Chapter 40 LIPOMODELING FOR CONGENITAL BREAST DEFORMITIES: TUBEROUS BREASTS, POLAND SYNDROME, AND ASYMMETRY
It is not a new concept to transfer fat from a region of the body with excess adipose tissue, such as the abdomen and thighs, to the breast to enhance its shape and volume. The grafting of fat to the breasts has been used since the early days of liposuction procedures, mainly after the work of Illouz 1 and Fournier. 2 However, the earlier efforts did not fully meet the established goals, because the fat grafting techniques were less precise than those used today and often led to fat necrosis. At that time, fat necrosis was more challenging to identify, because breast imaging modalities were less definitive. A final blow to progress in refinement of the technique was delivered by the controversy following the work of Bircoll. 3 , 4 This polemic debate led to a recommendation by the American Society of Plastic and Reconstructive Surgery dissuading surgeons from further fat grafting to the breast 5 : “The committee is unanimous in deploring the use of autologous fat injection in breast augmentation; much of the injected fat will not survive, and the known physiological response to necrosis of this tissue is scarring and calcification. As a result, detection of early breast carcinoma through xerography and mammography will become difficult, and the presence of disease may go undiscovered.” This restriction by the ASPRS quelled research and experimentation in this field for a time.
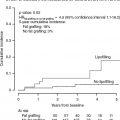
Interest was renewed following the work of Coleman, 6 , 7 who stated that fat grafting could be safely and efficiently performed if a meticulous preparation and transfer protocol was followed. Because fat grafting had proved very efficient for facial rejuvenation and for the correction of facial deformities, in 1998 we developed a research protocol to evaluate the efficacy of fat grafting in the thoracomammary region. This work allowed us to develop our own technique, which we called lipomodeling, 8 , 9 to confirm the value and tolerance of grafting to the breast 4 , 10 and to confirm that there were no deleterious clinical or radiologic effects. 11 – 13
When we first presented our work at the Société Française de Chirurgie Plastique et Reconstructrice and at international society meetings, our reports were the subject of criticism, with the same arguments used as in the 1980s controversy. We then designed scientific studies to address every argument pointby-point with scientific evidence. As we presented our work, hostility in the community began to decrease, and over time fat grafting to the breast became a well described and accepted procedure for breast reconstruction. 4 , 8 , 9 , 14 We then progressively expanded our indications to the thoracomammary region.
In this chapter we present the relevance of fat grafting for the treatment of asymmetries and congenital breast deformities and discuss the expected results of the lipomodeling technique.
Material and Methods
SURGICAL TECHNIQUE
We have used breast lipomodeling since 1998 in our department. We progressively developed an accurate technique allowing maximum efficiency of a large-volume fat transfer to the breast (megavolume transfer). Recent works also contributed to the standardization of the harvesting and transfer techniques, thus minimizing the hazards of each step. Precision in performing each step is the key to fat survival in the short, medium, and long term. 4 , 6 , 8 , 9
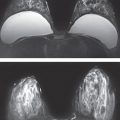
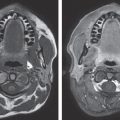
Before any lipomodeling procedure can be planned, the patient must be at her ideal weight, because transferred fat maintains a “memory” of its origin, and if the patient loses weight after lipomodeling, she will lose part of the benefit of its effects. Breast ultrasonography is always performed by a well-trained breast radiologist before surgery as a baseline, and another ultrasound is obtained 1 year after the last session of lipomodeling to be used as a reference. If the patient is more than 30 years old, mammography is added to this protocol. 12 , 13 The patient is thoroughly instructed before surgery about the procedure, the follow-up, and the need for preoperative and postoperative radiologic surveillance so that any newly arising or preexisting breast cancer will not be overlooked. 15
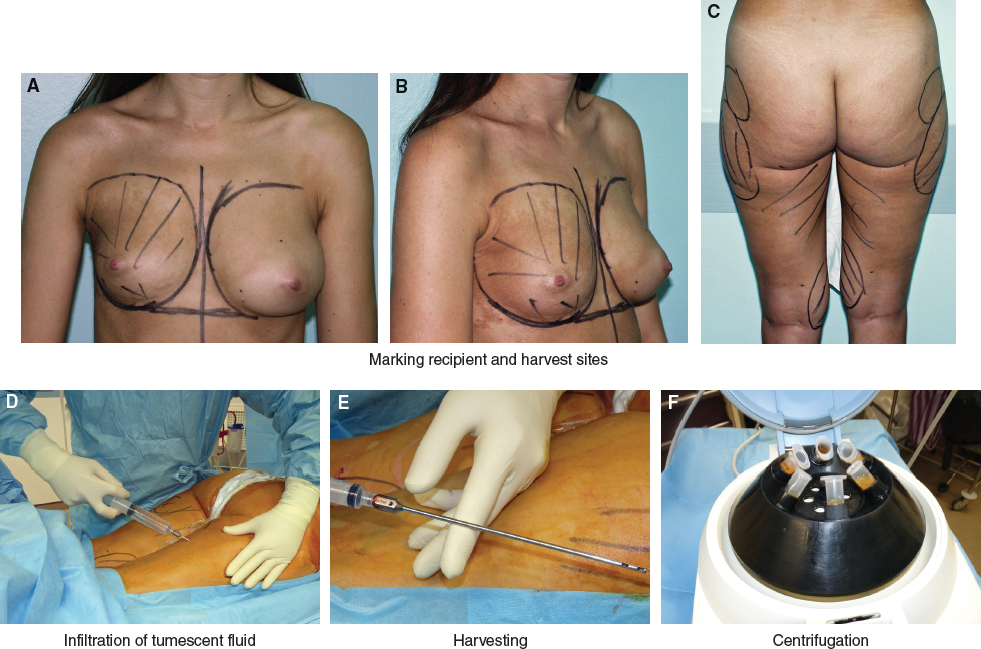
The surgeon must first evaluate the areas to be treated in the breast and thorax. These areas are marked with the patient standing. Then potential fat harvesting zones are evaluated to highlight natural fat deposits. Abdominal fat is generally the first choice of a donor site, because it does not require any position change during surgery. However, in teenagers or young adults, the fat volume of the abdomen can be limited. Second choices are the saddlebags and medial aspects of the thighs and knees. Outlines of harvesting zones are drawn with a surgical marker.
Because a significant amount of fat is typically needed for the procedure, general anesthesia is used for most patients. A classical prophylactic antibiotic is usually given preoperatively if another surgery is planned at the same time, as is usual in plastic surgery. Lipomodeling itself requires no specific antibiotic. Local anesthesia only is used for small corrections of potential residual imperfections.
In the fat donor sites, small incisions are made with a No. 15 blade. If abdominal harvesting is done, we use four periumbilical incisions. One lateral incision is added on each side if lateroabdominal areas and fat above the iliac bone are to be harvested. On the thighs, we use an incision in the buttock crease on each side, and often an incision on the medial aspect of the knees.
In the recipient sites, we try to conceal incisions in previous scars. To cross the numerous transfer tunnels, one has to make three or four incisions, with two of them located in the inframammary fold. Incisions are made by means of the cutting edge of an 18-gauge needle to limit their length.
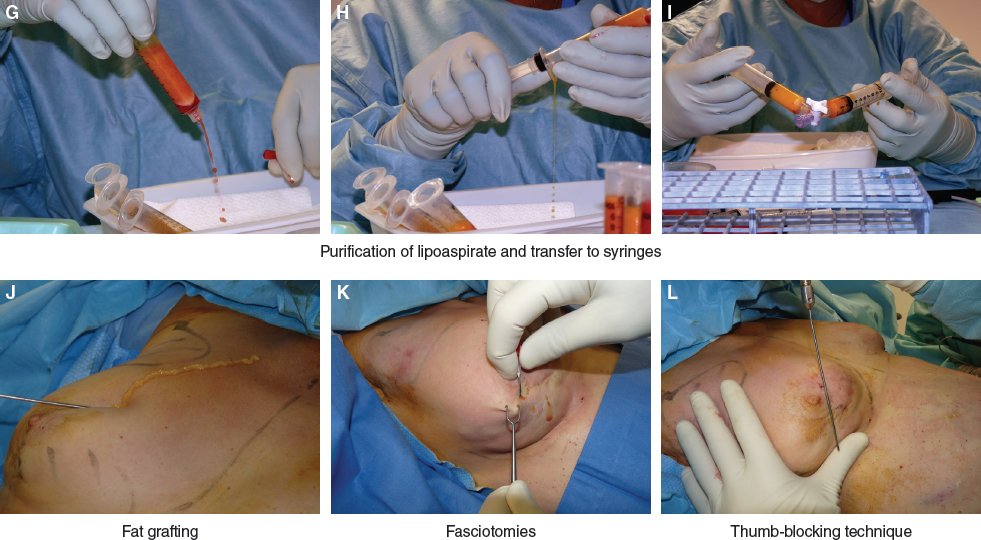
We use harvesting cannulas with blunt tips and five holes, with a diameter of 3.5 mm. Harvesting is done with a 10 cc Luer-Lok syringe attached to the cannula. Aspiration is performed with a minimal vacuum pressure and delicate handling so that adipose cells are not injured; violent mechanical aspiration can have a deleterious effect on cell survival. The total amount of lipoaspirate has to compensate for the loss of the waste fractions separated by centrifugation, as well as the necessary overcorrection during fat grafting. Incisions are closed with thin rapid-absorbable suture.
During harvesting, an operative assistant will prepare syringes for centrifugation: screw caps are placed on the syringes, which are then centrifuged at 3000 rpm for 20 seconds. The team must be well organized to handle fat properly and quickly. By means of the three-way valve, purified fat is transferred from the centrifuged syringes to 10 cc syringes.
At the completion of fat processing there will be numerous 10 cc syringes of purified fat. Fat grafting can then be done in the thoracomammary region with the 10 cc syringes on which a transfer cannula 2 mm in diameter is attached. These cannulas are slightly longer and stronger than the ones used for fat grafting to the face, because the mechanical demands of grafting in the breast are different. Breast incisions are made with an 18-gauge needle, which allows adequate access yet limits scar length, which will be a mere dot, hardly noticeable. More than one incision is made to allow multiple crisscrossing grafting tunnels.
The surgeon must have thorough knowledge of the anatomy of the thoracomammary region. Grafts are placed from the bony plane of the ribs to the cutaneous level, and it is very important to be aware of each tissue layer’s thickness. For correction of a congenital deformity, it is essential to evaluate individual variations in each layer on the surface of the projecting breast mound. A capacity for mentally visualizing these different layers in a three-dimensional grid is a valuable asset for the surgeon and relies on his or her surgical experience in breast surgery. The anatomy of the infraclavicular vessels and brachial plexus must also be well understood. Great care must be exercised while transferring fat to the upper thoracic region to prevent injury of the infraclavicular vessels or creating brachial plexus lesions. The depth of cannula insertion must be kept under strict control throughout multiple thrusts into the tissue.
Grafting is done in very small quantities in the form of ultrathin, spaghetti-like cylinders of fat in multidirectional microtunnels, working from the deep to the superficial plane. The fat is transferred as the cannula is withdrawn, not as it enters the microtunnel. A large lobule of fat must not be grafted or an excessive amount injected in the same level and zone, which would lead to fat necrosis. Each microtunnel should be placed so that it is enveloped by well-vascularized tissue.
The fasciotomy maneuver is a very important technique to consider when treating patients with a breast deformity. It is particularly useful for treating scar retraction and a lack of skin expansion. The technique consists of sectioning fibrous tracts that would prevent skin expansion. Fasciotomies must be done in several different levels to allow global tissue expansion without devascularization, which would predispose the tissue to fat necrosis. The technique consists of putting fibrous tracts under tension by pulling the skin with a double hook and cutting the fibrous tracts with the tip of an 18-gauge needle. 16
Lipomodeling requires overcorrection if the recipient tissues allow it, because a 30% volume resorption of fat (20% to 30%, depending on fat quality) can be expected. When the recipient site is saturated with fat and can accept no further lipoaspirate, grafting must be discontinued to avoid creating fat necrosis zones; this may be referred to as the principle of respecting recipient site saturation. Breast injection sites are closed with a thin fast-absorbing suture, and a simple dry dressing is applied for a few days.
The pain patients experience at the harvest sites will be the same as for any liposuction procedure. Patients complain of a sharp pain for the first 48 hours, which can be treated with simple analgesics. We infiltrate the region with dilute ropivacaine at the end of the harvesting procedure, which reduces the discomfort at the harvest sites during the first 24 hours. The patient will have an unpleasant sensation at these sites for 2 to 3 months. Bruising is significant and lasts for about 3 weeks. Postoperative edema resolves completely or almost completely within 3 months.
On the breasts, bruises last for approximately 15 days. Postoperative edema in the breasts resolves in about 1 month. Tissue volume will shift toward a progressive loss of about 30% of transferred fat, but the patient may have the impression that a 50% loss is taking place, because she saw the result the day after surgery when edematous volume was at its highest. This must all be discussed with the patient preoperatively, with assurances that her breast volume will stabilize after 3 to 4 months.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree