I. PROBLEMS
A. Burn contractures
1. Tight, shortened scars from tissue deficit
2. Can form across joint creating limitation of movement
3. Can involve more than skin: Causes shortening and fibrosis of underlying muscle, fascia, and joints
4. More common on flexor surface because flexors are stronger and flexed position is position of comfort.
5. Assessment of contracture should include description of functional limitation, presence of joint involvement, quality of scarred skin, condition, and availability of surrounding tissue.
B. Scar deformity
1. Risk factors: Wound closure, infection, race
2. Characteristics of problematic scars: Poor pliability, hypertrophic scarring, loss, uneven surface, pigment change, fragility, chronic open wounds
C. Pigment and hair loss
1. Pigment: Hyperpigmentation and hypopigmentation are problematic
a. Can develop in donor site, recipient site, or nonsurgical site.
b. Topical treatment options: Hydroquinones and retinoids for hyperpigementation
c. Lasers useful for management of red, immature scars: Pulsed dye laser.
2. Hair loss
a. Can occur in grafted region or in region of deep burn without grafting.
b. Small areas addressed with excision and tissue rearrangement, large areas with tissue expansion.
c. Mircrografts for eyebrows and moustache region.
d. Excess hair can be treated with laser (KTP or Nd:YAG) or electrolysis.
e. Thicker grafts in general will have more hair.
D. Pain and pruritis
a. Can be addressed with fractional CO2 laser.
b. Compression garment may provide temporary relief.
II. TECHNIQUES IN ACUTE PHASE OF SCAR MATURATION TO DECREASE RECONSTRUCTIVE NEEDS
A. Use sheet grafts
B. Use aesthetic units to face and hands
C. Splints, physical therapy, and scar management as early as possible
D. Place seam of graft to follow relaxed skin tension lines
III. BURN RECONSTRUCTION OFFICE VISIT
A. Obtain complete record of acute hospitalization
B. Complete record of encountered problems, including skin quality, color, pigmentation, contracture, and hair
C. Evaluate function, range of motion, and record for all examined joints
D. Evaluate skeletal deformities caused by scar contractures across joints
E. Consider needs for occupational and physical therapy, pressure garments
______________
*Denotes common in-service examination topics
F. Make inventory of all possible donor sites
G. Patient’s desires should dictate what is operated on
IV. TIMING OF RECONSTRUCTIVE SURGERY
A. Urgent reconstructive surgeries
1. Release of vital structures such as eyelids and exposed cornea
2. Release of entrapment of neurovascular bundle entrapment
3. Severe microstomia
4. Exposed ear cartilage
B. Semielective procedures (should be done within first few months to 1 year)
1. Release of joint limited by range of motion
2. Progressive deformities
C. Elective procedures
1. Should be done after 1 year to allow scars to mature.
2. Reconstruction in passive areas
3. Aesthetics
4. Hypertrophic scars
V. SURGICAL TECHNIQUES
A. Contracture release
1. Linear incision through scar overlying point of maximum tightness, oriented perpendicular to line of contracture
2. Incise skin and then keep area on tension and carefully push with scalpel.
3. If contracture persists, may need to release underlying fascia, muscle, tendon, or joint.
B. Local tissue rearrangements (See Chapter 4 “Flaps”)
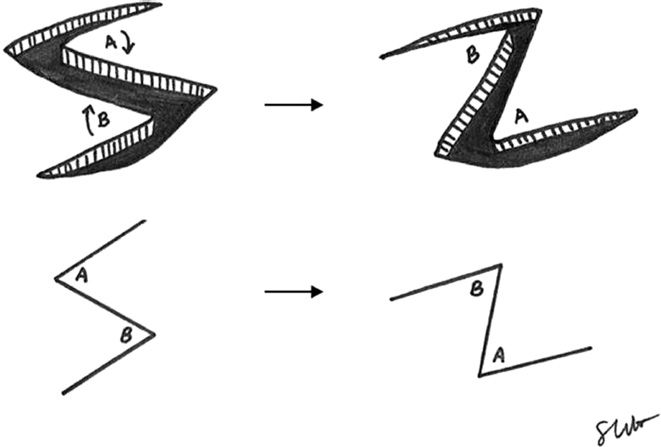
Example: The standard Z-plasty (Fig. 57-1)
1. Place central limb of Z-plasty at site of tightness
2. Have assistant hold contracture on stretch while cutting
3. After Z cut, assess if it can reach and may need to deepen Z to get additional rotation
4. Suture Z in place with 4-0 monocryl suture at the corners of the Z and then run the 4-0 monocryl along the entire Z
Figure 57-1. Z-plasty.
1. Grafts
a. In general, defects lead to loss of skin and thus skin graft is common technique used to address this.
i. Prepare graft bed by creating even surface with weck blade or versajet (helpful for small areas on the face and eyelids).
ii. Keep anatomic subunits in mind during resurfacing.
b. Meticulous hemostasis and relatively uniform wound bed aids in graft take.
c. Bolster or VAC dressing placed over xeroform can aid in graft contact if irregular surface
d. Bolsters often composed of xeroform, cotton balls +/− mineral oil ± acticoat.
e. Bolsters can be secured by using tie over silk sutures.
f. Secure graft around edges using sutures or staples
g. For reconstruction, if using split thickness skin graft (STSG), should use a thicker setting (0.012 to 0.020 in). Useful for forehead, upper eyelids, or closure of perhipheral areas.
h. Full thickness skin graft (FTSG): Consists of entire dermis therefore less remodeling and secondary contracture
i. Preferred over STSG for hand and joint surfaces
ii. Pre-expansion can increase size of FTSG
2. Dermal substitutes
a. Integra (Life Sciences): Collagen–glycosaminoglycan biodegradable matrix covered by semipermeable silicone. Secured to burn in a similar way to skin graft.
i. *Provides temporary coverage and allows for thinner STSG to be used (0.005 to 0.008 in).
ii. Increased risk of infection can be tempered with antibiotic dressing.
b. Alloderm (Life Cell): Human decellularized dermis
c. Cadaveric skin: Temporary if not enough graft available
D. Flaps
1. Distant
a. Can use rotational perforator flap such as propeller flap or keystone flap if surrounding tissue is not affected.
b. If severe hand burn, can consider groin flap or intercostal flap.
2. Free flaps
a. Thin free flap options such as fascia only with skin graft or fasciocutaneous free flaps.
b. Common flaps: Anterolateral thigh, scapular/parascapular, radial forearm (See Chapters 4 and 5).
E. Tissue expansion
1. Produces additional tissue with similar appearance to recipient site.
2. Expanded tissue has improved vascularity.
3. Especially helpful for burn alopecia.
4. Place expander through short limited incision at junction of the defect and expander site parallel to tension forces generated when expander is inflated.
5. If possible, place incision in burned skin so that it can be eventually excised.
6. Expander base dimensions should be planned preoperatively.
7. When first placing expander, it is important to make sure that the expander is not folded. The pocket must not be made too large in order to prevent unwanted changes in position of the expander.
8. Create small tract distal from expander for filling port and use remote port in a different pocket than expander.
9. Can use 10-mm, 30-degree endoscope to minimize incision and maximize dissection pocket.
F. Nonsurgical options
1. Lasers
a. Pulsed dye lasers for erythematous scars.
b. Fractional CO2 laser for hypertrophic, tight and pruruitic scars.
2. Cosmetics
A. Facial burns
1. Split face into aesthetic subunits
a. Small subunits covered with FTSG
b. Large subunits covered with thick STSG
c. Can delay with allograft to allow for thinner STSG
d. Facial allotransplantation at specific centers
2. Mouth
a. The commissure should form an acute angle at a vertical line dropped from the medial limbus in repose.
b. Contraction causes blunted oral commissure.
c. Successful splinting may counteract, or prevent, the natural tendency for a mild-to-moderate perioral burn to lead to microstomia and reduce the need for subsequent reconstructive operations.
d. Correct microstomia: Horizontally oriented release at commissure extended lateral.
i. Skin of lateral commissure incised lateral to mid-pupil
ii. Oral mucosa mobilized and advanced out laterally and closed in Y–V muocasal advancement using orbicularis oris muscle.
iii. Do not resect any tissue
e. Upper lip
i. Three subunits: Two lateral lip elements and the philtrum
ii. Philtrum can be recreated using skin graft or philtral shaped cartilage graft.
iii. The columella can be lengthened with “fork flaps” from the upper lip.
iv. Important to preserve and realign white roll where possible
f. Lower lip.
i. Can place scars in labiomental creases
ii. Maintain soft tissue of pogonion for chin prominence
iii. Untreated neck contractures can cause lower lip eversion
3. Eyebrow
a. If contralateral brow unaffected, create template from this side
b. Micrografts
c. Hair-bearing FTSG or scalp composite grafts
d. Vascularized island flap based on STA
e. Tattoo
4. Eyelid
a. Reconstructive challenges: Corneal exposure, ectropion (from internal or external contracture), and canthal contracture
b. Tarsorraphy may be helpful in the first few weeks to prevent exposure to keratitis.
c. Ectropion: Caused by inadequate tissue; therefore, in addition to release, the surgeon will need to replace tissue, often with a graft.
i. Extrinsic contracture: Need to release scar and provide additional tissue to prevent recurrence
a) Release 2 mm from the ciliary margin, extending 15 mm beyond the medial and lateral canthi
b) FTSG form contralateral side for upper lid and from retroauricular region for lower lid.
c) Dissect the orbicularis oculi muscle free from all scar tissue, re-drape the muscle over the entire eyelid as a sling, and secure it laterally to the orbital rim and medially to the nasal sidewall.
ii. Intrinsic contracture
a) Requires addressing all lamellae
b) Upper: If ipsilateral lower lid is intact: Hughes or Cutler–Beard flaps
c) Lower: Mustarde cheek advancement with deep anchoring. If no local tissue is available, pedicled temporoparietal fascia flap.
d) Subperiosteal mid-face lift through preseptal incision on maxilla
1) Release is carried laterally to the zygomatic arch, medially to the nasomaxillary buttresses, and inferiorly to the alveolus.
2) Can perform a gingivobuccal sulcus incision for complete release under direct visualization.
3) Infraorbital nerve is identified and preserved.
4) Midface is suspended from the orbital rim with permanent sutures.
5) Postseptal fat is redraped over orbital rim and septum is sewn over fat as additional layer for midface lift.
e) Medial: Release bands of scar with Z-plasties, V–M plasties, or double opposing Z-plasties
f) Lateral: Local transposition flap(s)
1) Lateral canthotomy
2) Canthoplasty
3) Laterally, the inferior limb of the lateral canthal ligament is secured to the inner aspect of lateral orbital rim with nonabsorbable horizontal mattress suture
d. The canthal tendon is secured at the level of the midpupillary line
g) Middle lamella: Palatal mucosal graft for support
1) Palatal graft measuring 8 to 10 mm in height and 20 mm in width placed superficial to the tarsal plate through the previously dissected preseptal plane
2) The superior border of the graft is placed along the inferior margin of the tarsal plate, overlapping the tarsal plate by 2 to 3 mm
3) The graft is secured in place with permanent sutures.
5. Nose
a. Layers to consider: Skin, mucosa, and cartilage
b. Consider nine aesthetic nasal subunits: Dorum, tip, columella, sidewalls, soft triangles, ala
c. Dermabrasion followed by STSG or FTSG in an aesthetic unit
d. Total or subtotal reconstruction: Forehead flap
e. Cartilage defects: Conchal or septal cartilages
6. Ear
a. Small helical rim defects: The Antia–Buch advancement flap
b. Larger helical rim defects: Davis conchal transposition flap. Elevation of a composite flap of skin and cartilage from the concha, pedicled at the crus helix, is transferred to the upper third of ear. The donor site is closed with a skin graft.
c. Extensive defects: A temporoparietal fascial flap is used to cover a cartilage framework.
d. An osseointegrated prosthesis is an excellent option for total ear loss with significant burn scar on surrounding tissue.
7. Neck and Chin
a. *Neck contractures are the most common complication of burn injury
b. Key components: Range of motion and oral competence
c. Release scar contracture down to plastysma or subplatysmal followed by coverage with large FTSG or thick STSG followed by aggressive range of motion 5 days after having patient in neck brace.
d. Can use multiple tissue expanders in infraclavicular region.
e. Postop: Compression garments for 6 to 18 months and neck brace to keep neck extended and preventing recurrence.
8. Scalp
a. Small defects: Advancement or rotation flaps with donor site closed or covered with skin graft.
b. Moderate: Tissue expansion with expander placed in subgaleal plane (deep to frontalis)
c. Extensive: Omentum or latissimus dorsi myocutnaoeus flap or large rotational flaps (Orticochea)
1. Small defect: Excision and closure
2. Moderate defect: Serial excision
3. Large defect: Tissue expansion
C. Breast
1. Key deformities: Tight skin envelope, parenchyma asymmetry, and nipple–areola complex malformations
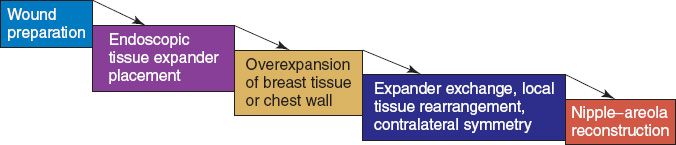
2. Tissue expansion algorithm (Fig. 57-2)
3. Autogenous reconstruction: TRAM or latissiumus dorsi if tissue uninjured
4. Can do contralateral reduction to aid in symmetry
5. Prepubescent breast burns
a. Breast bud progenitor cells are at risk.
b. Important to release contracture to allow for development of breast.
D. Axilla
1. Regions: Anterior axillary fold, mid-axillary line, and posterior axillary line
2. Common because difficult to maintain adequate positioning in acute phase of burn.
3. Shoulder should be kept 90 to 120 degrees abduction, 15 to 20 degrees flexion (60 to 80 degrees arm elevation)
4. Three grades of axillary contractures
a. Type I: Both the anterior and posterior axillary folds are involved leaving the normal skin in the hair bearing central part. A web is formed during abduction.
b. Type II: The inner portion of the upper arm and the adjacent trunk as well as one axillary fold are involved.
c. Type III: The upper arm and the lateral aspect of the trunk and completely included in one mass of U-shaped hypertrophic scar.
5. Type I and II: Contracture sequential release and thick STSGs or FTSGs
6. Type III: Local and distant flaps, including parascapular and latissimus flaps
7. Must pay attention to where hair-bearing regions are transposed
8. May need release pectoralis major or latissiumus dorsi muscles
9. Intraoperative OT range of motion including shoulder
10. Postoperative OT and splinting necessary to prevent recurrence
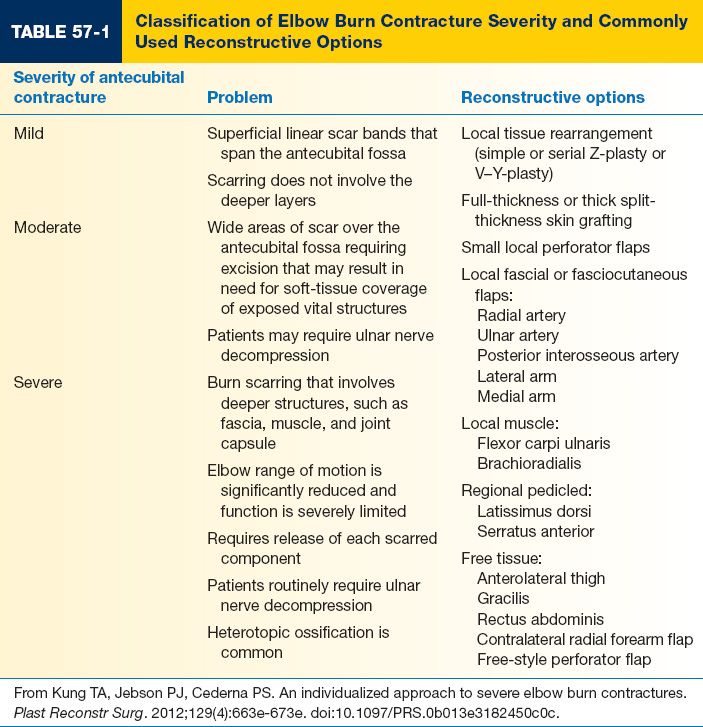
E. Elbow (Table 57-1)
1. Results from scarring along antecubital fossa or dorsal forearm and upper arm
2. No bone exposed: FTSG or thick unmeshed STSG
3. May need to perform tendon lengthening of the biceps tendon.
4. Bone exposed: Local fasciocutaneous flap—reverse radial forearm or propeller flap
5. Bone exposed and no local tissue available: Free fascia only or thin fasciocutaneous flap
6. Hetertopic ossification: Common in elbow with unknown etiology
a. Thought to be caused by trauma-induced activation of local mesenchymal cells or endothelial to mesenchymal transition of local endothelial cells
b. Current diagnosis strategies inadequate and include X-ray and CT.
c. Treatment includes radical resection of osseous tissue and contracture release.
d. More common in blast injuries and burns over 50% TBSA.
F. Hand
1. Prevention of hand contracture is key
a. Unchecked burn hand contracture: Wrist flexion, MCP joint hypertext, PIP flexion, boutonniere deformities of digit, and thumb adduction contracture
Figure 57-2. Algorithm for tissue expansion reconstruction of the burned breast.
b. Splint in position of protection: MC flexed at 70 to 90 degrees, wrist 20 to 30 degrees, IP joints in full extension and thumb kept abducted and slightly opposed
2. Flexion deformities
a. Isolated scar bands volarly or excision of scar and FTSG
b. Small defects after release: Local skin flaps such as cross finger flaps or dorsal web space flaps
c. If joint affected: Release of volar plate, joint capsule, and collateral ligaments
3. Boutonniere deformity
a. Results from destruction or weakening of central ext slip allowing lateral band to migrate volar, thus flexing PIP and extending DIP.
b. Tendon plasty using palmaris longus and groin flap for coverage after full ROM of joints.
c. Joint fusion
d. Release and redirection of lateral bands from volar to dorsal.
4. Extension deformity
a. MCP hyperextension results from dorsal skin deficits skin and graft contracture.
b. If scar released and not sufficient gain in flexion, may need dorsal capsulotomy.
a. Avoid excision of palmar skin
b. FTSG to resurface small defects, though may need dorsal neurocutaneous island flap for large defects
6. Web space contractures
a. Post-burn syndactyly is the most common secondary deformity and usually involves dorsal skin of web space
b. Treatment options: Y–V advancement, Z-plasty, “jumping man plasty” (See Chapter 4). Important to place the V–Y portion of the “jumping man” into the space you want deepended.
c. Thumb most difficult and often best treated by “jumping man”
d. If more severe: Release fascia or adductor pollicis from its insertion (and reinsert more proximally on thumb metacarpal)
e. Burn syndactyly
i. Unlike congenital syndactlyly, there is not enough laxity or surrounding tissue for reconstruction.
ii. Need to release scar and place FTSG.
7. Thumb reconstruction
a. Pollicization if index finger not involved
b. Web-space deepening
c. Toe thumb transfer
d. First web space flap and toe pulp flap to improve sensate tip
8. Nail bed
a. Dorsal digital burns cause eponychial retraction and nail bed exposure
b. A single-stage bilateral transposition flap can be used to restore the nail fold
G. Perineum
1. Perineal webs result from burn to genitalia and perineum and deep burns to proximal thigh
2. Perineal webs interfere with hygiene and ambulation
3. Early scar release and grafting important in severe deformities
4. Labia and scrotum: Release of webbing and skin grafting
5. Complete reconstruction utilizes the techniques of gender surgery: Tubed pedicle flap or a radial forearm free flap for total phalloplasty or gracilis flaps for vaginal reconstruction.
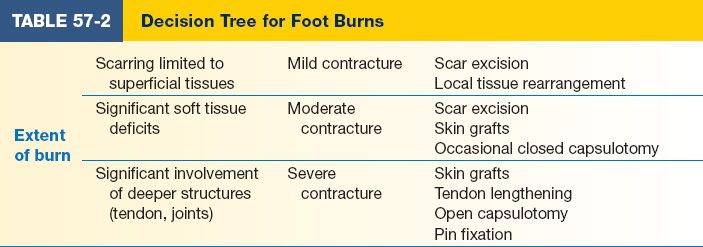
H. Foot
1. Based on the complexity, depth, and severity of the contracture, a classification system was developed to describe each toe burn scar contracture as mild, moderate, or severe (Table 57-2).
2. Mild: Superficial tissues only. Treatment: scar excision or rearranging the local tissue, that is, with a Z-plasty burn scar release.
3. Moderate: Soft tissue deficits. Treatment: scar excision and resurfacing with skin grafts. Sometimes require ancillary procedures, such as closed capsulotomy of the metatarsal phalangeal or interphalangeal joints.
4. Severe: Involvement of deeper structures, including tendons, ligaments, and joint capsules. Treatment: Multiple procedures, including skin grafting, tendon lengthening, open capsulotomy, tenotomy, and pin fixation.
A. Lack of donor sites makes this significant area of interest.
B. Epidermal replacement has already been achieved with expansion of keratinocytes
1. Takes longer to vascularize and more prone to infection
2. If graft does take, it is very thin and fragile
3. Squamous cell carcinoma have been reported from these grafts
C. Dermal replacement remains unsolved
PEARLS
1. Burned lid ectropion requires surgeon to address internal, middle and outer lamella.
2. Lower lid ectropion usually requires more than just release and FTSG for long term effects.
3. Neck scar contracture release requires post-operative splinting to prevent recurrence.
4. Burned hand syndactly often has a greater tissue deficit than congenital syndactyly and almost always requires a skin graft.
5. Burned breast reconstruction in kids requires release of the breast bud to allow breast growth.
6. Burned toe reconstruction may require release of tendons and joints depending on severity of the contracture.
7. Fractionated CO2 laser offers new method that greatly improves hypertrophic scar contour and pruritis.
QUESTIONS YOU WILL BE ASKED
1. What angle should you set up the limbs of a Z-plasty?
In general, between 60 and 70 degrees.
2. What are you gaining by doing a Z-plasty?
Gaining length at the expense of width.
3. What flap is ideal to improve a web space contracture of the thumb?
5-flap jumping man flap.
4. How do you fix burn syndactyly?
Contacture release and FTSG.
5. What tissue is best to use for FTST to the upper lid?
Contralateral upper lid.
6. What joint most commonly develops heterotopic ossification?
Elbow.
THINGS TO DRAW
1. Z-plasty and serial Z-plasty including where to place and how it rearranges tissues (Fig. 57-1 and Chapter 4—Fig. 4-3C)
2. Jumping man flap (See Chapter 4—Fig. 4-3C)
Recommended Readings
Ranganathan K, Wong VC, Krebsbach PH, Wang SC, Cederna PS and Levi B. Fat grafting for thermal injury: current state and future directions. PMID: 23370993.
Klein MB, Donelan MB, Spence RJ. Reconstructive surgery. J Burn Care Res. 2007;28(4):602–606. PMID: 17665522.
Klein MB, Moore ML, Costa B, Engrav LH. Primer on the management of face burns at the University of Washington. J Burn Care Rehabil. 2005;26(1):2–6. PMID: 15640725.
Klein MB. Burn reconstruction. Phys Med Rehabil Clin N Am. 2011;22(2):311–325, vi–vii. PMID: 21624723.
Wainwright DJ. Burn reconstruction: the problems, the techniques, and the applications. Clin Plast Surg. 2009;36(4):687–700. PMID: 19793562.
< div class='tao-gold-member'>