Case 17 Cleft Palate

17.1 Description
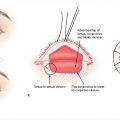
Photo reveals a submucous cleft palate
Bifid uvula
Zona pellucida: Diastasis of levator muscle with notable thinning of soft tissue at the midline, especially with elevation of the palate
Patient is phonating with anterior displacement of levator muscles (inverted V)
17.2 Work-Up
17.2.1 History
Pregnancy, birth, and newborn history
Prenatal care and exposures (alcohol, smoking, anticonvulsants, corticosteroids)
Gestational age of the newborn at birth (e.g., preterm, term, and postterm)
Family history of orofacial clefting
Additional medical problems
Cleft palate without cleft lip: 40% incidence of syndromic presentation
Airway concerns
Consider Pierre Robin sequence (Chapter 18) if small jaw and airway obstruction
Feeding and weight gain history
17.2.2 Physical Examination
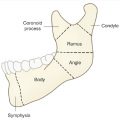
Classify the extent of cleft and structural involvement
Complete (i.e., soft and hard palates) or incomplete (i.e., soft palate alone)
Primary and/or secondary palate (dividing point is the incisive foramen)
Unilateral or bilateral (vomer visible on one or both sides)
Cleft lip involvement, if any
Veau cleft palate classification system (Table 17.1)
Evaluate for facial dysmorphic features and other congenital anomalies
Cleft palate alone (without cleft lip): 40% incidence of syndromic presentation
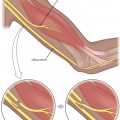
Mandible evaluation: Pierre Robin sequence—micrognathia/retrognathia, glossoptosis, and airway difficulties (see Chapter 18)
Head-to-toe examination for other anatomic abnormalities
17.2.3 Pertinent Imaging or Diagnostic Studies
Evaluate other organ systems (e.g., echocardiogram, renal ultrasound, X-rays of the spine) if there is suspicion for other congenital anomalies or syndrome.
Perform genetic testing if syndrome is suspected, possible through chromosomal microarray analysis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree