Chapter 20 SCLERODERMA AND FAT GRAFTING
Systemic sclerosis (SSc) is an orphan systemic autoimmune disease characterized by progressive microvasculopathy and fibrosis that both contribute significantly to morbidity and mortality. Prevalence of SSc in Europe, depending on the diagnosis criteria used, is estimated to be 1.26 to 1.58 cases/10,000. SSc consistently occurs more frequently in women, with a mean sex ratio of approximately 3:1. The peak of incidence is usually during the fifth decade of life.
The vasculopathy results from a chronic vasomotor imbalance leading to vasoconstriction, endothelial damage, proliferative vasculopathy, capillary destruction, and adventitial fibrosis, with subsequent luminal obliteration. In response to the microvasculopathy, appropriate vessel formation or repair does not occur. The microvascular disorder of SSc precedes and favors the inflammatory response and fibrotic process with proliferation of fibroblasts and differentiation into myofibroblasts secreting high amounts of extracellular matrix proteins. The fibrotic process involves not only skin but also internal organs, leading to deteriorating organ function. 1
Research efforts have been aimed at preventing and treating life-threatening complications that arise from the effects of SSc on the internal organs, particularly pulmonary arterial hypertension (PAH), pulmonary fibrosis, and renal crisis.
In general, vasodilators such as calcium channel blockers, nitrates, and PDE5 inhibitors are considered first-line therapy. Other vasodilator drugs such as endothelin receptor agonists (ERAs) and prostaglandin analogs (iloprost, prostacyclin) can be used for Raynaud phenomenon when first-line medications fail, but are often used as first-line treatment for pulmonary arterial hypertension. In interstitial lung disease/pulmonary fibrosis, immunosuppressive drugs are recommended, including cyclophosphamide, mycophenolate mofetil (MMF) or azathioprine. First-line therapy for scleroderma renal crisis (SRC) is based on angiotensin-converting enzyme inhibitors (ACEi). 2
As a consequence, mortality in SSc disease has dramatically decreased in recent years. Thus patients now request treatment of the lesions of the face and hands that are almost always present. These are a source of social discomfort and disability, and they are not improved by drugs. To date, therapeutic interventions in this disease are mainly based on the use of vasodilators for Raynaud phenomenon and digital ulcers. Bosentan (Tracleer), an ERA, may be prescribed to prevent ischemic digital ulcers. Unlike other autoimmune diseases, steroids and other immunosuppressive drugs have limited clinical benefit in SSc. No therapy has been shown to reverse or slow the progression of tissue fibrosis or substantially modify the natural progression of the disease. 3 – 8
Significant renewal of interest in the use of fat grafting for the restoration of all volume defects was observed after the initial description of the LipoStructure technique by Coleman (see Chapter 1). In this chapter, we present the literature and our clinical approach using autologous adipose tissue in the treatment of the face and hands in patients with SSc.
Fat Grafting: A Promising Option for Treatment of the Face in SSc Patients
Involvement of the face with associated oral complications, aesthetic changes, and impairment of the patient’s self-image is found in more than 90% of patients with SSc. 9 – 12 The face becomes amimic, cutaneous wrinkles disappear on the forehead, vertical furrows develop around the mouth as a result of retraction of the skin, and the nose becomes sharp. Face and mouth changes also include lip thinning, reduction of both the width of the mouth (microcheilia) and opening (microstomia), and xerostomia. These changes interfere with eating, speaking, and oral hygiene measures. Dental problems are common in people with SSc for a number of reasons: tightening of the facial skin can make the mouth opening smaller and narrower, which makes it hard to care for the teeth; dry mouth caused by salivary gland damage speeds up tooth decay; and damage to connective tissues in the mouth can lead to loose teeth. Facial manifestations are disfiguring and lead to functional, aesthetic, and social discomfort. The high frequency of these manifestations, as well as the functional disability and aesthetic burden they induce in patients, underscore the need to offer therapeutic options that have been crucially lacking to date. Fat grafting has been used for the treatment of other sclerotic conditions, including localized scleroderma.
In 2015 Del Papa et al 13 first reported the benefit of fat grafting using the classic Coleman method to treat fibrotic perioral changes in 20 SSc patients with a cutaneous diffuse form. After fat harvest and centrifugation, 2 cc of processed lipoaspirate was injected in 8 different sites around the mouth using a blunt cannula. This minimally invasive surgical procedure was reported to have a good safety profile. Three months after treatment, both the interincisive teeth distance and oral perimeter significantly increased in these patients.
The special context of SSc requires some modifications to this approach, in particular the use of harvest and implantation of smaller parcels of adipose tissue. 14 Thus micrografting represents an evolution of the art. Fat is harvested with a 2 mm (14-gauge) cannula with openings of less than 1 mm, which harvests fat lobules of about 600 microns. Processed lipoaspirate is then injected using a 0.8 mm (21-gauge) placement blunt-tipped cannula. The entire procedure is performed with the use of local anesthesia (supplemented with conscious sedation if needed) and can be performed either on an outpatient or inpatient basis.
SURGICAL TECHNIQUE
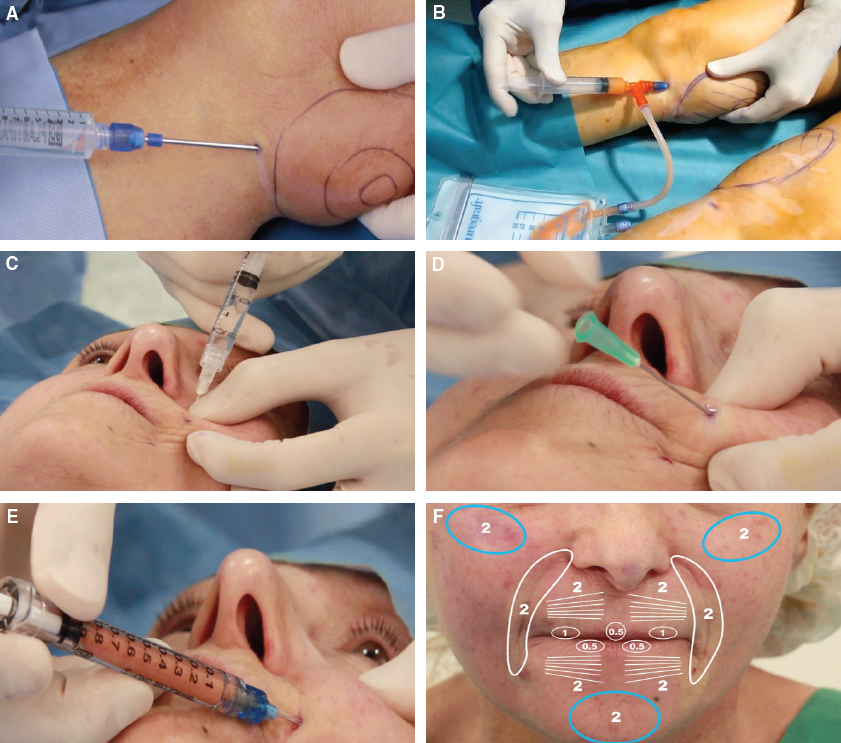
The steps of fat micrografting for the treatment of SSc of the face are shown. Local infiltration is done, in this case, in the inner aspect of the knee (a preferred site for harvesting) (A). After an interval in which the lidocaine takes effect, microharvesting is performed with a closed system (B). The lipoaspirate is processed (as described under Purification). A local anesthetic is injected in the affected areas of the face (C), and the entry point is punctured with a 21-gauge (0.8 mm) needle (D). Micrografting is performed with a 1 cc syringe and a 21-gauge (0.8 mm) cannula (E). The fat placement and quantities in this patient (total 21.5 cc) are shown (F).
Sampling and Infiltration
The first step is anesthesia of the entry point with a 3 cc syringe and a 30-gauge needle. An incision is then made with a 14-gauge needle before inserting the infiltration cannula of the same diameter (14-gauge, 2 mm). For infiltration, we use a modified Klein solution containing 800 mg of lidocaine and epinephrine 1:1,000,000 with a wet technique. Typical harvesting areas include the abdomen, hips, and inner knees; our preferred location for small quantities is the inner side of the knees. Aspiration is performed using a 10 cc syringe with less than 1 cc of vacuum (less than 300 mm Hg).
Purification
Two techniques can be used for purification of the product:
The standard for fat graft processing has for a long time been based on centrifugation. For microfat grafting technique, we recommend 1 or 2 minutes of centrifugation at 1200 g. The lower fraction containing the infiltration liquid is removed. In our experience, there will be minimal oil from disrupted fat cells.
Filtration with the PureGraft closed membrane filtration system (PureGraft, Solana Beach, CA) can be used as an alternative. Tumescent fluid, blood cells, debris, and oil are removed by this system, leaving filtered, purified, living fat.
With both techniques, the pure fatty tissue is transferred through a Luer-Lok adapter from the 10 cc syringe into multiple 1 cc syringes for grafting. To prevent air bubbles, a connector is first placed on the 10 cc syringe and primed with tissue before connecting to the 1 cc syringe.
Placement
The entry points are anesthetized. The skin barrier is punctured with a 21-gauge needle (0.8 mm diameter) in the same direction in which the mini-cannula will be introduced (21-gauge, 0.8 mm). Adipose tissue can be injected in all areas, but especially in the superficial plane, as close to the skin level as can be achieved without risk of irregularities. The tissue can be implanted in several planes and in different directions. The micrografts are approximately 500 microns and contain only a few hundred cells.
RESULTS

The results for three SSc patients who underwent microfat grafting are shown at 6-month follow-up. In this 47-year-old patient with a diffuse cutaneous form of the disease, microfat grafting improved her ability to open her mouth (A and B). A 58-year-old patient with a limited cutaneous form of the disease (C and D).
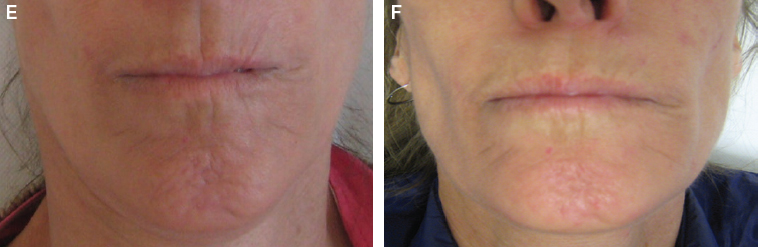
A 51-year-old patient with a diffuse cutaneous form both show a decrease in the vertical furrows around their mouths caused by retraction of the skin and trophic effects (E and F). The aesthetic improvement is evident in each woman.
The minimally invasive fat grafting technique was used to treat the faces of 14 patients with SSc (8 with limited cutaneous forms) with facial handicaps defined by the Mouth Handicap in Systemic Sclerosis Scale (MHISS) with a score equal to or greater than 20, a Rodnan Skin Score of the face equal to or greater than 1, and maximal oral opening of less than 55 mm. The outcomes are summarized in the table. 15 No infectious complications related to the procedure were recorded. After liposuction, small areas of bruising at the zones of fat harvest were observed in 8 patients and local pain reported in 3 patients. Concerning the perioral fat injection, small areas of bruising were observed (n = 3), pain (n = 3), perioral sensitive manifestation (n = 1) and trigeminal neuralgia (n = 1), which spontaneously resolved in a few days. We observed a significant decrease in the mouth handicap score (MHISS) at 3 and 6 months after the procedure. Secondary efficacy parameters evaluating perioral skin sclerosis with the Rodnan Skin Score applied to the face, maximum oral opening, sicca syndrome (assessed with the xerostomia inventory questionnaire and the sugar test), and facial pain (assessed with a Visual Analog Scale) also significantly improved at 3 and at 6 months. Thus this minimally invasive approach offers new hope for treatment of the face in SSc patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree