Breast Reduction with the Free Nipple Graft Technique
Scott L. Spear
M. Renee Jespersen
History
Breast reduction with free nipple graft is a powerful technique ideally suited to a specific patient population. Patients who require a large-volume reduction, present a high risk for adverse outcome from a pedicle reduction, and exhibit certain physiologic changes associated with gigantomastia can benefit from this technique.
Adams first presented the free nipple breast reduction for gigantomastia in 1944 (1). The drawbacks of the free nipple technique include the loss of lactation, the short-term loss and variable return of nipple sensation and contractility, common changes in pigmentation, and potential graft failure (2,3,4,5,6,7). Patients who are ideally suited for this technique therefore are often at increased risk for nipple loss after pedicle reduction, do not have highly sensate and contractile nipples, and are willing to forego breast-feeding. In fact, patients with gigantomastia frequently have poor nipple sensation and contractility, which may improve following free nipple breast reduction (5,6,7).
Pedicle reduction places the nipple at risk in gigantomastia. In general, nipple necrosis is more common in patients with severe macromastia requiring resections of 1,000 g or more, patients with longer preoperative suprasternal notch-to-nipple distance, obese patients, smokers, and otherwise unhealthy individuals (6,8,9,10,11). In gigantomastia, the folding of an excessively long pedicle can compromise circulation and lead to nipple necrosis (11). In pedicle reductions, the distance of the nipple-areola complex (NAC) transposition may be as important in increasing the risk of developing postoperative complications as the volume resected (12). This risk of nipple ischemia and necrosis can be mitigated by the free nipple technique. Blood flow to the areola measured 2 weeks after pedicle reduction is decreased below baseline, while after free nipple graft reduction it is increased (13).
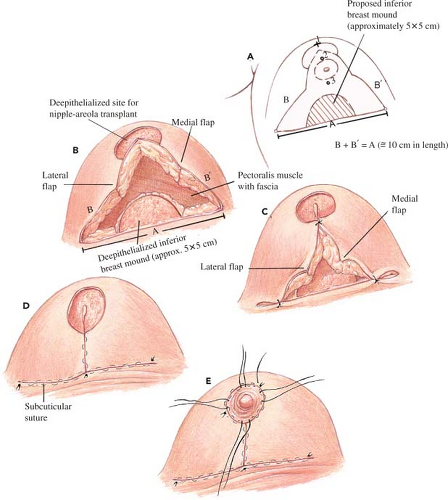
Opponents of the free nipple technique claim the inferior pedicle blood supply is reliable and that nipple-to-inframammary fold (IMF) distance is consistent, regardless of the degree of gigantomastia (14). This statement fails to account for the increased risk of nipple loss in the severely macromastic patient and is counterintuitive because as the sternal notch-to-nipple distance increases, the nipple descends and the skin stretches. It would seem that the greater the descent, the greater is the distance from the IMF. Detractors also criticize the free nipple technique for leaving a flat, boxy-appearing breast due to the loss of central volume, as will any procedure that fails to create a conical breast shape. Simply amputating the inferior breast tissue leaves medial and lateral flaps with thin fat only, as in a large, severely ptotic breast most of the breast parenchyma has descended into the inferior amputated portion (11). Because of this problem, modifications of the free nipple breast reduction technique have been designed to retain parenchymal volume and create projection. Gradinger retains breast tissue in the vicinity of the inferior pole to avoid a boxy, flat appearance in the lower portion of the breast (Fig. 100.1A). He provides breast projection by suturing medial and lateral pillars together when parenchyma is adequate, or by retaining parenchyma between the medial and lateral flaps and imbricating it when there is inadequate parenchyma (15,16). Casas et al. increase the length of the vertical limbs, deepithelialize the additional length, and fold it under the inferior pole (17). Casas et al. also close the vertical limb with a cone deformity at the nipple site to improve nipple projection and suction the lateral breast to enhance contour.
We prefer to retain the parenchymal tissue and dermis between the vertical limbs to create central volume projection (Fig. 100.2). Proponents of the free nipple graft technique argue that over the long term, the breast bottoms out less and maintains shape better than with the pedicle reduction technique because there is no pedicle that can shift or change shape with the passage of time (15,16).
Indications
The free nipple breast reduction is ideally suited for ptotic gigantomastia when more than 1,000 g is planned on being removed in postmenopausal women with no pleasurable nipple sensation (Fig. 100.3). The procedure plays a role in treating gigantomastia patients with obesity, poor health, or tobacco use, where the NAC has increased risk of necrosis. Some systemic diseases, such as diabetes mellitus, collagen vascular disease, peripheral vascular disease, and rheumatoid arthritis, might affect vascularity and increase risk of nipple loss (9). The free nipple breast reduction can be performed faster than the pedicle reduction, which may be useful in patients at higher risk of anesthetic complications. Breast reduction with free nipple graft is also applicable in special situations, such as repeat reduction mammaplasty with an unknown original pedicle (18) or prior breast biopsy in the vicinity of a proposed pedicle.
In addition to those patients who have medical problems that warrant a free nipple graft reduction, we find that there is a population of patients who may prefer the results offered by this technique. As previously mentioned, patients with gigantomastia may have little to no pleasurable nipple sensation. In this group of patients who are also past childbearing age and desire the most aggressive reduction possible, the free nipple technique offers a distinct advantage. The pedicled technique of breast reduction requires that structural elements of the breast be retained in addition to the tissue supporting the vascular pedicle. Because the free nipple technique allows the
surgeon to remove all tissue not contributing to the desired shape and size of the final breast, a greater amount of bulk can be removed than in the pedicled technique. This gives the surgeon more control over the final shape and size of the breast, as well as the ability to cone the parenchyma aggressively without distorting nipple position or compromising pedicle vascularity.
surgeon to remove all tissue not contributing to the desired shape and size of the final breast, a greater amount of bulk can be removed than in the pedicled technique. This gives the surgeon more control over the final shape and size of the breast, as well as the ability to cone the parenchyma aggressively without distorting nipple position or compromising pedicle vascularity.
Patients who are offered a free nipple graft reduction as a treatment alternative must understand, however, that return of nipple sensation and contractility is not guaranteed and that no chance of breast-feeding remains. In addition, they must understand that the grafting procedure can also fail, and that color and texture changes are still possible drawbacks even when it is successful.
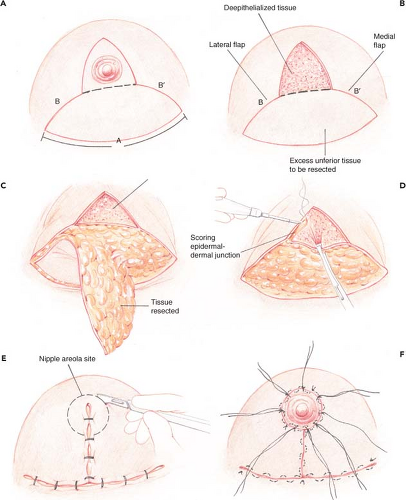 Figure 100.2. Infolding tissue between vertical limbs technique. A: The length of the horizontal limbs should equal the length of the incision along the inframammary fold. Note that B + B′ = A. B: The area between the vertical limbs is deepithelialized after the nipple-areola complex (NAC) graft is removed and saved. C: The excess tissue below the horizontal limbs is resected, leaving ample tissue between the vertical limbs. D: The epidermal–dermal junction is scored along the vertical limbs with the electrocautery unit. E: The NAC site is deepithelialized after marking with a 42-mm cookie cutter while the patient is upright, and then it is bilaterally reduced and temporarily closed with staples. F: The 4-0 silk tie is sutured through the graft and the breast skin edge to anchor the graft to the dermal platform. The vertical and horizontal skin edges are closed with a deep, interrupted 3-0 Monocryl and a running, subcuticular 3-0 Monocryl.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|