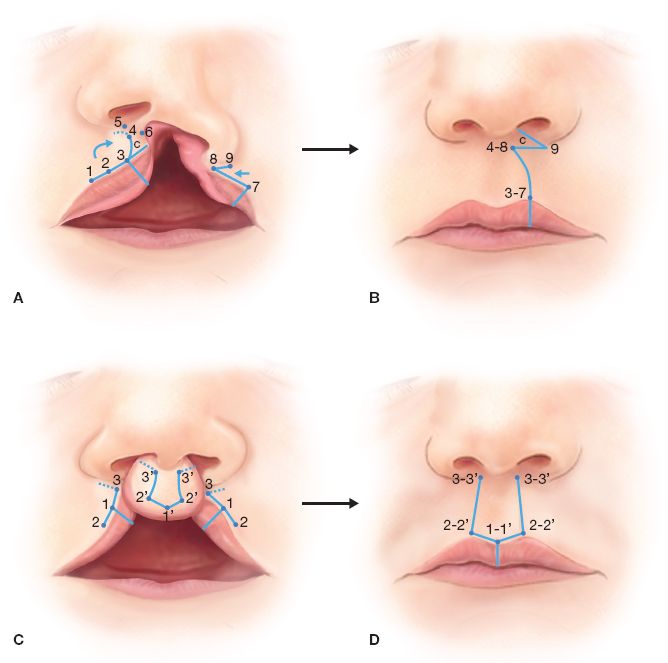
Figure 25-3. Example of surgical repairs of the unilateral and bilateral cleft lip deformities. A: Preoperative markings for the unilateral lip repair. B: Postoperative result for unilateral lip repair. C: Preoperative markings for the bilateral lip repair. D: Postoperative result for bilateral lip repair.
IX. CHEILOPLASTY TECHNIQUES (FIG. 25-3)
A. Unilateral CL repair variations. Note most are Z-plasty-based reconstructions
1. Straight-line repair (Rose–Thompson): Excision of cleft margin and primary straight-line closure; Rose–Thompson repair incorporates Z-plasty to establish normal vertical height of the lip
2. Quadrangular flap (Le Mesurier): Uses a back-cut above Cupid’s bow and a laterally based inferior rectangular flap to fill in the rotational defect of the medial lip element
3. Triangular flap (Randall-Tennison, Trauner, and Skoog): Incorporates Z-plasty to restore vertical height
a. May result in excess vertical length
b. Places scar in the center of lip with oblique portion crossing philtrum
4. Rotation advancement
a. Poole
i. Similar to Millard which moves cleft advancement flap back-cut inferi-orly ~3.5 mm
ii. May place scar in undesirable area in center of upper lip
b. *Millard (Fig. 25-4)
i. Most commonly used repair currently in the United States
ii. Incorporates the Z-plasty superiorly
iii. “Cut-as-you-go” technique
a) C-flap back-cut is variable
b) Determined intraoperatively
iv. Medial lip rotated downward
v. C-flap (“c” is for columella)
a) Rotated to create the nasal sill, or
b) Used to lengthen the columella (more common)
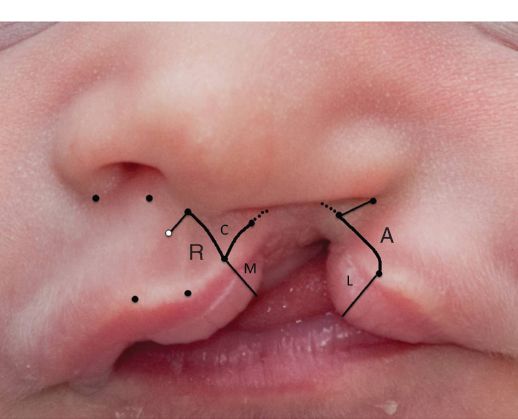
Figure 25-4. Unilateral cleft lip deformity, with preoperative markings for (Millard) repair. For clarity, descriptive anatomy is used in place of numbers. First, mark the peak of the Cupid’s bow on the noncleft side. Then mark the nadir of the Cupid’s bow. Extrapolate the proposed peak of the Cupid’s bow in the cleft equidistant from the nadir of the Cupid’s bow. Next, mark the superior point of the philtral column on the noncleft side: This is the height of the normal philtral column that you must achieve with the cleft side! You also need to establish the normal width of the nostril floor. To do this, mark the midpoint at the columellar–labial junction and then mark subalare: the alar insertion point on the normal side. This distance must equal the distance between subalare on the cleft side (please go ahead and mark this now) and your midline columellar–labial mark. The defect in the nasal floor will need to be closed to close this distance. At the junction of the nasal floor and the lip skin, mark off a proposed “wedge excision” (two marks here) that will achieve this. … Noordhoff’s point: the point at which the white roll begins to fade and where the vermillion begins to thin toward the cleft must now be marked. This last point is the point that only your attending can correctly mark preoperatively. In the Millard repair, the incision is made through the vermillion to the new Cupid’s bow peak and then up toward the columellar midpoint. A back-cut via “cut-as-you-go” is then made toward the open circle. Again, only your attending knows how far to make this back-cut. This releases the lip, thereby lengthening the non-cleft side. Care must be taken to avoid crossing the noncleft philtral column. On the cleft side, the incision is carried through the vermillion and Nordhoff point, to the superior-medial most point on the cleft lip, then back laterally toward subalare along the skin/nostril sill junction. Nasal dissection for primary rhinoplasty is then performed through these incisions. Once the muscle is dissected free of the skin and mucosa, and disinserted from its abnormal attachments, it can be reapproximated transversely in the midline. The mucosa is also closed in a separate layer, using the M-flap, and then the L-flap is used for nasal lining. The C-flap rotates toward the columella for inset, and closure of the lip commences with the white roll. (A, Advancement flap; R, Rotationflap)
vi. *Nasal lining is repaired with L-flap from mucosal portion of lateral segment (“l” is for lining)
a) This is required because the cleft ala is posteriorly displaced (Fig. 25-2)
b) When ala advanced forward to desired position, mucosal defect must be filled to prevent contraction
c) May also be filled with turbinate flap
vii. Gingivolabial sulcus is augmented with M-flap from mucosal portion of medial segment (“m” is for mucosa)
viii. Scar follows the line of philtral column and preserves Cupid’s bow
ix. Orbicularis oris muscle repair is important to restore dynamic lip function
a) Muscle fibers are inappropriately inserted into the alar base and columella
b) Must be completely disinserted and repaired in a transverse position
x. Primary rhinoplasty
a) Diffuse undermining of alar cartilage
b) Transnasal suture techniques to secure desired position
c) May use nasal conformers to maintain shape
xi. Common pitfall: Inadequate rotation and inadequately corrected vertical lip height on non-cleft side; “whistle deformity”
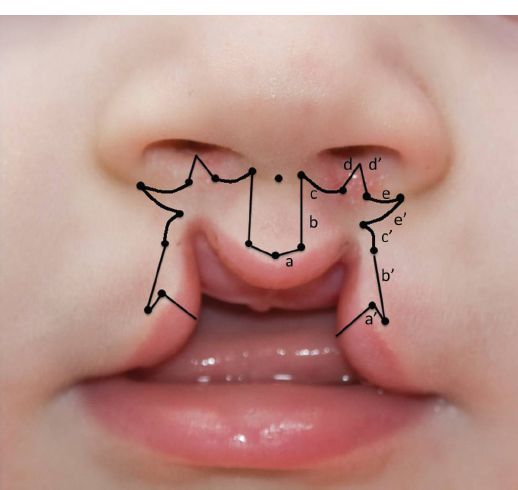
c. Fisher repair (anatomic subunit, Fisher DM; Plast Reconstr Surg. 2005) is editor’s preferred technique (Fig. 25-5)
i. Markings are similar to Millard but closure lines are placed along anatomic subunits
ii. Stresses the importance of complete leveling of the Cupid’s bow
a) a = greater lip height
b) b = lesser lip height
c) c = difference between “a” and “b”
Figure 25-5. Unilateral cleft lip Fisher repair. The height of the greater lip segment is measured from white roll to the apex of philtral column “a.” The height of the lesser lip segment is similarly measured “b.” The difference between “a” and “b” is made up with a triangle from the cleft lip element “c.” Because of the Rose–Thomson effect, 1 mm is subtracted from triangle “c.” Noordhoff point is marked on the cleft side. From the proposed location of the philtral column apex on the cleft side, the length “b” is marked with a compass so that it coincides with Nordhoff point and the triangle “c.” A back-cut is made beneath “a” to admit the triangle “c.” A similar triangle may be required in the vermillion to augment the thickness of the vermillion on the medial aspect of the cleft.
iii. A white roll triangular flap (a “Nordhoff triangle” or “c”) is used to achieve Cupid’s bow symmetry
iv. The equation: a − b − 1 mm = c
a) Accounts for 1 mm lengthening effect
b) “Rose–Thompson” effect: Lip repair via closure as an ellipse will “automatically” lengthen the incision
v. Vermilion height is equalized by using a similar triangle as a vermilion flap
B. Bilateral CL repair (Fig. 25-6)
1. Measurements and maneuvers (Millard repair)
a. Prolabium is used to create the philtrum only
b. Prolabial white roll and vermillion are discarded; the remaining prolabial mucosa is rolled inward to reconstruct the central gingivolabial sulcus
i. Prolabial vermillion lacks minor salivary glands
ii. Using this tissue results in dry, chapped, keratotic “patch”
iii. Prolabial vermillion previously used in Manchester repair (of historical interest)
c. Tip: Make width of philtral flap near columella 1 to 2 mm narrower than inferior portion near white roll to allow for subsequent widening
Figure 25-6. Bilateral cleft lip deformity, with preoperative markings. The most inferior point on the prolabium is marked; this will become the trough of the Cupid’s bow. The proposed peaks of the Cupid’s bow are marked approximately 3 mm lateral, on each side, to this point. The center of the columellar–labial junction is also marked, and 2 mm lateral to this, on each side, a mark is also made. Draw a neck-tie that connects these dots. On the lateral lip elements, Nordhoff points are defined and marked above the white roll. About 3 mm lateral to these points, a mark is made that will allow (a) and (a’) to coincide upon closure. Mark subalare bilaterally. The height of the philtrum (b) is transferred to each lateral lip element (b’). Line (c) is marked extending into the nasal floor and (c’) is made to equal length. A similar concept to the unilateral repair is applied to the nasal floor in the bilateral repair, in that a wedge must be taken from the floor to narrow it. This corresponds to (f) and (f’). The prolabial skin inside of the original markings is discarded and the mucosa is used for lining. Lines (e) and (e’) are made to close the distance in vertical lip height to subalare. The lateral lip elements rotate downward, forming the tubercle in the midline.
d. Cupid’s bow and tubercle reconstructed from lateral lip segments, which are advanced medially beneath the elevated philtral flap
e. Alar cinch suture to reposition alar bases
f. Common pitfall(s)
i. Inadequate columellar length
ii. Poor projection of tubercle
iii. May have significant widening of the prolabium
X. SECONDARY PROCEDURES
A. Secondary cheiloplasty
1. Hypertrophic scars
a. Consider massage
b. Silicone sheeting
c. Steroid injections, prior to operative intervention
2. Short scar/lip
a. May be amenable to the addition of Z-plasty
b. Likely requires complete revision
3. Deficient tubercle
a. Most common encountered following bilateral repair
b. Likely requires Abbe flap
i. Lip sharing procedure from the lower lip
ii. Usually performed after maxillary growth or Le Fort I advancement
B. Secondary rhinoplasty
1. May be performed at any age, but commonly at skeletal maturity
2. Open approach requires creative use of preexisting incision or judicious planning of transcolumellar incisions
3. Requires stable bony foundation for the base of nasal pyramid (i.e., previously suitable alveolar bone grafting to address maxillary deficiency)
4. Must address poor tip projection and abnormal alar position
5. Columella and caudal septum may require repositioning to the cleft side and suturing to the ANS
6. Requires addition of anatomic and nonanatomic cartilage grafts
a. Alar contour grafts
b. Onlay tip grafts
c. L-strut grafts
7. Severe septal deviation may require aggressive submucous resection of ethmoid in addition to septal cartilage (used for grafts)
8. Spreader grafts often needed for airway patency at internal nasal valve (see Chapter 30)
QUESTIONS YOU WILL BE ASKED
1. Describe basic CLP epidemiology
a. Asians>Whites>Blacks
b. Left:right:bilateral; 6:3:1
2. What are key timepoints and events in CLP embryology?
a. 4 to 7 weeks, critical period
b. Cleft lip: Failure of fusion medial nasal process and maxillary prominence
c. Cleft palate: Failure of fusion palatal shelves
3. What is most common CLP syndrome and what are the findings?
a. Van der Woude
b. Autosomal dominant with lip pits and CLP
4. What is pathologic anatomy of cleft nasal ala?
a. Posterior and superior displacement
b. Loss of convexity of lower lateral cartilage
5. What is primary goal of unilateral cleft lip repair?
a. Increase the height of medial cleft lip segment
b. Restore continuity of orbicularis
c. Reposition alar base(s)
6. Draw Unilateral and Bilateral CL markings.
See Fig.24-4, 24-5
THINGS TO DRAW
1. Key anatomical landmarks in CLP
2. Unilateral and bilateral Millard repair techniques
Recommended Readings
Fisher DM. Unilateral cleft lip repair: an anatomical subunit approximation technique. Plast Reconstr Surg. 2005;116(1):61-71. PMID: 15988248.
Millard DR Jr. Complete unilateral clefts of the lip. Plast Reconstr Surg Transplant Bull. 1960;25: 595-605. PMID: 14422441.
Millard DR Jr. Refinements in rotation-advancement cleft lip technique. Plast Reconstr Surg. 1964;33:26-38. PMID: 14104544.
Mulliken JB. Primary repair of bilateral cleft lip and nasal deformity. Plast Reconstr Surg. 2001;108(1):181-194; examination 195-196. PMID: 11420522.
< div class='tao-gold-member'>