7 Cheek
Summary
This chapter focuses on the reconstructive principles with respect to the cheek. The cheek is broken up into several subunits including lateral cheek, medial cheek, zygomatic area, and buccal area. Flap design is guided based on location, and special attention must be paid to medial and zygomatic defects that also involve the lower eyelid in order to avoid ectropion. Cheek defects classically involved extensive back cuts and undermining in order to provide tension-free closure.
Keywords: medial cheek, lateral cheek, cervicofacial advancement flap, rhombic flap, transposition flap, undermining, zygomatic
 Introduction
Introduction
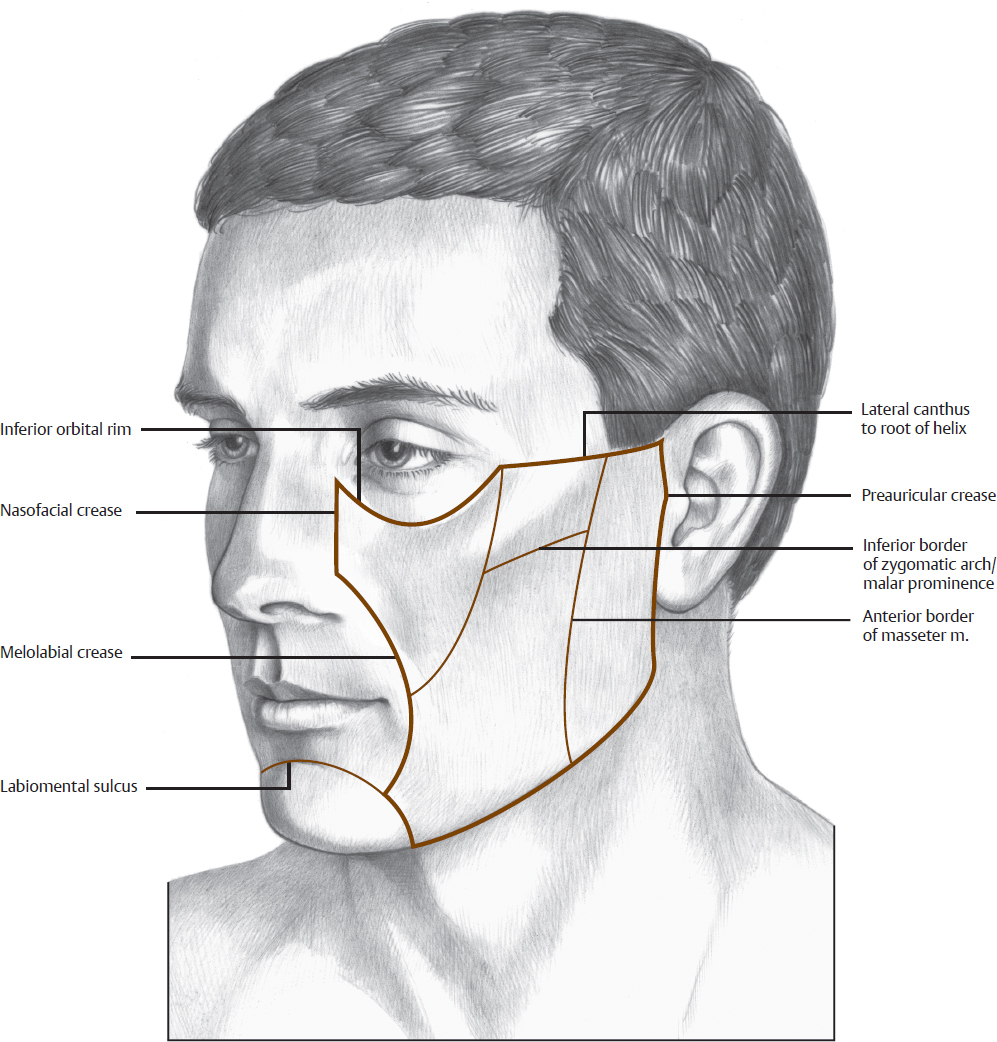
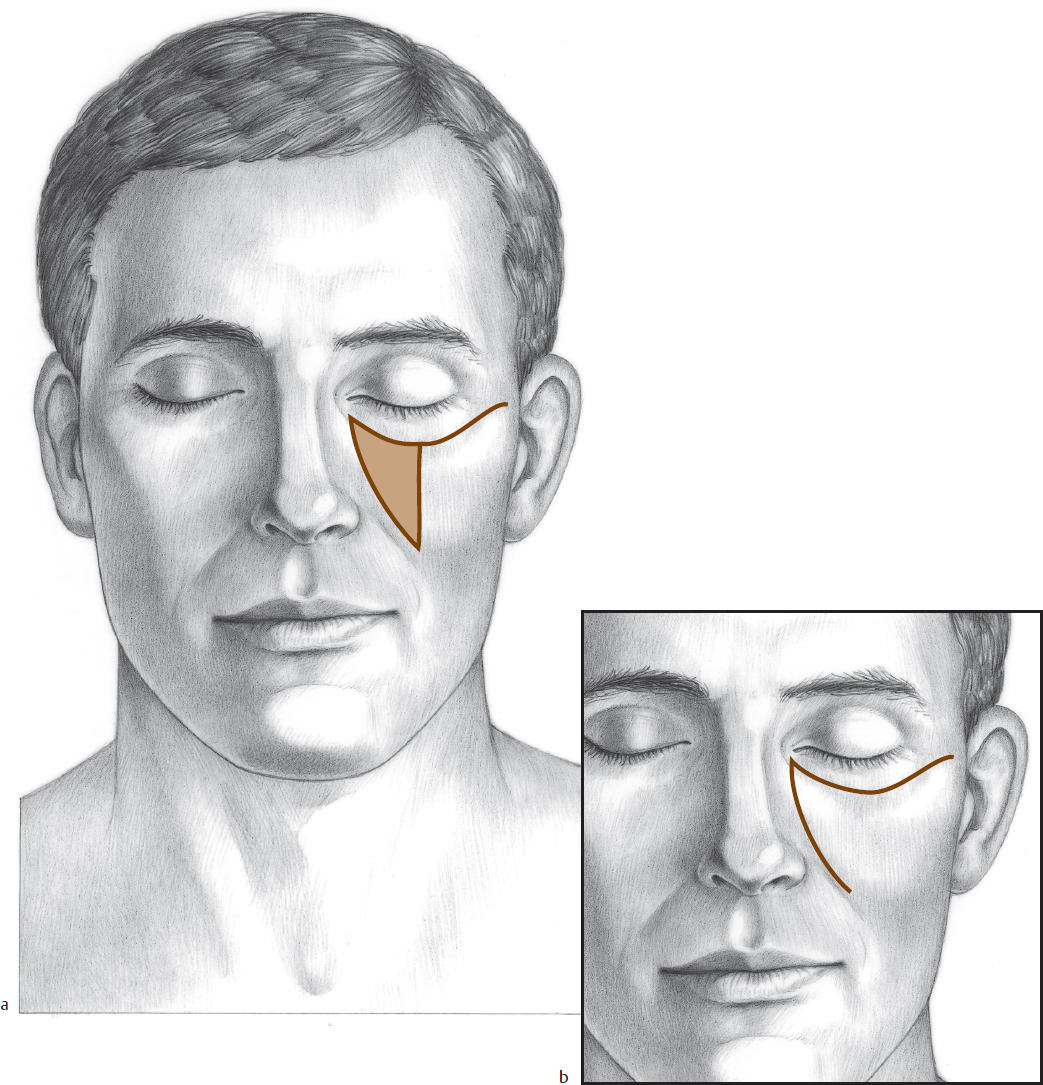
The boundaries of the cheek unit are the preauricular crease, the superior border of the malar eminence and zygomatic arch, the inferior orbital rim, the nasofacial groove, the melolabial crease, and the inferior border of the mandible. The cheek is divided into the medial, zygomatic, buccal, and lateral subunits (Fig. 7.1). The medial and buccal cheek subunits consist of thicker skin that is freely mobile over the underlying fat. The skin of the lateral subunit, over the parotid, is somewhat more attached to the underlying fat and fascia. The skin of the zygomatic subunit (sometimes referred to as the “McGregor’s patch”) has firm fibrous attachments to the underlying fascia.
Because of the broad, relatively flat contour of the cheek, incisions are best placed at the boundaries of this aesthetic unit; rotation and advancement flaps are thus used when possible. For a defect whose position away from the boundaries of the aesthetic unit does not permit use of rotation or advancement flaps, transposition flaps are selected. In the design of local cheek flaps, tension is placed where it will not distort landmarks, such as the eyelid, lip, and ala. Island pedicle flaps are occasionally useful in the medial and central cheek, where the subcutaneous fat allows easy mobility of the attached skin. The flaps are especially valuable if the closure can be camouflaged in the melolabial fold.
 Medial Cheek Subunit
Medial Cheek Subunit
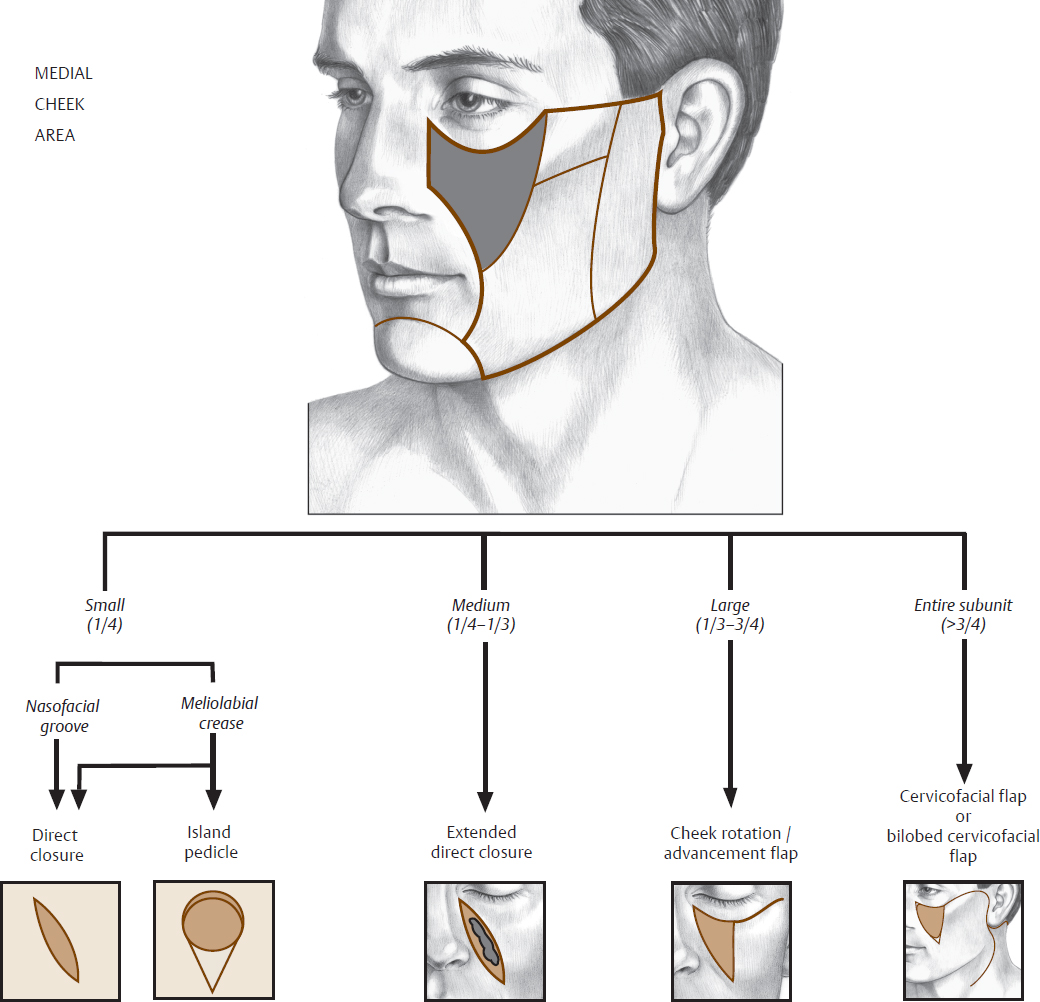
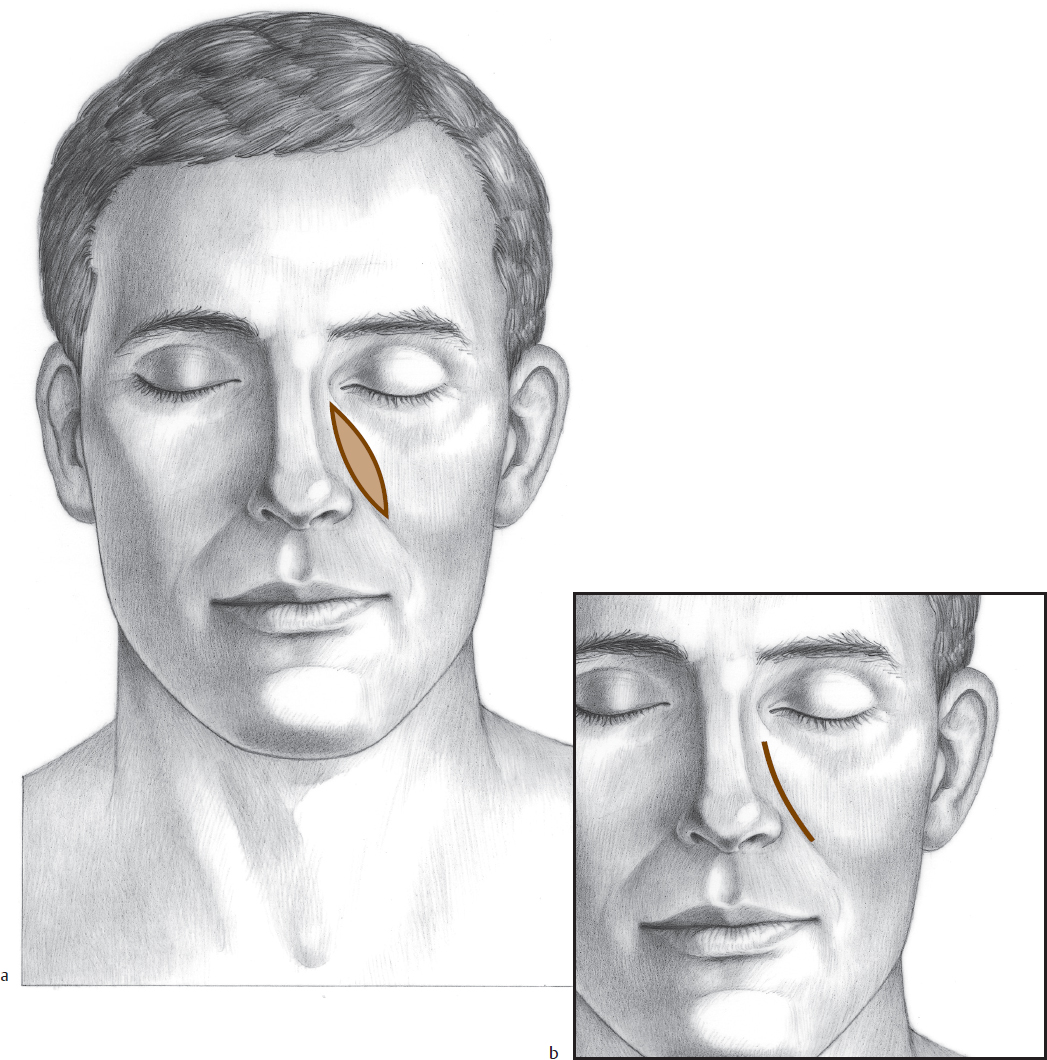
Medial cheek lesions are closed directly in the cheek–nose junction and melolabial fold, when possible (Fig. 7.2). For lesions adjacent to the nose–cheek junction, this closure simply involves undermining the cheek and advancing it (Fig. 7.3). To avoid distortion of the junction of the cheek with the nose, deep sutures from the dermis of the flap are fixed to the periosteum of the nasal bone or pyriform aperture with 3–0 or 4–0 permanent or long-lasting absorbable sutures.
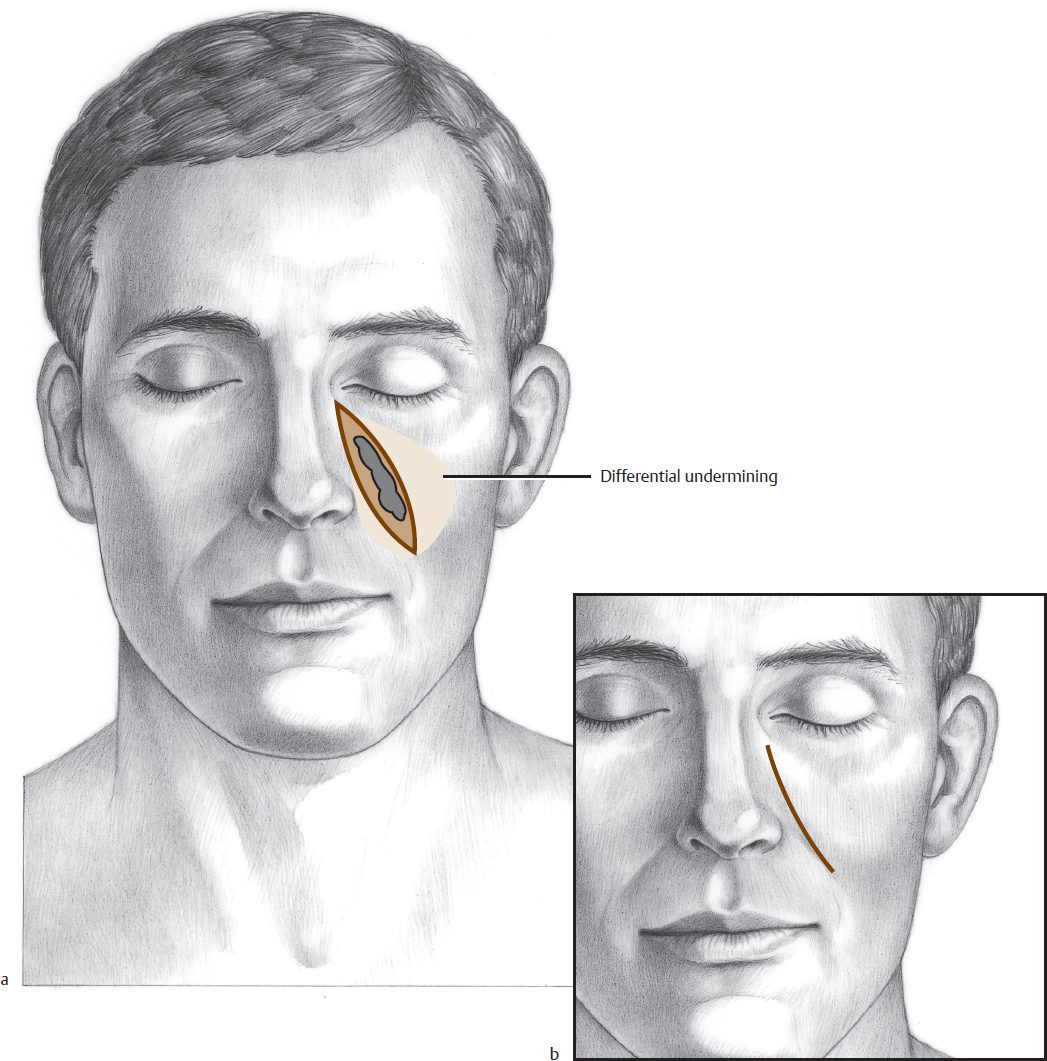
In patients with sufficient cheek laxity, a defect not immediately adjacent to the nose can still be closed in the nasofacial groove by excising intervening skin and creating a simple advancement flap in the plane just deep to the subdermal plexus (Fig. 7.4 and Fig. 7.5). Again, deep sutures must be placed to the pyriform aperture periosteum to prevent distortion of the nasofacial groove.
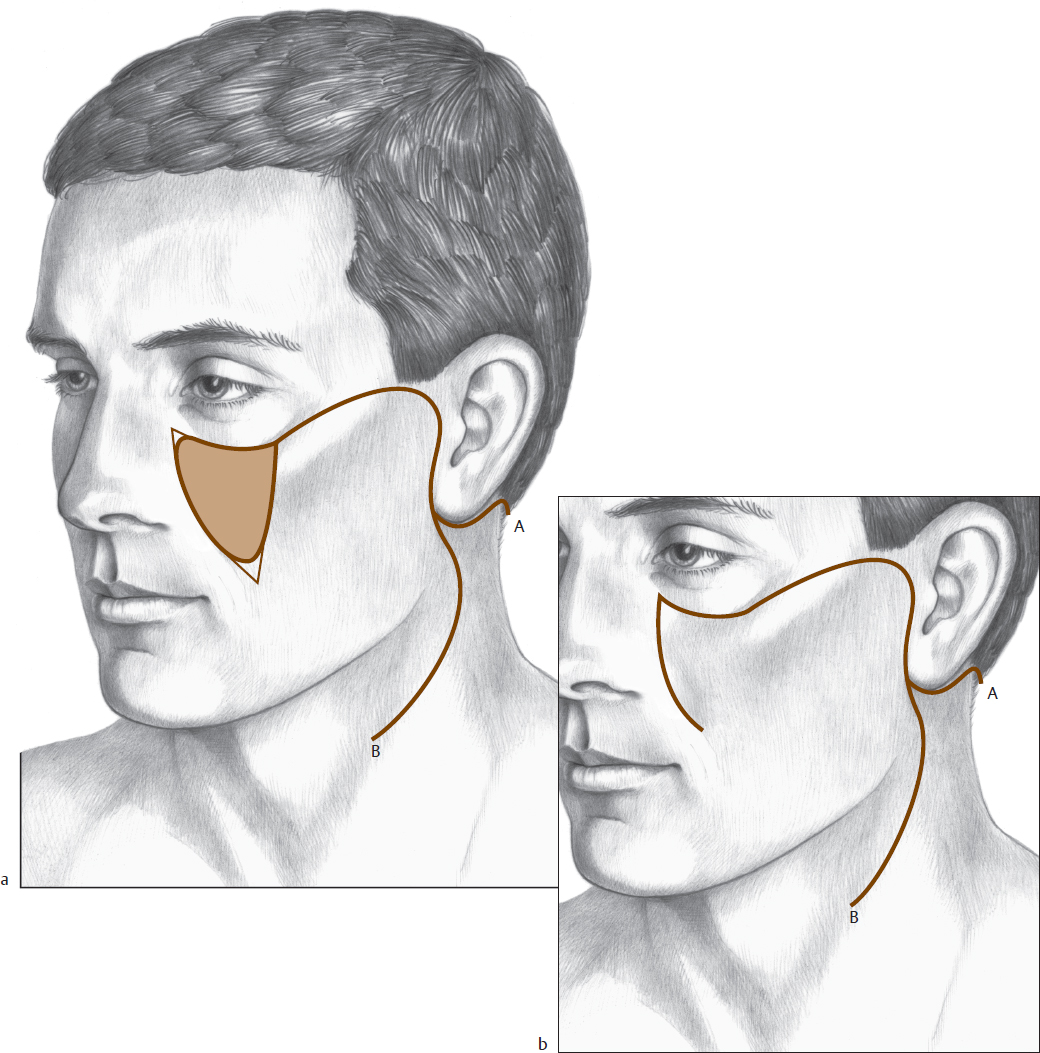
When a defect becomes too large to close with a simple advancement flap, an incision is made along the orbital rim (the junction of the cheek and lid aesthetic units) to create a cheek rotation flap (Fig. 7.6 and Fig. 7.7). This useful flap is elevated in the same subcutaneous plane. As the defect becomes larger, the releasing incision can be extended to create a cervical facial rotation flap (Fig. 7.8 and Fig. 7.9). In practice, the surgeon can proceed in limited stages by making sequential back cuts in the rotation flap until the defect can be closed with minimal tension and contour distortion. The back cuts allow for recruitment of tissue from the submandibular region and the neck. The dermal layer of this flap should be fixed to the periosteum of the inferior and lateral orbital rim with 4–0 long-lasting absorbable sutures to prevent postoperative ectropion formation. If the depth of the defect is greater than the flap thickness, a local “flip-flop” flap of fat can be rotated into the deep layer of the defect prior to flap inset.
For very large medial cheek defects, a bilobed cervicofacial flap with the bilobe from postauricular skin can be used (Fig. 7.10 and Fig. 7.11). If there is not enough laxity to close the postauricular donor site, a full-thickness skin graft can be used to close the site.

Fig. 7.6 (a, b) Simple cheek rotation flap. (c) Medial cheek defect. (d) Medial cheek inferiorly based melolabial flap. (e) Closure. (f) Healed wound.
Fig. 7.7 (a) Cheek defect with rotation flap template. (b) Defect closed with lateral rotation advancement flap. (c) Postoperative appearance.