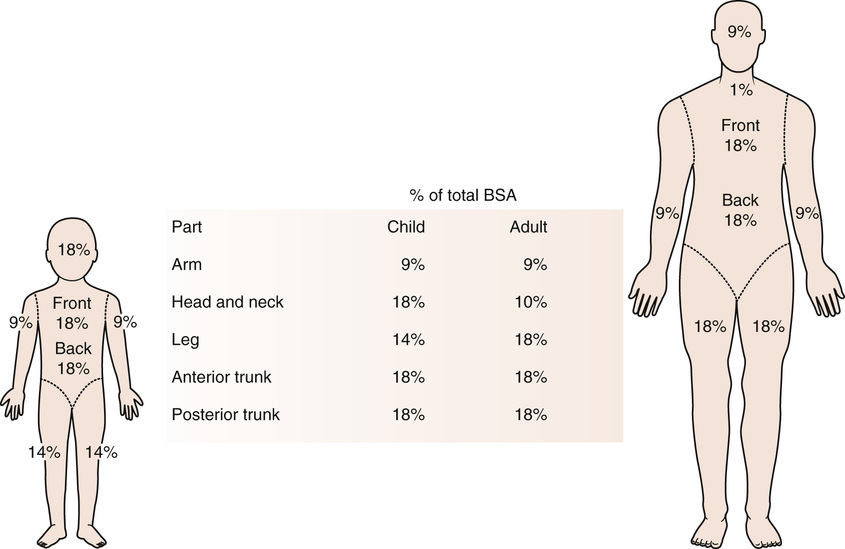
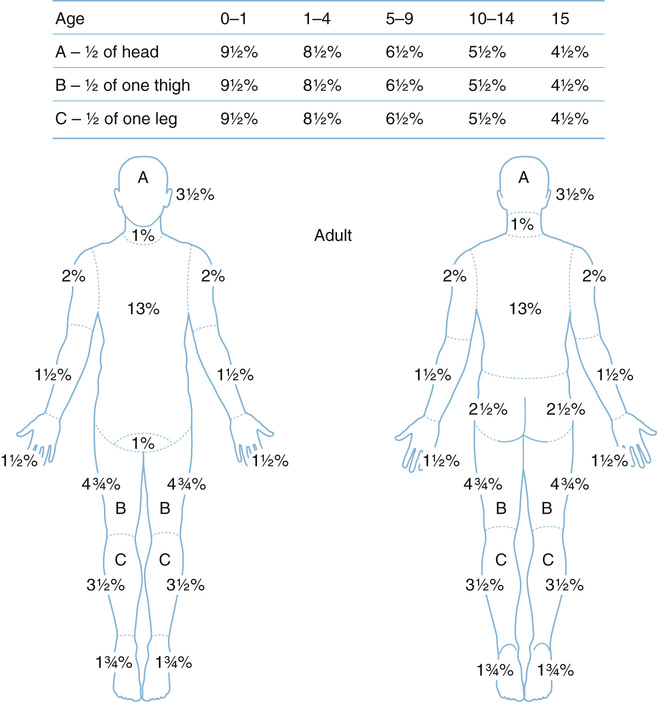
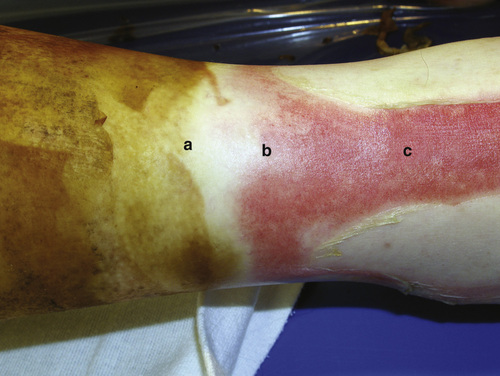
1. Burn severity or “degree”: Described based on depth of injury • Third degree (full thickness): Charred or translucent, “white” color, mild pain, pin prick absent 2. Burn volume: Described by total body surface area (TBSA) involved • “Rule of nines” (see Figure 22.1) • Lund and Browder method (see Figure 22.2) • Outcomes of burns better at high-volume centers • Criteria for referral to an accredited burn center (American Burn Association) (see Box 22.1) • Zone of coagulation: Central area of nonviable tissue • Zone of stasis: Threatened area with initial perfusion that can progress to ischemia ▪ Progression can be prevented with adequate resuscitation • Zone of hyperemia: Outer area of viable tissue (see Figure 22.3) 2. Burns >30% TBSA are associated with a systemic inflammatory response and general down-regulation of the immune system, including • Reduced B-lymphocyte function, T-helper-cell function, and cytotoxic T-lymphocyte function • High-volume resuscitation is warranted in burns >20% TBSA ▪ (4 mL/kg) × (weight in kg) × (% TBSA) = total fluid to be infused over 24-hour period. ▪ Give remaining half during the next 16 hours. • Titrate fluid resuscitation to urine output. ▪ Urine output can be falsely elevated with elevated urine glucose (glycosuria), thereby overestimating a patient’s fluid status. • Systemic prophylactic antibiotics and steroids have not been shown to improve outcomes. ▪ Antibiotics are indicated in the presence of cellulitis, purulent drainage, and active infection. ○ Most common organisms are methicillin-resistant Staphylococcus aureus, Pseudomonas, and Klebsiella. • Most common cause of death is bronchopneumonia. • Large burns are associated with hypermetabolism. • Elevated daily protein requirement for burn patients • Enteral feeding is preferred to parenteral nutrition. 4. Topical antimicrobial agents ▪ Advantages: Can provide antimicrobial coverage and some hemostasis • Silver sulfadiazine (Silvadene) ▪ Advantages: Broad-spectrum antimicrobial coverage • Mafenide acetate (Sulfamylon) 5. Surgical management/burn reconstruction • Operative excision and grafting are recommended for burn wounds that are not likely to reepithelialize and heal within 3 weeks. ▪ The practice of early burn wound excision and grafting has reduced mortality from burn wound sepsis. • Skin substitutes may be used in patients who may not have enough donor site availability for burn wound coverage. ▪ Cultured epidermal autografts: Ex vivo expansion of donor keratinocytes ○ Advantages: Can obtain ~10,000-fold expansion; available in spray form ▪ Symptoms ○ Dry, pale/whitish skin, nonblanching, insensate ○ “5 Ps”: pain, pallor, poikilothermia, paresthesia, pulselessness ▪ Perform at bedside as soon as the patient stabilized ▪ Make incisions in the following orientation and with a depth into the subcutaneous fat: ○ Arm/forearm: Longitudinal medial and lateral ○ Hand: Thenar/hypothenar, dorsal incisions 3× between metacarpals, digital midlateral lines ○ Chest wall: Midline, + /− transverse ○ Thigh/leg: Longitudinal medial and lateral ○ Foot: Dorsal, medial, lateral • Reconstruction of burn wounds can be performed through skin grafts, pedicled flaps, and/or free flaps.
Burns and Burn Reconstruction
Initial Evaluation
Burn Physiology
Burn Management
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Burns and Burn Reconstruction
Chapter 22
 cc/kg/hr
cc/kg/hr





