Chapter 6 Care of outpatient burns
![]() Access the complete reference list online at http://www.expertconsult.com
Access the complete reference list online at http://www.expertconsult.com
Introduction
During the past four decades there has been a remarkable improvement in the outcome of burn injuries and a progressive decline in its incidence. In the United States, this process began with the development of specialized burn treatment units, the first at the Medical College of Virginia, now the Virginia Commonwealth University Medical Center, and then at the US Army Institute of Surgical Research, Brooke Army Medical Center, San Antonio, Texas, both in 1947. There are now 125 units/centers in the USA.1 The improvement in outcome in the treatment of burn patients accelerated following the formation of the American Burn Association in 1967. According to the American Burn Association’s 2007 Fact Sheet, using information derived from a variety of sources, each year, in the USA, there are now approximately 500 000 individuals who sustain a burn injury requiring treatment from healthcare professionals.2 The annual incidence of burn victims has declined from an estimated 1 million each year during the 1960s. Fagenholz and colleagues documented a decrease in the incidence of visits to Emergency Departments for burns during the period 1993–2007.3 Currently, among those who sustain a burn, approximately 40 000 are admitted to hospitals for their care and there are approximately 4000 fire- and burn-related deaths each year.2 Therefore, thermal trauma typically results in an injury of low mortality in which the majority of care can be safely rendered in an ambulatory setting.
Who can be managed as an outpatient?
When a patient with a burn is first evaluated, information is immediately available from which an accurate prognosis can be derived. For instance, a valuable easily remembered estimate of the probability of death from burn injury was published in 1998.4 Using stepwise logistic regression analysis of 1665 patients, the authors identified three risk factors for death: age greater than 60 years; burns on more than 40% of the total body surface area (TBSA); and, the presence of inhalation injury. The mortality prediction for the presence of none of these risk factors is 0.3%; for the presence of one risk factor it is 3%; for two it is 33%; and, for all three it is approximately 90% (actual, 87%).
Age
Patients between 5 and 20 years of age have the most favorable survival outcome from burns. The LA50 (percentage of total body surface area at which 50% of the patients live and 50% die) for this age cohort is 94.5% TBSA of burn.5 Younger individuals, especially infants, have an increase in morbidity as well as mortality from burn injury. In this age group, child abuse or neglect must be included in the psychosocial analysis.6,7 The peak incidence of non-accidental burn injury is 13–24 months of age.8 Burns that are particularly suspicious are those whose appearance suggests an injury from a cigarette, hot iron, or immersion in hot water. The latter injury is identified by a stocking/glove distribution of the burn and a sharp linear demarcation between the burned and unburned skin (Fig. 6.1). Scalding which has occurred in an institution or in the presence of a caregiver other than one who has a biological relationship to the victim should also heighten one’s suspicion. Even with trivial injury, if the burn was sustained under suspicious circumstances or the history does not correspond with the nature or distribution of the burn, the patient should be admitted to a hospital for their protection. Cases of suspected abuse, neglect or bad parenting must be referred to the appropriate social services agency.
The author has become aware that in some instances being investigated for non-accidental trauma, the actual cause was from bad parenting and not done with malicious intent. However, when investigated, for a variety of reasons, e.g. immigration status, prior felony conviction, previous report to or concern of the local county authorities, the individual lied about the details of how the injury occurred. In a more unusual instance, a third person tries to protect the perpetrator, e.g. a mother protecting her daughter, when the daughter was the perpetrator of the injury to a child. Any patient over the age of 70 years with burns is in danger of dying regardless of the extent of the burn. The LA50 for this age group is 29.5% TBSA of burn.5 Therefore, admitting the older patient to a hospital to assess their response to the injury can prove invaluable before treatment is continued as an outpatient.
Extent of the burn
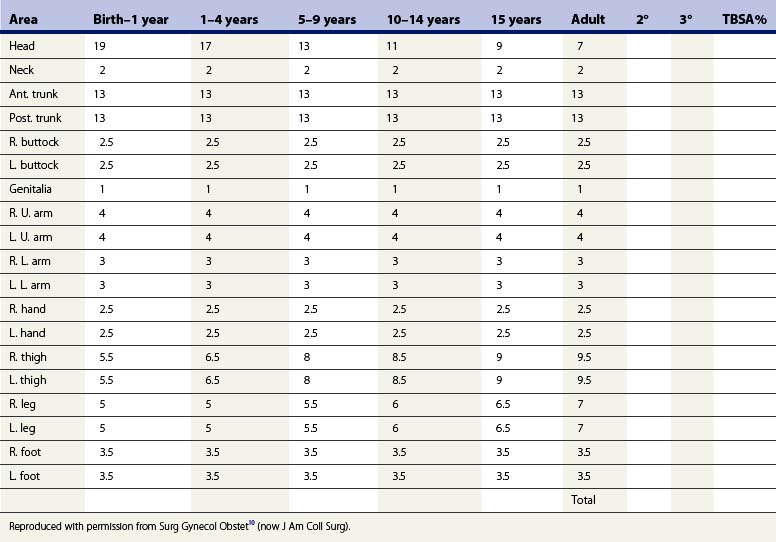
The larger the percent of body surface area involved by the burn, the worse the prognosis. The percent of the body surface area can be roughly estimated by using the ‘rule of nines’9 or more accurately by the technique of Lund and Browder (Table 6.1).10 A helpful adjunct in estimating the area of burn is to use the surface area of the patient’s hand. This area, which approximates 1% of the TBSA, includes the palm together with the fingers and thumb extended and adducted.
Any burned patient who requires intravenous fluid resuscitation should be admitted to a hospital. This includes adults and older children with burns in excess of 15% of the body surface area, as well as younger children (under 5 years of age) and infants with burns in excess of 10% of the body surface area.11 In some instances, due to premorbid dehydration caused by physical activity, an arid or semi-arid climate, alcohol, or diuretics, some patients with smaller burns may need supplemental intravenous fluids for optimal care. In the author’s practice, patients with small area burns that need intravenous fluid are often held for several hours or overnight in an observation area in the Emergency Department until their pain is controlled and fluid needs are met. Then care can often be continued as an outpatient.
Depth of the burn
When a burn is first evaluated it is often difficult to determine its depth. The superficial injury of sunburn or its equivalent is easy to identify. Likewise, it is easy to discern a waxen, dry, inelastic, insensate, cadaveric-appearing wound as a full-thickness burn. However, it is difficult to distinguish the subtle differences between a superficial partial-thickness burn, which will heal spontaneously within 3 weeks, and a deeper partial-thickness burn that will take longer to heal. This is especially true for weeping wounds in which the blisters have ruptured. Initially, these wounds appear superficial and are perfused. However, with time, as the injured small blood vessels in the wound thrombose, the wound takes on an ischemic, cadaveric appearance of a deeper injury.12,13 This change does not reflect invasive infection but merely the natural evolution of the wound.
Premorbid diseases
Preexisting medical conditions often have a profound influence on the clinical course and outcome of a burn injury. While any medical disorder may have an adverse effect, there are a number of conditions that occur frequently among the burned and which may play a significant role in causation or outcome. For instance, any condition or habit that alters an individual’s mental state may lead to a burn injury. These include seizure disorders, senility, and psychiatric illnesses as well as the use of sedatives, controlled substances, illegal and recreational drugs, and alcohol. These usually obligate hospital admission. Medical conditions that are known to enhance morbidity of patients with burns include renal failure, congestive heart failure, cardiac dysrhythmias, hypertension, chronic obstructive pulmonary disease, diabetes mellitus, sequelae of alcoholism, morbid obesity, conditions which require the use of steroids, and other diseases which compromise the immune system.14 The clinical status of any of these disorders must be determined and their potential influence on the outcome assessed before determining whether the patient can be safely managed as an outpatient.
Co-morbid disorders
Respiratory complications
Inhalation injury and carbon monoxide poisoning substantially magnify the burned patient’s risk and may occur even with no or trivial cutaneous injury.15,16 In addition, upper airway obstruction can be caused by the edema produced from burns of the oropharynx or the flux of fluid into the soft tissues of the upper airway resulting from deep burns of the face and/or neck. The full-blown adverse sequelae of these complications may not be immediately apparent.17 Therefore, if the history of the accident or distribution of burns suggests any of these three complications, a period of monitored observation is warranted. Overnight observation is usually sufficient.
Distribution of the burn
The location of the burn may have a profound effect on the patient’s activities of daily living, and dictate the setting in which the patient receives care. For instance, the edema from a small-area superficial burn of the face may result in swelling of the eyelids, hampering the patient’s vision (Fig. 6.2), or burns that involve the lips or the oral cavity may inhibit efficient oral alimentation. Likewise, burns of the hands, feet, or those involving the perineum or adjacent areas may severely limit an individual’s autonomy. While burns in these areas may not necessarily demand care in a hospital, there must be consideration of the assistance available to the patient when contemplating outpatient ambulatory care.
Because of fluid flux into the tissues beneath a burn, patients with circumferential burns of an extremity are in danger of ischemia of underlying and distal tissues from increased tissue pressure.18 Except for those with very superficial burns all patients with circumferential burns of an extremity should be monitored for evidence of elevated tissue pressure. Since the clinical signs of compartment syndrome and ischemia in a burned extremity are unreliable,19 the author advocates measuring the tissue pressure by a direct method and uses the Stryker® Intracompartment Pressure Monitoring System. A tissue pressure above 40 mmHg is the indication for surgical decompression of the injured limb. Alternatively, a Doppler ultrasonic flow meter can be used to assess the circulatory status of the extremity.19 A muffled first arterial sound and/or the absence of the second arterial sound is regarded as sufficient evidence of pathological elevation of the tissue pressure.
Burns across joints do not, for that reason alone, require admission to a hospital.
Injuring agent
Electricity
Patients exposed to low-voltage electricity, arbitrarily defined as less than 1000 volts (the most frequent source being household currents of 110 or 220 volts), are in danger of dying at the accident scene from a cardiac dysrhythmia, usually ventricular fibrillation.20 Following low-voltage electrical exposure, the most frequent residual electrocardiographic abnormality is a non-specific change in the ST-T wave segment21 and the most troublesome dysrhythmias are among the atrial fibrillation-flutter group.22 If the electrocardiogram is normal or becomes normal during observation, the chances of a subsequent dysrhythmia or cardiac arrest are virtually nil.
Chemicals
Although chemicals cause tissue damage by chemical reactions and not from heat, by tradition, the care of those injured by chemicals is by burn surgeons. Brushing off dry chemicals or copious lavage with water of wet chemicals is the appropriate emergency treatment.23,24 No one knows how long lavage should be continued, but up to 1 h has been recommended.25 One guide is the presence of pain. The supposition is that, as long as there is pain, the chemical remains active and continues to cause damage.
In some instances, there are specific antidotes for the pain caused by a chemical. For example, with hydrofluoric acid, the injured tissues should be injected with calcium gluconate.26 Hydrofluoric acid also serves as a good example of the many chemicals that are absorbed into the body with the potential to cause organ injury. Exposure of concentrated hydrofluoric acid to as little as 3% of the body surface area can result in a fatal dysrhythmia from hypocalcemia caused by the binding of calcium by the absorbed fluoride ion.27 Since it is impossible to remember the systemic sequelae of all the chemicals to which an individual might be exposed, the physician should identify the chemical and seek information from the local poison control center.
Treatment
Cooling the burn
The first objective in burn wound care is to dissipate the heat. As long as the temperature in the tissues is above 44°C injury continues.28 The first step is to remove the source of heat. Both clinical and experimental evidence indicate a beneficial effect from immediate active cooling of the wound to dissipate heat.29 Cool tap water or saline at about 8°C (46.4°F) applied in any practical manner (e.g. compress, lavage, or immersion) is as effective as any other product or method.30–32 Colder substances, such as ice, may be detrimental.33 The period of time that is required for active cooling is brief.34 Typically, by the time most patients present for care, the tissues have cooled spontaneously.
Active cooling also has several potential advantages beyond dissipation of heat. First, cooling stabilizes skin mast cells, decreasing histamine release and, thereby, decreasing edema of the wound. Second, in the first several hours after the injury, cooling is an effective way of controlling the pain of partial-thickness burns.35,36 In cooling for pain control, cool, but not ice-cold,37,38 moist compresses are applied to the painful wound. This method is applicable in the management of virtually all patients whose wounds can be safely cared for in an ambulatory setting. Because of the limited surface area of burn among most of those patients treated as outpatients, the detrimental systemic effects of active cooling, e.g. hypothermia from accelerated heat loss, should not occur. However, since water conducts heat 23 times faster than air, it makes good sense to monitor the patient’s core temperature during active cooling of the wound. A limit to the surface area that is cooled is arbitrary, but a practical limit is about 10% of the TBSA.
Pain control
Burn wounds are painful. The most severe pain occurs with partial-thickness wounds devoid of epidermis. Initially it is intense and can prove to be unbearable. The pain spontaneously moderates after several hours but intensifies when wounds are manipulated during dressing changes, wound care, and physical activity. While eschar-covered burns may be insensate, when the eschar separates spontaneously or is removed, the exposed viable tissues are painful when cut into, cauterized, or manipulated.39
Clearance of these classes of drugs is accelerated among those who regularly abuse alcohol or controlled substances.40,41 Therefore, remarkable amounts of analgesics and sedatives may be required.
Topically applied or injected local anesthetics are not recommended in the management of burns.
Local burn wound care
Blisters
Recommendations for the management of blisters are varied and range from leaving blisters intact,42 to removing the blistered skin immediately,43 or delaying removal.44
Those who advocate removal of blistered skin cite laboratory studies that show that the blister fluid exhibits several potentially detrimental effects.43 Immune function is depressed by impairment of polymorphonuclear leukocytes and lymphocytes. Blister fluid adversely affects neutrophil chemotaxis, opsonization, and intracellular killing. Inflammation is enhanced by the presence of metabolites of arachidonic acid in the blister fluid. A plasmin inhibitor in the blister fluid decreases vascular patency. Finally, blister fluid may provide a medium for the growth of bacteria. Based on these considerations, the case can be made that blistered skin should be removed to facilitate healing.
Conversely, this author recommends leaving burn blisters intact. Blisters form in the stratum spinosum layer of the epidermis. An intact blister usually indicates a superficial partial-thickness wound, which will heal spontaneously within 3 weeks. If, under these circumstances, the blistered skin is removed, the wound is converted from an absolutely painless one to a painful open wound exposed to colonization by bacteria and potential infection.42 An infection in a burn wound covered by an intact blister rarely, if ever, occurs. Therefore, this author prefers to leave blisters intact, and recommends that they be dressed for protection and not necessarily covered with medication.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree