Introduction
Superior pedicle breast reduction is the authors’ technique of choice in patients who qualify for its use. Numerous advantages of this technique make it ideal for many patients. Advantages of the superior pedicle technique include a reliable vascular pedicle. The superior pedicle receives blood supply from the internal mammary vessels that branch at the second and/or third intercostal space and course to the nipple–areola complex (NAC) at a depth of 1–1.5 cm. A central mound pedicle is also maintained with perforators entering the NAC from deep by the pectoralis major muscle (thoracoacromial vessels).
The superior pedicle breast reduction technique allows resection of the ptotic, inferior portion of the parenchyma that weighs down the breast. Therefore, this technique unloads the mass at the lower pole and preserves superomedial fullness of the breasts, as desired by many women for enhanced cleavage. Unlike the inferior pedicle technique, which relies on maintaining lower pole parenchyma inferior to the NAC and elevation of the pedicle against gravity, the superior pedicle technique allows the NAC to remain suspended from the breast parenchyma above (cephalically) with removal of the heavy breast tissue inferiorly. Thus, a superior pedicle is thought to have less vulnerability to the force of gravity with less “bottoming out” over time.
This fundamental difference allows the superior pedicle breast reduction to maintain a more youthful mammary shape over long term. When performed in the manner described, the superior pedicle technique allows a more efficient use of operative time with a smaller area of de-epithelialization required compared with that in the inferior pedicle technique. There is no rotation of the pedicle required to bring the NAC into the keyhole (as is performed with a superomedial, medial, or lateral pedicle) and thus no potential risk of kinking the pedicle when in-setting the NAC. With the superior pedicle technique, the NAC is brought directly straight through the vertical incision from beneath the skin surface without twisting or turning the NAC. A large amount of breast parenchyma is kept attached to the NAC, so this technique is favorable in younger women who may want to breastfeed in the future and has minimal chance of disruption of erogenous sensation to the nipple.
Disadvantages of the superior pedicle breast reduction technique include a limited amount of breast tissue that can be resected in patients with very large, ptotic breasts. The NAC is located within the vertical portion of the inverted-T design and not undermined, which limits resection ability relative to other breast reduction techniques. Medial and lateral breast pillars are not created like in some of the other techniques; thus, breast parenchyma is not removed centrally deep to the NAC. With the superior pedicle technique, tissue is removed almost exclusively from the inferior pole with an extended resection superolaterally along the axillary tail of the breast to remove some additional undesired lateral breast volume. Because breast tissue is not removed centrally, the breast width can be narrowed only to a limited extent. Thus, the superior pedicle technique relies on advancement of medial and lateral skin flaps toward the T-junction and resection of the axillary tail, to decrease the horizontal dimension of the breast.
As with the inferior pedicle technique, the need to undermine skin to create medial and lateral flaps of uniform thickness without tension at the T-junction is a potential disadvantage of the superior pedicle technique. Considering these advantages and disadvantages, appropriate patient selection is important based on the following indications and contraindications that make some women more ideal candidates than others for a superior pedicle breast reduction approach. Guidelines regarding patient selection and technical aspects of the procedure are outlined in this chapter.
Indications and Contraindications
Patients with Regnault grade I or II ptosis or pseudoptosis and an estimated resection weight of 600 g or less are considered candidates for a superior pedicle breast reduction in the authors’ practice. Patients requiring minimal elevation of the NAC are extremely well suited for this technique. Within these standard guidelines, there are also three unique situations in which the superior pedicle reduction technique is particularly ideal.
Younger women with very glandular breasts and minimal to no ptosis who desire breast reduction can be a difficult surgical problem; there are very few reduction pedicles available that allow substantial volume reduction in women who do not need much elevation of the NAC ( Fig. 17.1 ). For instance, a superomedial, medial, or lateral pedicle cannot be designed in the standard fashion when the nipple is already at an appropriate elevated position preoperatively (i.e., minimal to no ptosis). An inferior pedicle can be performed in such a situation but is not ideal. Furthermore, these young patients are not good candidates for liposuction-only breast reduction to remove volume without changing NAC position because of the glandular rather than fatty nature of their breast tissue that prevents effective suction-assisted lipectomy.
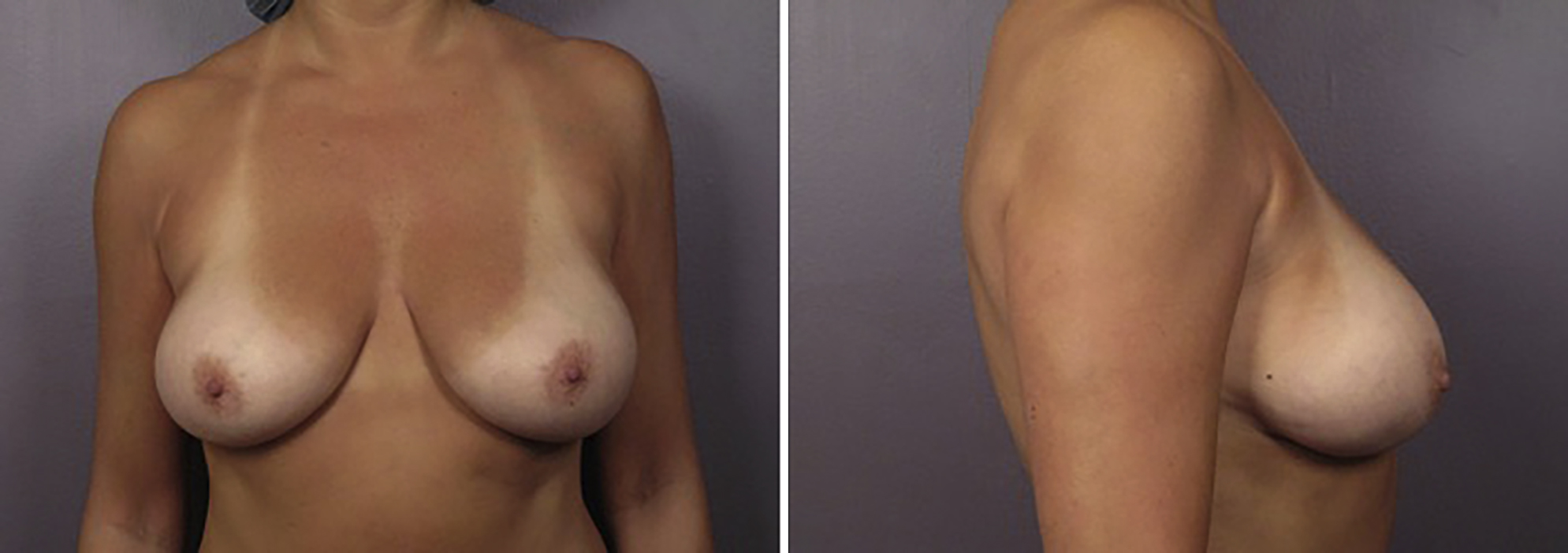
Patients who previously underwent primary breast reduction with residual/recurrent macromastia but with a NAC at an appropriately lifted level are often good candidates for a secondary breast reduction using a superior pedicle technique ( Fig. 17.2 ). The superior pedicle technique maintains central perforators from deep to the NAC; therefore, a superior pedicle can be used for a secondary breast reduction after a previous primary breast reduction with an inferior pedicle.

Limitations of use of the superior pedicle technique exist in patients needing very large reductions with long distances from the nipple to the inframammary fold (IMF). In such patients, tissue rearrangement to elevate the nipple into the desired position becomes more difficult, with increased concerns regarding vascularity of a long, narrow pedicle. Therefore, patients with Regnault grade III ptosis (NAC at the inferior-most aspect of the breast) are generally not good candidates for a superior pedicle technique. The NAC is simply positioned too low on the heavy inferior pole tissue that weighs down the breast.
Very large reductions in patients with Regnault grade II or III ptosis and a very long nipple-to-IMF distance in which the NAC is inferior to the previously described triangle can be candidates for a superomedial, medial, or lateral pedicle because tissue deep to these pedicles is typically resected to reduce volume and allow rotation of the NAC into the keyhole; however, there are also concerns for impaired perfusion of the NAC with these pedicles when their lengths are very long and narrow in patients with gigantomastia and grade III ptosis. For patients not meeting the previously described indications, an inferior pedicle technique with a wider pedicle width (e.g., 10 cm) may be a better alternative. , Very large areolas (e.g., width greater than 8 cm) are not an absolute contraindication to a superior pedicle reduction, but they require a wider triangle base to completely remove the darker pigmented areolar skin and thus greater undermining of medial and lateral flaps to allow closure at the T-junction. Similar to other breast reduction techniques, contraindications include active smoking and other conditions that could have a deleterious effect on pedicle/flap perfusion and potential nipple vascular compromise.
Preoperative Evaluations and Special Considerations
A thorough history is important when assessing these patients. Patients are asked about their symptoms associated with mammary hyperplasia. Specifically, they are asked about the presence of back/shoulder pain, rashes in the IMFs, bra strap shoulder grooving, and changes in weight. Questions regarding breast health are also assessed such as recent mammograms, previous breast surgery, and family history of breast cancer. A thorough breast examination is performed to assess for any pathologic conditions, and standard breast measurements (sternal notch–to-nipple distance, nipple-to-IMF distance, breast width, and areola width) are recorded. The patient’s body mass index (BMI) is also calculated. To help the surgeon gauge the patient’s goals, patients are asked about their bra size preoperatively and desired bra size postoperatively. The weight of the breast to be removed in grams is estimated based on these measurements and patient goals. When submitting for insurance coverage, the Schnur scale is often used to determine the weight of tissue needed to be removed to meet insurance requirements. Medications that can increase bleeding or impair would healing are held. Patients 30 years of age and older undergo a preoperative mammogram. Patients younger than 30 years of age with a strong family history of breast cancer also undergo preoperative breast imaging.
Achieving a satisfactory aesthetic outcome can be challenging in patients who present for a breast lift with substantial breast asymmetry (e.g., greater than 100-g difference between the breasts) ( Fig. 17.3 ). These patients are often well-suited for a standard vertical mastopexy in the smaller breast and a superior pedicle reduction in the larger breast because of the similarities in superior/central pedicle design in both breasts. Patients with mild breast asymmetry (e.g., less than 100-g difference between the breasts) can often have the volume difference between the breasts corrected by removing parenchyma centrally from the vertical pillars of the larger breast. However, only about 50–100 g of tissue can be removed in this fashion. Therefore, patients with more than 100-g difference between the breasts can have the larger breast reduced by a superior pedicle technique that suspends the nipple in a similar fashion as a superior/central pedicle vertical mastopexy to allow for maximal possible symmetry postoperatively.

In the standard superior pedicle technique, the NAC should be within the designed triangle of the vertical limbs of the Wise pattern (not inferior to the triangle’s borders) because all of the tissue inferior to the base of the triangle is resected and the NAC is not normally undermined with this technique. If the NAC is inferior to the base of the triangle, this technique would need to be modified to extend the pedicle inferior to the base of the triangle, preventing a standard medial-to-lateral transverse resection across the base of the triangle. Such modification would also likely require undermining of the NAC to allow it to elevate into position superiorly, which would sacrifice some of the deep central perforators to the NAC. This obstacle cannot be overcome by simply designing longer vertical limbs of the triangle because that would produce a nipple-to-IMF distance that is too long at the end of the operation. Because the vertical limbs of the triangle are typically designed to be about 8 cm long to allow for an appropriate nipple-to-IMF distance postoperatively, patients who require elevation of the nipple by 10 cm or more are generally not good candidates for a superior pedicle reduction technique.
Surgical Techniques
The procedure can be described in 17 steps, which are presented in Box 17.1 and demonstrated in the . ![]()
- 1.
Mark the patient preoperatively.
- 2.
Perform tumescent injection, excluding the central mound and superior breast.
- 3.
Prepare and drape the patient.
- 4.
Mark incision site of the NAC and the de-epithelialization area.
- 5.
Make all incisions.
- 6.
De-epithelialize the triangle surrounding the NAC.
- 7.
Dissect inferior incision to the level of the de-epithelialized tissue along the chest wall.
- 8.
Dissect the medial breast pillar.
- 9.
Dissect the lateral breast pillar.
- 10.
Pass specimen off sterile field for weighing.
- 11.
Release through dermis superior to nipple.
- 12.
Dissect caudal portion of the vertical limb until the flap reaches the inset medially and laterally.
- 13.
Achieve hemostasis.
- 14.
Consider drain placement.
- 15.
Perform temporary closure with staples.
- 16.
Apply cookie cutter to mark skin excision for final position of NAC.
- 17.
Perform wound closure in layers.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree