Chapter 18 SCAR REMODELING WITH FAT GRAFTING AFTER BURN INJURY
Problems Associated With Burn Scars
Patients who survive second- or third-degree burns in which significant burn surfaces and important areas of the body are involved will have functional and aesthetic complications that constitute social, economic, and psychological problems. Despite the scientific efforts made in an attempt to relieve these problems, long-term outcomes and scars can be poorly improved. The most frequent problems of healed severe burns are hypertrophic scars, contractures, itching, heterotrophic ossification, neuropathies, and pain.
Facial burn contractures may cause microstomia, lip defects, ectropion, and loss of facial expression, whereas on the neck, hands, feet, and armpits there may be a reduction of passive and active range of motion as a result of retractile scars. Furthermore, despite healing of burned areas, there may be persistent itching in 15% and potentially as much as 44% of patients, 1 sensory problems (paresthesias) in 82% of patients. 2 Ongoing pain, sweating, and thermoregulatory difficulties have been documented. 3
Therapies used to date, such as surgery (early removal of the burned areas and skin grafting, traditional Z and V-Y plastic and tissue expansion), 4 physiotherapy and pressure therapy (pressure garments and splinting), 5 the use of film and silicone bandages, 6 injection of corticosteroids, 7 and laser therapy 8 have produced results that are limited and unpredictable, with a high relapse rate. The use of radiotherapy 9 and administration of medications such as colchicine 10 and interferon 11 are still controversial. Fat grafting provides a promising new approach to this intractable problem.
Rationale for the Use o f Fat Grafting in Burned Patients
Treatment of deep burn injury scarring is particularly difficult because of the presence of significant tissue fibrosis, retractions, and scar contractures, hypertrophic areas, and keloids. In addition, there are changes in the normal pattern and coloring of skin resulting from infective and inflammatory processes caused by toxins and proteases that alter and damage the normal wound healing process. 12 Histologic examination of a burned tissue sample shows the presence of fibrotic tissue in the reorganization phase with no significant signs of regenerative activity; cell activity seems absent, as in a necrotic process.
We decided to use the fat grafting technique to treat burn scars for the following reasons:
Fat grafting in the face and neck with moderate shrinking has been found to correct cicatricial contraction. 13
An improvement in retraction and scar contraction has been demonstrated experimentally in wounds treated with autologous fibroblasts. 14
The use of injected lipoaspirate in patients with chronic degenerative problems resulting from radiotherapy has provided promising outcomes. 15
The Role o f Stem Cells
Regenerative medicine and tissue engineering are developing in concert with recent progress in biotechnologies, and there is great promise for the potential to repair damage to the mesoderm by combining biomaterials, growth factors, and stem cells. 16 , 17
Stem cells have the capacity to self-replicate with long-term vitality and the potential to originate and differentiate into more than one cell population. Well-known stem cell sources are embryonic cells and bone marrow–derived adult cells. The use of embryonic stem cells has ethical and political limitations, whereas adult cells present problems for morbidity, postharvest pain, and a limit on the number of cells obtainable. 18 Adipose mesenchymal tissue, just like bone marrow, was recently identified as an ideal source of adult stem cells. In fact, recent studies show how the lipoaspirate and purified fat according to the Coleman protocol contains a pool of mesenchymal stem cells with differentiation potential in more than one cell line. These offer the highest percentage of adult stem cells in the human body: approximately 5000/g of fat compared with the 100 to 1000 stem cells/mm 3 of bone marrow. It is possible to isolate approximately 350,000 preadipocytes from 1 g of fat. 19
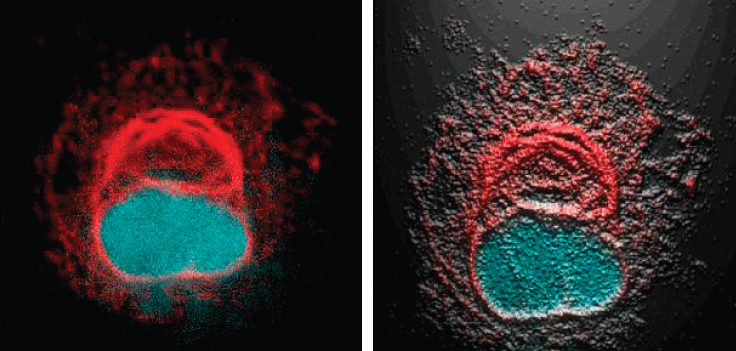
This microscopic photo of a stromal cell with antivimentin/Cy3 (red) and DAPI (blue) is from an abdominal lipoaspirate sample obtained via the Coleman technique. The original image is on the left (magnification 100×); on the right, it has been enhanced with image-improving software to show the filaments organized and wrapped like a ball near the core.
Treatment with mesenchymal adult stem cells is a new and promising therapy proposed for the repair of damaged tissue. In fact, bone marrow–derived or fat-derived adult stem cells may be of different cell phenotypes, such as bone, fat, cartilage, muscle, skin, and nerve tissue. Reported experiences on the use of bone marrow–derived adult stem cells for the treatment of limb ischemia, 20 ischemic myocardium, 21 retina, 22 and incontinence 23 are encouraging.
In our experience, centrifugation using the Coleman protocol is the ideal processing method to obtain a final product of purified and enriched fat with higher regenerative properties. To confirm this fact, we conducted a clinical trial comparing the centrifuged samples obtained by Coleman’s technique with noncentrifuged samples, focusing on cell viability, the content of adipose-derived stem cell (ADSC) populations, and the frequency of clonogenic precursors. 24 The results of our study showed that centrifugation produces a viable cell population significantly enriched in mesenchymal and endothelial progenitors, with a higher clonogenic potential than noncentrifuged samples. In addition, centrifuged fraction samples had a lower content of contaminants, such as oil and blood cells, which may have a relevant influence on graft take. Thus centrifugation concentrates a higher number of viable cells with regenerative potential in a smaller amount of inoculum, making this method ideal for the treatment of retracted scar tissue.
Study Design
Our experience began in December 2005 when we first treated three patients with fat graft injections. 25 To date we have treated nearly 1000 patients with structural fat grafting who had either mature or immature scarring caused by second- and third-degree burns. We started with a total study population of 160 patients recruited and treated through structural fat grafting. For each we performed a detailed clinical evaluation, classified their scars according to the Vancouver Scar Scale, 26 and performed a series of routine preoperative examinations. The study subjects then underwent fat liposuction with local anesthesia using sterile technique.
Before the initial surgical procedure, punch biopsies were performed in the burn scarred areas as well as in the healthy surrounding tissues as a control. The samples were fixed in paraffin and colored with hematoxylin-eosin to aid assessment of the structural features of the tissues, the distribution of the collagen, and vascularization. Nuclear MRIs, with and without contrast agent, of the burned area was performed before and after the treatment to evaluate the dermohypodermic layer of the burned areas, particularly the areas in which purified fat containing ADSCs had been injected. 27
In some patients, the same surgical procedure was repeated after 3 to 6 months. Before the second intervention, an MRI was obtained. During the intervention, punch biopsies and histologic examination were performed, as previously described. Three months afterward, punch biopsies and an MR scan were obtained; 3 to 6 months later, some patients underwent a third, fourth, or fifth similar operation.
In addition to this study population, we performed a parallel analysis on a subgroup of 20 patients submitted to a clinical assessment, adopting the Patient and Observer Scar Assessment Scale (POSAS) and durometer measurements to objectively demonstrate that autologous fat grafting does improve scar quality. We excluded patients with scars retracted above bony surfaces (such as the anterior tibia, patellar region, or elbow) so the durometer results would not be distorted. The RexGauge durometer type 00 (RexGauge, Buffalo Grove, IL) is a spring instrument for measuring skin hardness, with a 5 mm diameter round noninvasive gauge head and a value range of 0 to 100. This instrument has been widely used to evaluate sclerodermic skin, but it has been adopted in some clinical trials as an objective evaluation tool of scarred tissue. In these patients, the scar was virtually divided into two parts: a part of the scar was treated using fat grafting (the study portion) and the other part of the scar was infiltrated with saline solution (the control portion). 28
Technical Guidelines
ANESTHESIA
The area chosen for liposuction was the abdomen, because it is easy to access with the patient lying supine and because it contains a significant quantity of adipose tissue in most individuals. After the preliminary cut of the skin using a No. 11 blade near the umbilicus, a Coleman blunt-tipped cannula was inserted in the chosen area to inject 100 ml of cold physiologic solution with 10 ml of levobupivacaine 7.5 mg/ml, 20 ml of mepivacaine 10 mg/ml, and 0.5 ml epinephrine 1 mg/ml. This infiltration ensures good hemostasis and postoperative analgesia.
HARVEST
We performed fat harvesting and purification according to the Coleman technique, as described in Chapter 1. Fat is harvested using a 2 to 3 mm cannulas of variable lengths (15 to 23 cm) with a blunt tip connected to a 10 cc Luer-Lok syringe. A slight negative pressure is created inside the syringe itself while the tube is pushed in and out of the donor’s abdomen with circular movements. The surgeon must take care not to perform repetitive thrusts in the same area to avoid creating a local deformity.
Next, the lipoaspirate is centrifuged at 3000 rpm for 3 minutes. On average, the injectable tissue obtained through this procedure, depending on the patient’s individual habitus, will be approximately 30 to 40 cc. The purified fat contains ADSCs, which remain in their natural three-dimensional scaffold; these will promote reconstruction of a microvascular bed. 29 This injectable fraction is transferred from a 10 cc syringe to a 1 cc Luer-Lok syringe, which allows precise control of the amount of injected fat and facilitates ease of handling.
PLACEMENT
At the beginning of our practice, purified fat was injected in small parcels through a small incision in the skin, creating lines of injectate about 7 to 9 cm long (using a 0.1 or 0.2 mm Coleman blunt infiltration cannula) in the dermohypodermic joint of the burn-scarred areas, but we soon realized that a using a less-blunt cannula could produce more control for placement in the immediate subdermal plane in the burn-scarred areas. Scar tissue is characterized by abundant fibrous tissue, with significant resistance to the sliding of blunt cannulas. For this reason, more recently we have adopted the use of an 18-gauge angiographic needle with a snap-on wing (Cordis/Johnson & Johnson, Roden, The Netherlands) to inject the adipocyte fraction. Today we consider needles essential for treating scar tissue 30 and performing a quick, safe, and painless procedure that will achieve a better outcome. By changing to an 18-gauge angiographic needle, we have been able to overcome the characteristic resistance of burn-scarred tissue.
Using a highly precise technique, we deposit a consistent amount of fat at the dermal-hypodermal junction with multiple radiating passages to distribute fat in all directions, creating an ideal web to support damaged areas of tissue. We believe that a sharp cannula stimulates new collagen deposition and remodeling of fibrous tissues, in a fashion similar to the “needling” procedure used in aesthetic medicine. Moreover, with these 18-gauge angiographic sharp needles, a rigottomy is easier to be perform, if necessary (see Chapter 20). These needles are available as low-cost disposable devices and thus are more cost effective than classic reusable blunt cannulas.
In contrast to Coleman’s reports, our clinical experience has been focused primarily on correction of scar tissue, and we find needles are fundamental to the effective treatment of fibrotic scars and correct injection of autologous fat in the appropriate planes.
The quantity of fat injected at every passage is quite small—0.1 cc—to avoid formation of irregularities and lumps. If irregularities do occur, these are immediately resolved by digital manipulation. Injection of such small aliquots of transplanted fat reduces the risk of necrosis, calcifications, and cysts. Lysis of scar tissue is obtained by two different methods: (1) pushing the plunger of the syringe and exploiting the strength of exiting fat to overcome the fibrous tissue’s resistance, or (2) using a retrograde technique, injecting the needle for its entire length at the dermal-epidermal junction and then, while extracting the needle, releasing the fat. A small space (less than 1 mm) is left between the tunnels of fat transplantation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree