Chapter 8
Burns
- Introduction
- Thermal burns
- Burn reconstruction
- Chemical burns
- Electrical burns
- Cold injury
- Conditions causing burn-like wounds
- Further reading
Introduction
- A burn is defined as coagulative destruction of the surface layers of the body.
- 250,000 burn injuries occur in the United Kingdom and 2.5 million in the United States every year.
- Most are preventable.
- Every year, 300 people die in hospital following burns in the United Kingdom; 3500 in the United States.
- Mortality after a 50% total body surface area (TBSA) burn in a young adult has reduced from 50%, 25 years ago, to 10% with modern management.
- Ten years ago, an 80–90% TBSA burn had a 10% chance of survival.
- This has improved to >50% survival.
- Improvements are attributed to advancements in:
- Resuscitation
- Surgical techniques
- Management of sepsis
- Nutritional and metabolic support.
- 250,000 burn injuries occur in the United Kingdom and 2.5 million in the United States every year.
Classification
Aetiology
- Thermal
- Chemical
- Electrical
- Cold injury
- Radiation.
Depth
- Superficial (epidermal only)
- Superficial dermal
- Deep dermal
- Full thickness.
- Superficial dermal
Body surface area involved
- Burns >15% TBSA in adults or >10% in children require formal resuscitation.
Thermal burns
- Most burns are thermal injuries, caused by:
- Scalding by hot liquids or gases
- Contact
- Flame
- Flash.
- Scalding by hot liquids or gases
- Thermal burns tend to occur in:
- The young
- The old
- The unlucky.
- The young
- Survival is largely determined by the burn’s TBSA and depth, and patient’s age.
- Other factors determining survivability:
- Inhalation injury
- Medical conditions that limit cardiovascular and respiratory reserve
- Coexisting polytrauma.
- Inhalation injury
Pathophysiology of thermal burn injury
- The degree of tissue necrosis depends on the temperature and duration of application of the burning agent.
- Boiling water causes partial thickness burn in 0.1 seconds; full thickness burn in 1 second.
- Prolonged contact with water or radiator at 50 °C can cause deep burns in the obtunded.
Local effects
Jackson’s burn wound model describes three zones of injury:
- Inner zone of coagulation (coagulative necrosis)
- Cell death and coagulation of cellular proteins.
- Intermediate zone of stasis
- Damage to microcirculation causing ischaemia which, untreated, proceeds to necrosis.
- The extent of progression is influenced by effective resuscitation.
- Damage to microcirculation causing ischaemia which, untreated, proceeds to necrosis.
- Outer zone of hyperaemia
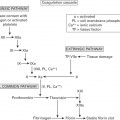
- Cellular damage triggers release of inflammatory mediators.
- Inflammatory mediators are released from:
- Capillary wall
- White blood cells
- Platelets.
- Capillary wall
- Examples: histamine, catecholamines, free oxygen radicals, platelet activating factor, arachidonic acid breakdown products.
- These result in vasodilatation and increased vessel permeability.
- Leads to fluid loss from the circulation into the interstitial space.
- These result in vasodilatation and increased vessel permeability.
- Cellular damage triggers release of inflammatory mediators.
Systemic effects
- Systemic effects occur if >25–30% TBSA is burned.
- Conceptually, this is the zone of hyperaemia, which is so extensive that it involves the whole body.
- Mediated by overspill of local inflammatory mediators into the systemic circulation.
- Examples: TNF, interleukins and interferon.
- Conceptually, this is the zone of hyperaemia, which is so extensive that it involves the whole body.
- Early excision and closure of the burn wound limits systemic inflammation.
- The systemic effects of a burn impact on all organ systems:
- Hypovolaemia
- Myocardial depression
- Pulmonary oedema
- Renal impairment
- Hepatic dysfunction
- Catabolism with increased metabolic rate
- Immunosuppression
- Loss of the protective function of the gut
- Psychological effects.
- Hypovolaemia
Burn assessment
Initial management
- Burn is trauma; should be approached in an ATLS-style.
- Airway may have sustained inhalation injury.
- Intubation required if airway patency is at risk or oedema expected.
- The tube is left uncut in case of subsequent facial swelling.
- Intubation required if airway patency is at risk or oedema expected.
- Profound hypovolaemia is not caused by acute burns—other causes of shock should be sought.
- The cutaneous burn is considered after the secondary survey is underway and immediate life-threatening injuries have been dealt with.
- Exposure allows the TBSA of burn to be estimated and guide initial fluid resuscitation.
- Two large-bore IV cannulas inserted (through burnt skin if necessary); blood sent for baseline investigations.
- Analgesia and fluid resuscitation.
- Urinary catheter to assess adequacy of fluid resuscitation.
- Nasogastric tube to decompress the stomach.
- Also used to start early feeding to provide nutrition and gut protection.
- The wound is dressed, often with cling film in the first instance:
- Decreases evaporative fluid loss
- Allows reassessment without removal of dressing
- Helps pain relief.
- Decreases evaporative fluid loss
History
- An ‘AMPLE’ history is taken if possible.
- Helps predict likelihood of inhalation injury, depth of burn, probability of other injuries.
- Aim to establish the following facts:
- Mechanism of injury (what happened, where, when, how and why)
- Loss of consciousness
- What first aid was given and for how long
- What treatment received so far
- Tetanus status.
- Regarding scalds:
- How recently had the kettle boiled?
- Was cold milk added to the tea/coffee?
- What was in the saucepan?
- Soups, oil, vegetables or rice boil at higher temperatures than water.
- Regarding electrical injuries:
- Voltage—domestic or industrial
- Associated flash
- Associated clothing fire.
- Regarding chemical injuries:
- What chemical
- Length of time exposed to the chemical
- Specific antidotes used.
Estimating burn depth
- Burns are assessed clinically by their appearance.
- Blisters are de-roofed to assess the base of the wound.
| Depth | Appearance | Blanching | Sensation | Blisters | Healing |
| Superficial | Red, like sunburn |  | Painful |  |  |
| Superficial dermal | Pink and moist |  | Painful |  |  |
| Deep dermal | Mottled white and ‘cherry red’ fixed staining |  | Dull |  |  |
| Full thickness | Leathery white/yellow |  | None |  |  |
- Some use Laser Doppler Imaging to estimate blood flow within the wound, which correlates with burn depth.
Estimating the surface area of a burn
- Erythema should not be included.
- Erythema fades within hours—accurate burn estimation is a dynamic process.
Comparison with the palm of the hand
- A patient’s palm with fingers adducted is ≈0.8% TBSA.
- Using a template of the patient’s hand is good for small, patchy burns.
- Also good for very large burns—TBSA of unburnt skin is subtracted from 100%.
The Wallace rule of nines
- Adult body surface area (BSA):
- 9% head and neck
- 9% each arm
- 18% anterior trunk
- 18% posterior trunk
- 18% each leg
- 1% perineum.
- 9% head and neck
- BSA of children up to 1 year old is distributed differently:
- 18% head and neck
- 9% each arm
- 18% anterior trunk
- 18% posterior trunk
- 13.5% each leg
- 1% perineum.
- For each additional year of age up to age 10, 1% should be subtracted from the head and neck and 0.5% added to each leg.
- 18% head and neck
Lund and Browder charts
- Most accurate graphical record of the extent of the burn.
- Automatically account for variation in body shape with age.
- Can therefore be used for both adults and children.
Surgical decompression
- Deep dermal and full thickness burns are inelastic.
- Can cause distal limb ischaemia if circumferential.
- Similarly, extensive involvement of the chest (or abdomen in a child) can impair ventilation.
- Constriction becomes worse once fluid resuscitation is begun.
- Escharotomy relieves this constriction.
- Usually done with electrocautery, because they tend to bleed.
- Fasciotomies usually required only for burns involving muscle, or high-voltage electrical injuries.
- Escharotomies begin and end in unburnt or superficially burnt skin.
- Limb escharotomies are generally made in midaxial lines.
- Avoid the ulnar nerve at the elbow and common peroneal nerve at the knee.
- Chest escharotomies are made along the mid-axillary lines to the subcostal region.
- They are joined across the upper abdomen by a chevron incision parallel to the costal margin.
- This creates a mobile breastplate that moves with ventilation.
- The anaesthetist can advise on the adequacy of chest escharotomy by a drop in ventilator airway pressures.
- They are joined across the upper abdomen by a chevron incision parallel to the costal margin.
Inhalation injury
- Patients with possible inhalation injury should be reviewed by an anaesthetist prior to transfer to a burns unit.
- Prophylactic steroids or antibiotics are not indicated.
Diagnosis
- Inhalation injury is a clinical diagnosis.
- Chest X-ray and arterial blood gas analysis may initially be normal.
- Carboxyhaemoglobin levels are useful, but may be normal if patients receive oxygen during transfer to hospital.
- Fibre-optic bronchoscopy is most reliable for making the diagnosis.
- Characteristic bronchoscopic findings:
- Soot below the vocal cords
- Hyperaemia
- Mucosal oedema and ulceration.
- Soot below the vocal cords
Factors suggestive of inhalation injury
- History of inhaled hot gases and vapours given off by a fire:
- Fire in an enclosed space
- Patients found unconscious in a fire.
- Fire in an enclosed space
- Symptoms
- Hoarse or weak voice
- Brassy cough
- Restlessness
- Shortness of breath
- Hoarse or weak voice
- Signs
- Soot around the mouth and nose
- Singed facial and nasal hair
- Deep burns to face, neck and upper body
- Carbonaceous sputum or carbon deposits in the mouth and oropharynx
- Swollen upper airway
- Stridor
- Dyspnoea
- Hypoxia
- Pulmonary oedema.
- Soot around the mouth and nose
Classification of inhalation injury
Supraglottic
- Caused by heat.
- If suspected, the airway must be secured before swelling develops in the ensuing hours.
- Oedema usually resolves spontaneously within 3–5 days.
Subglottic
- Caused by products of combustion.
- Act as direct irritants to the lungs, leading to bronchospasm, inflammation and bronchorrhoea.
- Secretions tend to pool due to the dysfunction of the mucociliary elevator, leading to atelectasis, adult respiratory distress syndrome (ARDS) and secondary pneumonia.
- Other changes:
- Ventilation-perfusion mismatching
- Decreased lung compliance
- Increased airways resistance.
- Respiratory failure is common, requiring support in the form of:
- Humidified oxygen
- Nebulisers
- Heparin to prevent cast formation
- Acetylcysteine, a mucolytic
- Salbutamol, a bronchodilator
- Heparin to prevent cast formation
- Chest physiotherapy
- Non-invasive ventilation with positive end-expiratory pressure (PEEP)
- Intubation and ventilation for bronchial lavage with dilute sodium bicarbonate.
- Secretions tend to pool due to the dysfunction of the mucociliary elevator, leading to atelectasis, adult respiratory distress syndrome (ARDS) and secondary pneumonia.
Systemic
- Results from inhalation of carbon monoxide (CO) or cyanide from the fire.
- Patients may require respiratory support.
Carbon monoxide poisoning
- CO has 250 times the affinity for deoxyhaemoglobin as oxygen.
- Half life of CO in patients breathing room air is ≈250 minutes.
- Half life of CO in patients breathing 100% oxygen is ≈40 minutes.
- Half life of CO in patients breathing room air is ≈250 minutes.
- CO binds to intracellular cytochrome proteins, affecting mitochondria.
- Levels up to 10% may be found in smokers or truck drivers.
- 15–20% cause headache and confusion.
- 20–40% cause hallucinations and ataxia.
- CO levels of 60% are fatal.
- Levels up to 10% may be found in smokers or truck drivers.
- Arterial blood gas analysis shows elevated carboxyhaemoglobin and metabolic acidosis.
- Pulse oximetry cannot differentiate between oxy- and carboxyhaemoglobin.
Treatment
- CO poisoning is treated with 100% oxygen, delivered through a non-rebreathing facemask with a reservoir.
- Patients with levels >25–30% should be ventilated.
- It important to continue oxygen until the metabolic acidosis has cleared.
- Later secondary release of CO occurs from the cytochrome system.
- Persistent metabolic acidosis may be due to poisoning by, e.g. cyanide.
Tracheostomy
- There is no consensus on tracheostomy use in burn patients.
- Often used in patients with large burns and inhalation injury.
- They typically require repeated surgeries and prolonged ventilation.
- Benefits of tracheostomy in inhalation injury:
- Ease of access to the bronchopulmonary tree for toileting and lavage.
- Improved ventilator weaning by reducing:
- Dead space (10–50% less than endotracheal tube)
- Airway resistance
- Work of breathing
- Sedation requirements.
- Dead space (10–50% less than endotracheal tube)
- Complications of tracheostomy:
- Bleeding from the wound or erosion of brachiocephalic vessels
- Accidental decannulation
- Swallowing dysfunction
- Tracheal ulceration and granulation tissue
- Tracheo-oesophageal fistula
- Tracheal stenosis.
Complications of inhalation injury
- Complications of mechanical ventilation
- Barotrauma and pneumothorax result from high ventilatory pressures required to overcome poor lung compliance and increased airways resistance seen in ARDS.
- This can be avoided by employing lung protective ventilation strategies:
- Pressure controlled ventilation
- High ventilation rate
- Small tidal volumes
- Inverse ratio ventilation
- Physiological PEEP (approximately 5 cm H2O)
- Lower target oxygen saturation of 92%
- Permissive hypercapnia and respiratory acidosis.
- Pressure controlled ventilation
- High-frequency oscillatory ventilation can be used as a rescue strategy when conventional ventilation fails.
- Barotrauma and pneumothorax result from high ventilatory pressures required to overcome poor lung compliance and increased airways resistance seen in ARDS.
- Complications of long-term intubation or tracheostomy
- Tracheomalacia
- Tracheal stenosis.
- Tracheomalacia
- Complications of persistent inflammation
- ARDS
- Multiple organ dysfunction syndrome (MODS)
- In the long-term, fibrosis can lead to emphysema and bronchiectasis.
- ARDS
Fluid resuscitation
- Greatest fluid losses occur in the first 24 hours post-burn.
- Increased vascular permeability allows leak of fluid and proteins from the intravascular to the interstitial compartment.
- The rate of leakage peaks around 8–12 hours post-burn.
- Burn shock results from this fluid shift, coupled with myocardial depression.
- The goals of fluid resuscitation are:
- Restore circulating volume
- Preserve tissue perfusion
- Avoid ischaemic extension of the burn wound.
- Achieved by administering large volumes of salt-containing fluid.
- Major burns present a ‘Catch 22’ situation:
- Burn oedema drives burn shock, but fluid resuscitation (required to treat burn shock) drives burn oedema.
- Fluid resuscitation is required for:
- Adults with burns >15% TBSA.
- Children with burns >10% TBSA.
- The optimal fluid and resuscitation algorithm is controversial.
- In most units, fluid resuscitation is administered by one of the following regimes.
- Fluid requirements are calculated from the time of burn, not time of admission.
- The goals of fluid resuscitation are:
Parkland
- 4 ml/kg/% burn of Hartmann’s solution in the first 24 hours after the burn.
- Half the fluid is given in the first 8 hours after injury.
- The second half is given in the next 16 hours.
- Half the fluid is given in the first 8 hours after injury.
- Hartmann’s solution contains:
- Na+ 131 mmol/l
Cl− 111 mmol/l
Lactate 29 mmol/l
K+ 5 mmol/l
Ca2+ 2 mmol/l.
- Na+ 131 mmol/l
Crystalloid sparing strategies
- Infusion of large volumes of crystalloid is associated with oedema, increased total body sodium and abdominal compartment syndrome.
- To mitigate these problems, some units introduce colloid as a crystalloid-sparing measure after 8 hours, when vascular permeability begins to decrease.
- Other units may wait for 24 hours.
- Use of colloids in burns resuscitation is controversial.
- Albumin has been used in adults for many years.
- Fresh frozen plasma (FFP) is often used in children.
- Randomised controlled trials of hydroxyethyl starch (HES) products in critically ill patients show increased risk of mortality and renal failure.
- Hence they have been withdrawn from the UK market.
Muir and Barclay
- Calculates the volume of human albumin solution to be given in the first 36 hours following a burn:
- 0.5 ml/kg/% burn gives a volume to be infused in each time period.
- The time periods are 3 × 4 hours, 2 × 6 hours and 1 × 12 hours.
- 0.5 ml/kg/% burn gives a volume to be infused in each time period.
- Formulas give only estimates of fluid requirements.
- They are unreliable at the extremes of age.
- More fluid may be required for:
- Paediatric burns
- Delayed resuscitation
- Large burns
- Deep burns
- Burns where an accelerant, such as petrol, was used
- Electrical burns
- Inhalation injury
- Coexisting polytrauma.
- Charles Baxter, who described the Parkland formula, reviewed its use:
- Accurate in 70% of adults.
- Overestimated in 18%; underestimated in 12%.
- Most often inadequate for burns >80% TBSA and patients >45 years.
- Few paediatric cases fell outside a range of 3.7–4.3 ml/kg/% TBSA burn.
- The rate of infusion is modified to meet specific end points of resuscitation:
- Urine output is the best indicator of tissue perfusion
- Aim for 0.5–1 ml/kg/h in adults; 1–1.5 ml/kg/h in children
- Double this after high-voltage electrical injuries.
- Aim for 0.5–1 ml/kg/h in adults; 1–1.5 ml/kg/h in children
- Other parameters to be monitored:
- Pulse, blood pressure, capillary refill
- Core–peripheral temperature gradient
- Respiratory rate
- Urine osmolality.
- Pulse, blood pressure, capillary refill
- Serial measures of arterial blood lactate and base excess also indicate adequacy of resuscitation.
- Direct measurement of cardiac output with transoesophageal Doppler can identify patients who would benefit from inotropes or vasopressors.
- Inotrope of choice: norepinephrine; preferred vasopressor: dobutamine.
- Drugs are not used to ‘treat’ low urine output without first ruling out hypovolaemia, which is treated with more fluid.
- Injudicious vasopressor use worsens tissue hypoperfusion, causing extension of the burn and poor skin graft take.
- They are unreliable at the extremes of age.
Factors specific to children
- Proportionately greater surface area than adults.
- Reduced physiological reserves.
- Because of this, children require additional maintenance fluid containing dextrose.
- Daily maintenance fluid requirement:
- 100 ml/kg for the first 10 kg body weight
- 50 ml/kg for the next 10 kg body weight
- 20 ml/kg for the remainder of the body weight
- 100 ml/kg for the first 10 kg body weight
- Maintenance fluid is given enterally whenever possible.
Complications of fluid resuscitation
- Under-resuscitation
- Hypovolaemia
- Shock
- Renal failure
- Ischaemia-reperfusion injury
- MODS.
- Hypovolaemia
- Over-resuscitation
- Generalised oedema
- Pulmonary oedema
- Cerebral oedema
- Intestinal oedema
- Compartment syndrome of limbs and abdomen.
- Generalised oedema
- Both under- and over-resuscitation may deepen the burn wound.
The hypermetabolic response
- Response to major injury is described by Cuthbertson’s ‘ebb and flow’ phases.
- The ebb is a hypodynamic period lasting ≈48 hours following injury.
- The flow phase follows, for up to a year, characterised by:
- Hyperdynamic circulation with doubling of cardiac output.
- Hyperthermia, maintaining core temperature 1–2 °C above normal.
- Hypermetabolism, with increased oxygen consumption and CO2 production.
- Hyperdynamic circulation with doubling of cardiac output.
- Circulating catecholamines and stress hormones create a diabetic-like state.
- Increased glycogenolysis releases glucose, causing hyperglycaemia.
- Most of the additional glucose is metabolised anaerobically at the burn wound, generating lactate.
- Lactate is metabolised in the liver by gluconeogenesis, using amino acids derived from protein stores to replenish glucose levels.
- This process is known as carbohydrate cycling, and yields only a fraction of the energy that would be derived from aerobic metabolism.
- Breakdown of muscle protein for this purpose causes loss of lean body mass.
- Loss of >40% lean body mass is normally fatal.
- This process is known as carbohydrate cycling, and yields only a fraction of the energy that would be derived from aerobic metabolism.
- Other complications of loss of lean body mass:
- Impaired immunity and increased infection.
- Impaired healing—dietary protein is preferentially used to restore lean body mass.
- Weakness—interferes with rehabilitation.
- Pressure sores.
- Pneumonia.
- Impaired immunity and increased infection.
Modulation of the hypermetabolic response
- Nutrition
- Environment control
- Medication and hormone manipulation
- Prevention of sepsis
- Early wound closure.
Nutrition
- Aims of nutritional support:
- Maintenance of body weight and lean body mass (muscle protein).
- Electrolyte and vitamin homeostasis.
- Maintenance of body weight and lean body mass (muscle protein).
Calculating calorie requirements
- Nutritional requirements correlate with resting energy expenditure (REE).
- REE can be measured directly at the bedside using portable calorimeters that analyse oxygen consumption and carbon dioxide production.
- Many formulas estimate energy requirements based on basal metabolic rate, with various multipliers used to account for physical activity and stress factors, such as a burn.
- The Harris–Benedict equation estimates REE.
- The Schofield equation estimates basal metabolic rate (similar to REE).
- The Harris–Benedict equation estimates REE.
- The Curreri formula is popular in adult burns:
- 25 kcal/kg + 40 kcal/% TBSA burn per day
- The Galveston formula is used for children:
- 1500 kcal/m2 BSA for maintenance + 1500 kcal/m2 BSA burn.
- Given the different surface area to volume ratios of children, this may be more appropriate than using body weight.
- 1500 kcal/m2 BSA for maintenance + 1500 kcal/m2 BSA burn.
- BSA (m2) of children is calculated by the Du Bois formula.
- Various web-based calculators are available for this purpose.
Composition of nutritional supplementation
- Standard enteral nutrition is fat-based: 44% lipid, 42% carbohydrate, 14% protein.
- Using this feed, body weight is maintained by deposition of fat rather than replacement of lean body mass (muscle).
- In burns, feeding should provide most calories as carbohydrate.
- High carbohydrate diets stimulate protein synthesis by increasing endogenous insulin.
- Burn patients may require exogenous insulin to control hyperglycaemia.
- Tight glycaemic control improves wound healing; decreases infection and mortality.
- Burn patients may require exogenous insulin to control hyperglycaemia.
- Protein requirements are defined in terms of nitrogen needs.
- Nitrogen makes up about 15% of a protein.
- Protein is provided to achieve a calorie to nitrogen ratio of 100:1.
- Enteral nutrition for burns is typically 3% lipid, 82% carbohydrate, 15% protein.
- Supplementation of vitamins C, A, E and folic acid, and trace elements copper, zinc, selenium, and iron is important in a burn >20% TBSA.
- Essential for normal cellular function and co-factors in many antioxidant enzymes.
- Glutamine and arginine are conditionally essential amino acids.
- They become essential under conditions of severe stress, such as major burns.
- Glutamine is a primary fuel for rapidly dividing cells.
- Supplementation improves wound healing rates; helps mucosal integrity.
- Arginine enhances natural killer cell function and stimulates T lymphocytes.
- Supplementation also promotes wound healing.
- Burn patients are prone to potassium, calcium, magnesium and phosphate depletion.
Route of feeding
- Healthy patients with burns <20% TBSA satisfy nutritional requirements by oral feeding and supplementary drinks.
- This may not be achievable with facial burns or painful upper limb burns.
- Larger burns, confused or malnourished patients are best treated with enteral feeding.
- Ideally, this is commenced within 4 hours of injury, via a nasogastric tube.
- Major burns >40% TBSA have higher risk of gastric stasis and require repeated periods of fasting for theatre.
- For these patients, nasojejunal feeding tubes allow continuous feeding.
- Enteral feeding provides nutrition to enterocytes that help maintain gut mucosal integrity and decrease bacterial translocation.
- Parenteral nutrition is avoided in burns because of its negative effects:
- Decreased liver function with fatty infiltration
- Reduced immune function
- Line sepsis
- Increased mortality.
Environment control
- Burn patients are prone to hypothermia due to evaporative loss of water from wounds.
- In addition, core and surface temperatures are elevated above normal by an upward shift in the set-point of the hypothalamus.
- Energy to maintain body heat is provided by the cycling of carbohydrate and lipids.
- This cycling relies on amino acids derived from muscle breakdown.
- Warming the environment to 28–33 °C provides environmental heat as energy for this insensible water loss.
- Decreases the metabolic burden and attenuates the hypermetabolic response.
Medication and hormone manipulation
Analgesics and anxiolytics
- Pain and anxiety both contribute to the hypermetabolic state.
- Opioid analgesia should be used, particularly before painful interventions:
- Dressing changes
- Physiotherapy
- Position change.
- Dressing changes
- Benzodiazepines for anxiety.
- Ketamine for more extensive dressing changes.
Catecholamine antagonists
- Propranolol is a non-selective β-blocker:
- Decreases heart rate
- Reduces cardiac work
- Decreases lipolysis
- Decreases REE with less muscle wasting
- Decreases peripheral lipolysis with less fatty infiltration of the liver
- Decreases thermogenesis.
- Decreases heart rate
- Dose is titrated to reduce heart rate by 20%.
Anabolic steroids
- They decrease protein catabolism; increase protein synthesis.
- Oxandrolone has been successfully used in burns.
- Oxandrolone’s virilising androgenic side effects are 5% those of testosterone, allowing its use in females.
Hormones
- Insulin helps maintain tight glycaemic control and inhibits muscle degradation.
- Use of recombinant human growth hormone (rhGH) is controversial.
- Associated with increased mortality in adults, but not in children.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree