Chapter 42 FAT GRAFTING FOR BREAST RECONSTRUCTION WITH EXTERNAL VACUUM EXPANSION
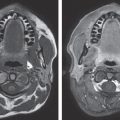
The distractive mechanical force of external volume expansion of the breast produces a three-dimensional vascularized tissue scaffold. The skin expands to create the necessary skin envelope for reconstruction of the new breast, and at the same time, the mechanical force generates new stromal, connective, and vascular tissue. 1 – 7 Once the new biologic scaffold has been expanded and created, the environment is poised to accept microdroplets of autologous fat that must be judiciously diffused without coalescing. There should be minimal increase in interstitial pressure throughout the new scaffold. 8
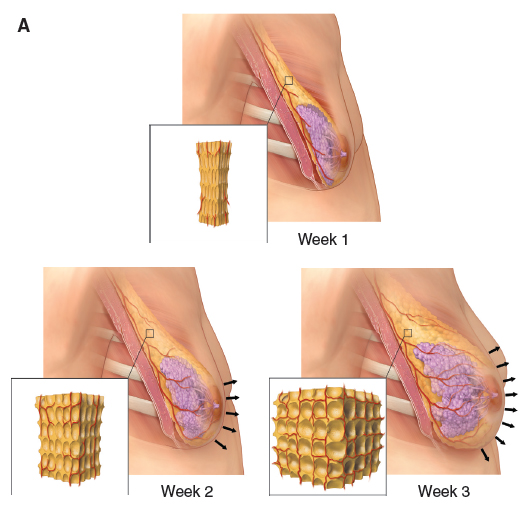
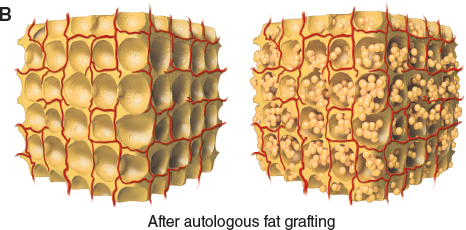
The tissue scaffold is created using an external vacuum expansion (EVE) technique in which new stromal and vascularized tissues are generated. It can be seen how the small droplets of fat fill the small spaces created and will eventually undergo revascularization.
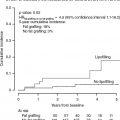
For more than 10 years, the second author (R.K.) has offered this alternative to autologous flap reconstruction. Our recently published multicenter study of 488 patients showed that external tissue expansion with subsequent autologous fat grafting is a safe, effective, and minimally invasive method of breast reconstruction that is performed on an outpatient basis. 9 – 11
In this chapter we will discuss patient selection and preparation for the procedure, surgical techniques for both immediate and delayed reconstruction, clinical outcomes and complications, and cost analysis of the procedure compared with autologous flap reconstruction.
Patient Selection and Preparation
The ideal patient has moderate fat deposits and nonirradiated, unscarred breast tissue, and is a nonsmoker with realistic expectations. We still consider patients with a low BMI who have previously irradiated breasts or scarring to be good candidates for the procedure. However, the procedure will require significantly more effort, time, and expertise in these patients, and it should therefore be approached with more caution. Our exclusion criteria include smoking, bleeding disorders, skin conditions that lead to deepithelialization (such as epidermolysis bullosa and pemphigus), an active skin infection where the expansion device will be placed, and patients with unrealistic expectations.
The expansion process and the time frame involved must be thoroughly discussed during the initial consultation with the patient, because patient compliance is essential to the success of the procedure. The EVE device is placed on the patient and activated in the office; it is tested for approximately 20 minutes to make certain that the patient can tolerate it.

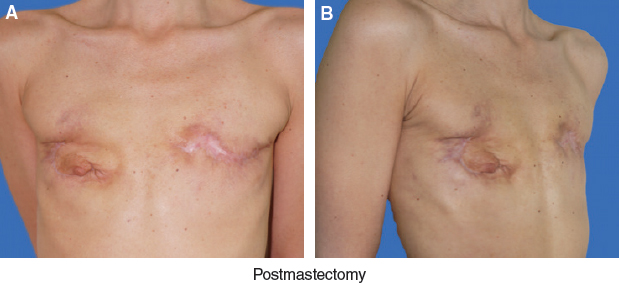
This patient shows how the EVE device is positioned and used by the patient. This woman had undergone bilateral mastectomy. The irradiated right breast required more grafting sessions; her left nonirradiated breast has already undergone an immediate reconstruction, external volume expansion, and autologous fat grafting (AFT).
The EVE device must be used with cycling pressures of 0 to 60 mm Hg for 3 minutes on and 1 minute off for 10 hours per day, starting 2 to 3 weeks before autologous fat grafting is performed. The minimum therapeutic dose is arbitrarily set at 200 hours to be accumulated over the approximately 15 days just before grafting.
This patient shows how the EVE process progresses during breast reconstruction. She is seen before and 3 weeks after external tissue expansion of her postmastectomy breast mounds.
Patients are considered ready for fat grafting when their breast mound volume is at least 2.5 times greater than their preexpansion volume. We educate the patient to understand that she is responsible for her results—the greater the expansion, the better the result. Fat will lodge and survive in a preexpanded scaffold, but it cannot expand the tissues and survive at the same time.
Surgical Techniques
FAT HARVEST
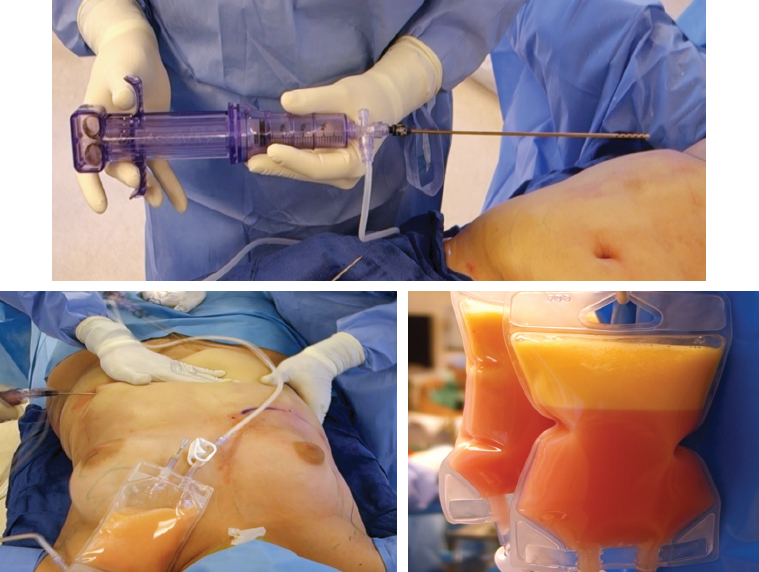
We use the Lipografter, K-VAC syringe, and AT valve (Marina Medical) devices, which maintain the aspirated fat in a closed system throughout the procedure. Two surgeons can harvest fat simultaneously, a major advantage. Above, two bags containing lipoaspirate are shown in two different stages; in the nearer bag the fat has been separating by gravity sedimentation for 10 minutes, whereas the posterior bag was just filled.
The identified donor sites are marked preoperatively. After general anesthesia is induced, the harvest areas are infiltrated with tumescent solution containing 1:100,000 of epinephrine until the tissues are very firm. We typically infuse 1 to 2 L per side per area to be liposuctioned. We attach the Lipografter to a 12-hole, 12-gauge cannula that is connected to the K-VAC syringe. The syringe provides a constant vacuum pressure of 300 mm Hg as it harvests fat, with no need to switch syringes or use multiple syringes at any point. The K-VAC efficiently and atraumatically drives the harvested fat into the sterile bag through the four-way atraumatic AT valve. 8 The fat remains in this closed system throughout; this minimizes its exposure to the environment and adheres to the accepted principles of fat grafting. As the fat is transferred to the sterile bag, at the same time the K-VAC syringe automatically gets recocked to create the constant 300 mm Hg of pressure.
LIPOASPIRATE PREPARATION
Once the sterile bag is filled with lipoaspirate to its total 200 cc capacity, it is centrifuged at 15 g for 1 minute, or it is allowed to separate by gravity (1 g) for 15 minutes. There is almost no free oil noted in the bag when this gentle technique is used. The tumescent fluid is drained out of the bag, and the fat is ready for grafting.
GRAFTING
This patient has been prepared for fat grafting, with markings on the skin to show the multiple planes and passes needed to distribute the fat evenly throughout the externally expanded mastectomy mound.
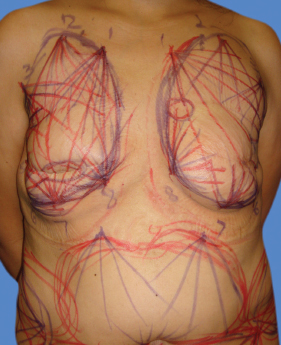
The increased recipient site volume after expansion provides the necessary additional grafting capacity. The amount of fat that can be grafted is determined by this added capacity and the mechanical compliance of the original recipient site. The grafted fat must be diffusely dispersed as a fine mist of microdroplets or as ribbons that are no wider than 2 mm and that do not coalesce into larger blobs, which could lead to necrosis. We therefore inject the graft through multiple 14-gauge needle puncture holes all around the mastectomy site. With this system of minute amounts of fat, we aim to achieve evenness through randomness. We prefer to use a single-hole curved cannula with a spatulated tip that follows the contour of the breast curvature; by keeping the tip pointing upward, this best prevents inadvertent chest wall puncture.
Microdroplets of lipoaspirate are delivered with a small 2.5 cc syringe using long passes of a 25 cm long, 2.4 mm diameter cannula. Delivering 0.1 cc/cm leaves behind 2 mm wide ribbons throughout the breast as the cannula goes through contiguous arcuate sweeping passes in multiple layers, from deep to superficial. The four-way AT valve allows the syringe to automatically draw the fat in from the bag, then back out through the grafting cannula. The economy of motion afforded by avoiding cannula switching and syringe reloading saves time while allowing the surgeon to precisely deliver the graft through small syringes.

The fat is dispersed from the same bag that was used to harvest the fat. This technique ensures even delivery and avoids large droplets, which can coalesce into lakes that may lead to fat necrosis or oil cysts.
It is crucial to avoid overgrafting which will lead to increased interstitial pressures that choke circulation and prevent revascularization of the fat. 12 – 13
Postoperative Care
On postoperative day 3 or 4, the patient will start to use the EVE device at a low constant pressure of 10 mm Hg for as many hours per day as can be tolerated for 3 to 4 weeks. The use of the device at this point helps create a three-dimensional stent to immobilize the fat grafts and keep the breast’s biologic scaffold in the expanded state. Alternatively, we place an immobilizing conforming adhesive splint over the breast to maintain the expanded, grafted state and to prevent it from deflating for a few weeks.
The entire process can be repeated after 2 or 3 months until the reconstructed breast mound has satisfactory projection. For bilateral reconstructions, the goal is to achieve a symmetrical result that satisfies both the patient and the surgeon. For unilateral reconstructions, the goal is to achieve symmetrical volume and contour with the contralateral breast. For irradiated breasts, there should be at least a 3-month interval between grafting sessions.
Additional Maneuvers
For breast tissue that is scarred, we employ the percutaneous aponeurotomy and lipofilling (PALF) procedure (see Chapter 44). This technique releases the contractures by percutaneously mesh-expanding the scars and grafting fat in the tiny three-dimensional gaps created by the needle release. The cicatrix becomes the matrix, and the hard, fibrous scar is softened by myriad fat micrografts lodged inside. Furthermore, the interspersed fat prevents the divided fibers from reconnecting, reducing the risk of contracture recurrence. 14
Delayed Reconstruction
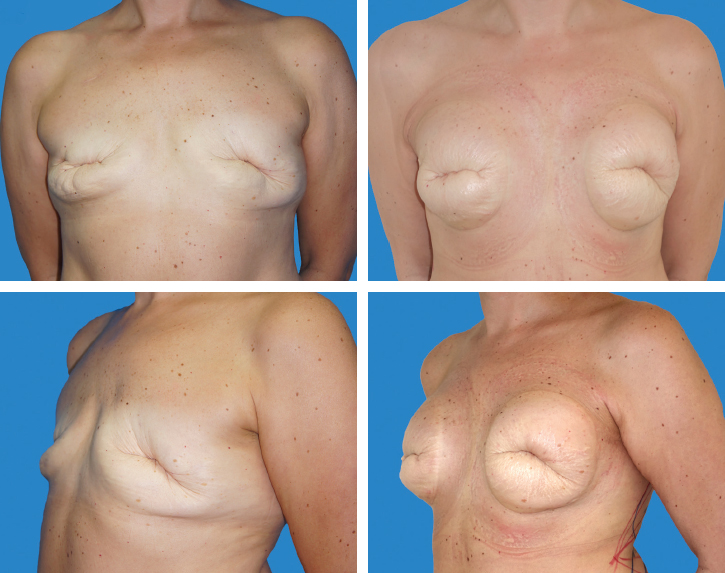
This patient underwent bilateral mastectomies and failed immediate implant reconstruction. She had a low BMI and presented with open wounds.
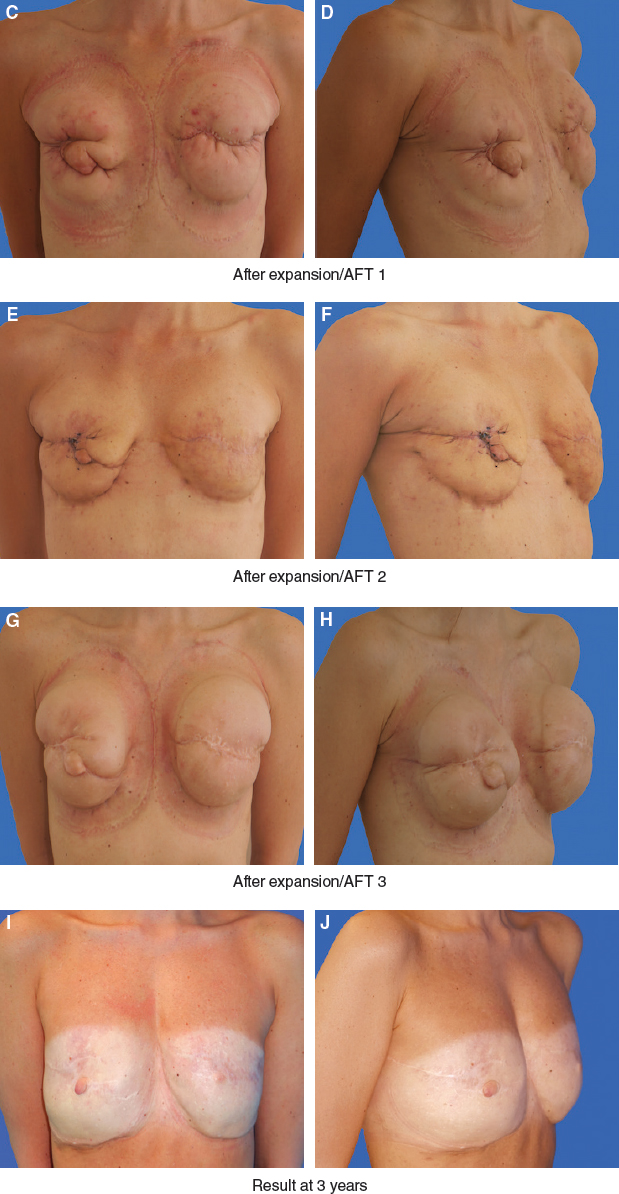
She underwent three sessions of external expansion plus AFT. Her results at 3-year follow-up show a healed and satisfactory result.
External expansion increases the volume of the mastectomy defect, enlarges the biologic scaffold, and stimulates the genesis of new stromal and vascular elements. External expansion allows more graft to survive per session and undoubtedly reduces the number of fat grafting sessions required for an acceptable whole breast reconstruction. 8
Many patients undergo mastectomy without immediate reconstruction. The last thing some of these women want to think about at the time of cancer treatment is undergoing another invasive procedure. Breast reconstruction with AFT lowers the acceptance threshold for mastectomy reconstruction at a later date. Delayed reconstruction is the safer option for patients who might undergo radiotherapy, because it would be a waste to irradiate the fat grafted tissue. In mastectomy patients who have undergone radiotherapy, poor tissue compliance limits expansion and restricts the amount of fat that can be safely grafted per reconstructive procedure. 15 – 16 It is not until the third grafting session that the tissue of the irradiated defect takes on a more normal structure and can be treated like the tissue of a nonirradiated mastectomy patient.
Immediate Reconstruction
Traditional fat grafting is a blind procedure: we cannot see the fat coming out of the cannula, and we are not sure that we are avoiding excess localized deposits. Immediate reconstruction provides a unique opportunity to perform three-dimensional grafting under direct vision.
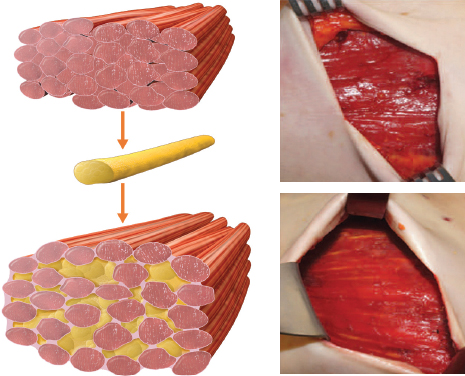
The technique of grafting into the pectoralis major muscle is shown, with clinical photographs of the thin ribbons of fat that are placed both intramuscularly and submuscularly.
The recipient site in standard fat grafting has a limited capacity. With the pectoral fascia removed, the muscle can swell to many times its original volume without increasing the interstitial tissue pressure. The pectoralis major muscle is completely exposed in this situation, and the plastic surgeon can graft autologous fat under direct vision to the entire muscle.
The idea is to graft fine ribbons of fat between the muscle fascicles (intramuscular) in multiple planes, from deep to superficial. Fat can also be deposited submuscularly, but one should always exercise caution to avoid penetrating the intercostal muscles with the cannula to prevent a pneumothorax. Depending on the size of the muscle, 100 to 400 cc of fat can be grafted immediately within the muscle, the lateral thoracic fascia, and, if possible, the base of the mastectomy flaps.
In contrast to traditional procedures, and somewhat counterintuitively, excess skin is a problem in AFT total breast reconstruction. Excess skin accordions into folds, with troughs that adhere to the chest and that become extremely difficult to release without creating ischemia or cavities where the fat grafts will die. The mastectomy skin flap closure should be loose, just right, and with no fold. In immediate AFT reconstruction, trimming or keeping the excess skin is a variable that is best controlled by the plastic surgeon.
Fat can also be grafted under direct vision into the subcutaneous tissues of the mastectomy flaps, especially in the upper pole, where the plastic surgeon can start to shape the breast. Patients will immediately have a small breast and can show some cleavage as the fat grafted pectoralis muscle swells up the medial and upper part of the thorax. This reduces some of the psychological trauma associated with mastectomies. If the patient’s tumor biology is such that she will undergo radiotherapy, immediate reconstruction is not offered, since the radiation will undoubtedly injure the grafted fat and compromise the results.
By 4 to 6 weeks after the mastectomy, the skin flaps have healed, the grafted fat has revascularized and is now adhered to the muscle, and the patient is ready for external volume expansion. To create a large enough biologic scaffold by expansion, a total of one to six additional procedures will likely be required to complete the entire whole breast reconstruction. One should adhere to the principles described in the sections on surgical techniques for each additional procedure and expansion.
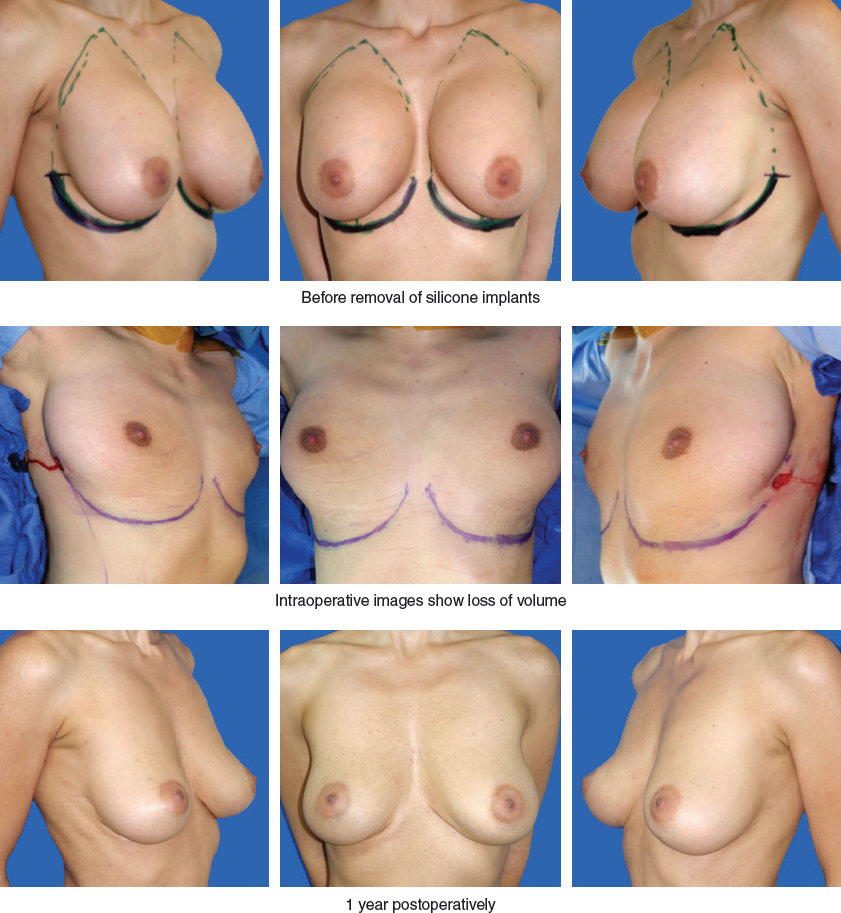
This woman requested removal of her silicone breast implants and immediate total breast reconstruction. Intraoperatively, the loss of volume after implant removal is evident. She underwent only one grafting session. Her result is seen 1 year postoperatively.
Another scenario in which immediate breast reconstruction with AFT can be achieved is when an implant is removed for a number of reasons, such as capsular contraction, infection, or other complications. In such cases, total breast reconstruction can be achieved in one AFT session, which is carried out in the same procedure in which the implant is removed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree