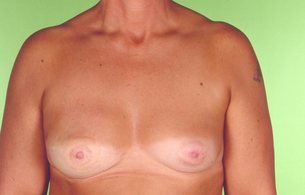
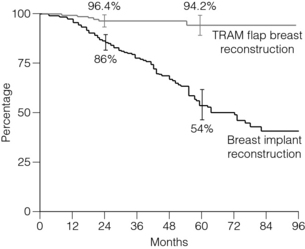
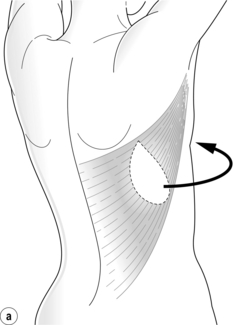
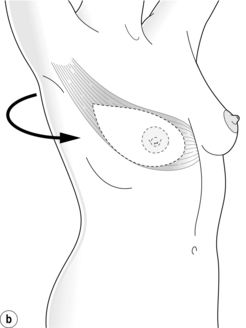
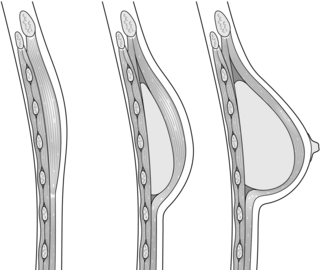
9 Surgery for breast cancer is not finished until the reconstruction has been completed in those patients who choose to have it. Mastectomy for breast cancer can lead to negative psychological effects on the patient and breast reconstruction, whether immediate or delayed, can provide significant psychosocial benefits.1–4 Even the most sophisticated breast reconstruction, however, will never fully replicate the breast that has been lost in terms of feel, movement, and erogenous sensation, although some spontaneous sensory recovery may occur.5 Women must be fully informed of all available options for breast reconstruction at the time of planning initial surgical treatment so that they can make informed decisions, even if it is their personal preference to have a delayed reconstruction or no reconstruction at all.6,7 The ultimate goal of breast reconstruction is to produce a ‘breast’ that satisfies the patient’s wishes and matches the contralateral breast, also improving the preoperative breast aesthetics if possible. Breast reconstruction may be either autologous, non-autologous, or a combination of the two, with the use of symmetrising mastopexy, reduction or augmentation surgery if necessary.8 The decision regarding the timing and technique of breast reconstruction should be made by the patient and a multidisciplinary breast cancer team, which should include reconstructive surgeons who are able to provide the full range of commonly used reconstructive procedures. The principal aim of breast cancer surgery is to provide safe and successful oncological treatment. The decision for delayed or immediate breast reconstruction and the reconstruction offered may be affected by the anticipated need for adjuvant therapy.8 The main advantage of immediate breast reconstruction is that the patient does not have to spend any time without a breast mound. It allows preservation of the native breast skin envelope and inframammary fold and therefore the reconstruction usually assumes a more natural shape when the breast volume is restored. The mastectomy skin flaps are pliable and unaffected by soft-tissue contracture and scar, and have not suffered the effects of radiotherapy. Skin-sparing and subcutaneous mastectomy techniques can lead to better cosmetic results, with a reduced need for contralateral symmetrisation surgery.8–10 The disadvantages of immediate reconstruction are the limited time for decision-making by the patient due to the need to perform the oncological surgery, increased operating time, and the difficulties of coordinating two surgical teams where different surgeons are required to perform the mastectomy and desired reconstruction. Immediate breast reconstruction does not compromise adjuvant treatment, although there is a potential in individual patients for complications to result in a delay in starting adjuvant treatment.8,11,12 The current indications for post-mastectomy radiotherapy lead many patients to receive radiotherapy as part of their breast reconstruction algorithm. The possibility of radiotherapy should be anticipated before proceeding with immediate breast reconstruction. Radiotherapy can have detrimental effects on breast reconstructions, but these can be reduced by choosing autologous reconstruction over implant-based procedures. With current radiotherapy delivery regimens good cosmetic outcomes can be expected in the majority of cases.13,14 Delayed-immediate reconstruction is also an option in these circumstances. Whether the use of acellular dermal matrix confers any protective effect for implant reconstruction requiring radiotherapy is unclear at present.15 It is now well established that immediate breast reconstruction does not adversely affect breast cancer outcome.13,16–18 Breast reconstruction may be indicated even in advanced disease to control locoregional disease and improve quality of remaining life.8,19,20 There is also evidence to suggest that survival may be improved by removal of the primary tumour.21 Delayed breast reconstruction allows the patient time for decision-making, psychological adjustment following their breast cancer diagnosis and mastectomy, and allows the full pathology to be available prior to reconstructive surgery. It avoids any potential delay of adjuvant treatment and also avoids any detrimental effects of adjuvant therapy on the reconstruction. In addition, the mastectomy skin flaps can be allowed to heal if necessary and any skin damaged by radiotherapy can be excised. The main disadvantage is that skin-sparing mastectomy techniques cannot be used due to the poor aesthetic outcomes of a contracted skin envelope, and therefore a much larger skin paddle is required. In addition, a second operation and episode of hospitalisation is required and treatment costs are increased compared with immediate reconstruction (see Box 9.1).22 Delayed-immediate breast reconstruction provides some of the benefits of both immediate and delayed breast reconstruction. A skin-sparing mastectomy and immediate reconstruction with a tissue expander is performed. Once the final pathology is available, patients who do not require adjuvant radiotherapy proceed to immediate breast reconstruction. Those who require radiotherapy have their expander fully deflated prior to radiotherapy to allow optimal delivery of the radiotherapy, following which the expander is serially re-expanded within a few weeks of completion of radiotherapy to prevent contraction of the skin envelope whilst awaiting delayed reconstruction.23 The aesthetics of autologous reconstruction do not deteriorate with time as with implant-based reconstruction, and are considered to be superior in terms of more natural appearance, feel and durability.24 Autologous tissue can also better withstand radiotherapy.25,26 Breast reconstruction by tissue expansion involves the serial expansion of chest-wall tissue to replace permanently the skin lost following mastectomy by repeated injections of saline into an inflatable silicone expander placed behind the pectoralis major muscle28 (Fig. 9.1). This may either be followed by replacement with a definitive implant once expansion is complete, or in the case of a permanent expandable breast implant that consists of a silicone outer lumen and an expandable saline inner lumen, only the filling port may need removal if it is not integrated into the device. Figure 9.1 Breast reconstruction with submuscular tissue expander. Courtesy of Eva M. Weiler-Mithoff. The outcomes of the technique are dependent on careful patient and implant selection. The technique appears simple and is generally good for restoring volume (Fig. 9.2), but it is difficult to create ptosis, and therefore good symmetry with the unaffected breast and true symmetry with implant-based reconstruction is best achieved by bilateral procedures (Fig. 9.3). Figure 9.3 Bilateral mastectomy with breast reconstruction with implants and nipple reconstructions. This technique is most suitable for patients with small non-ptotic breasts, when performing bilateral reconstruction, or for women who are happy to accept a mastopexy or augmentation procedure on the opposite breast. It is ideal for patients who want minimal scarring and are unwilling or unfit to undergo autologous tissue reconstruction.8,27 Patients are unsuitable for implant reconstruction if the chest-wall tissues are very thin, if the mastectomy skins flaps are of uncertain viability, or if the pectoralis major muscle is absent, either congenitally or following radical mastectomy. Radiotherapy significantly increases the risk of complications and diminishes the aesthetic result of implant/expander breast reconstruction.25,26 This may therefore not be the best method of reconstruction if adjuvant radiotherapy is planned or has already been given. The inframammary fold is an important landmark for implant reconstruction that can be preserved safely during mastectomy and should be restored with sutures if it has been violated. Careful choice of the expander is important, and the size should take into account the base width, height and projection of the normal, intact breast.29 Tissue expanders are placed under the pectoralis major muscle and the inferolateral portion may be covered by serratus fascia, allo- or xenograft, or the serratus anterior and external oblique muscles in a submuscular plane to reduce palpability. There is growing popularity for using acellular dermal matrix, most commonly human (AlloDerm®) or porcine (Strattice®) skin derived, as well as bovine skin and pericardium, to cover the inferolateral portion of the implant (Fig. 9.4). This potentially allows a one-stage immediate implant reconstruction or shortens the time taken for expansion. This technique expands the indications for immediate implant-based reconstruction in women with large ptotic breasts; however, these advantages need to be offset against the costs of the product. In the setting of one- versus two-stage reconstruction, though, the initial increased costs may be offset overall. Acellular dermal matrices (ADM) do allow much better inframammary fold definition. They are not without complications. There is a higher rate of seroma, infection and reconstruction failure with the use of ADMs. The key is to try and place the mastectomy incision over muscle and not over the matrix when inserted and to ensure primary wound healing by refreshing the mastectomy wound. This is achieved by excising the traumatised skin edges at the end of the operation. A good alternative in immediate reconstruction of large ptotic breasts is to perform a skin-reducing mastectomy and use the deepithelialised lower skin flap sutured to the caudal edge of the pectoralis major muscle to cover the inferolateral portion of the prosthesis as a vascularised dermal flap, although a contralateral reduction procedure is usually necessary. Figure 9.4 One-stage reconstruction after mastectomy with Strattice sling visible covering lower half of implant. Tissue expansion can be used for immediate or delayed breast reconstruction (Fig. 9.5). The expander is only partially inflated at insertion to allow closure of overlying mastectomy skin flaps without tension. The actual expansion starts 2–4 weeks postoperatively following an interval for healing and is usually performed at weekly intervals. The volume of expansion at each occasion should be guided by patient comfort. Overexpansion was a technique that was used to create a degree of ptosis to produce a more natural-looking breast, but this is unnecessary when anatomical devices are used. Once expansion is completed, the expander is left in place for 1–3 months to allow the skin envelope to maintain its stretch permanently. The expander is then removed, a capsulectomy or capsulotomy is performed, and a definitive implant is inserted based on the width and height of the pocket and the desired projection. Reconstruction of the breast mound can therefore take up to 6 months using tissue expansion. A slightly larger definitive prosthesis is often used following expansion with an anatomical device to reduce the risk of rotation, which can be problematic. Revisional procedures are often required to optimise the aesthetic appearance of the reconstructed breast, and over one-third of patients require further surgery within the first 5 years after implant-based breast reconstruction.30 In addition mastopexy, reduction or augmentation of the contralateral breast and lipofilling are often required to improve symmetry. The long-term aesthetic results of implant-based reconstruction can be expected to decline with time, independent of the implant type or volume, due to gradual ptosis of the contralateral side and failure of the implanted side to undergo normal ptosis, leading to late asymmetry.31 This procedure requires approximately 1 hour of operating time, a short period of hospitalisation and 2–4 weeks of recovery time. Early complications include haematoma, infection, mastectomy skin flap necrosis and wound dehiscence, and late complications include implant rupture/deflation, capsular contracture, implant malposition/rotation, implant rippling, extrusion and asymmetry. Even with the latest prosthetic materials and modern radiation delivery techniques, the complication rate for implant-based breast reconstruction in patients undergoing post-mastectomy radiation therapy may be as high as 40%, and the extrusion rate is 15%.32 The commonest and least predictable complication of implant reconstruction is capsular contracture, which may lead to firmness and visible distortion of the breast, as well as pain in advanced cases, and may warrant surgical revision. The risk of capsular contracture is significantly increased following radiotherapy.33 There is some evidence that textured implants may reduce the risk of capsular contracture.34 Lipofilling appears to improve capsular contracture and can help improve cosmetic outcomes. It is particularly valuable for implant rippling and achieving a greater degree of symmetry. The LD flap may be used either as a muscle or musculocutaneous flap. With its excellent blood supply to the overlying skin it affords a variety of skin paddle designs that can be hidden within the bra strap lines (Fig. 9.7). It is usually combined with an implant and reduces clinically evident capsular contracture and rippling of the prosthesis (Fig. 9.8). The extended LD flap includes the subcutaneous fat overlying the muscle deep to the superficial fascia to increase volume and reduce the chance of needing an implant (Fig. 9.9). Where volume is still deficient with this method, later lipofilling can be used to provide the necessary volume without the need for an implant. Figure 9.8 Immediate right breast reconstruction with extended LD flap, a very small implant and nipple reconstruction. Figure 9.9 Immediate right breast reconstruction by autologous latissimus dorsi flap after skin-sparing mastectomy. Courtesy of Eva M. Weiler-Mithoff. The pedicled LD flap has the lowest flap failure rate of the autologous reconstructions available and may be indicated in patients who are higher risk for autologous reconstruction. The best indication is in cases where the abdomen is unsuitable as a donor site either due to insufficient tissue volume or the presence of multiple scars, or where the deep inferior epigastric pedicle has been previously ligated. Disadvantages include a scar on the back, possible shoulder stiffness and impairment of upper limb function. The functional deficit of the upper limb has been investigated in multiple studies, and although its absence is well compensated for by the teres major muscle, it is necessary to counsel patients who have high demands of their upper limb, in particular for activities involving shoulder extension and adduction such as climbing and swimming, that this option may result in some functional deficit. Additional physiotherapy may also be required to restore full shoulder mobility.35 The tissue from the back is thicker than that of the native chest skin and the colour match may be different, and this needs to be taken into consideration. The procedure generally requires 3–4 hours operating time, with an extended LD usually taking longer than an LD and implant, a hospital stay of 5–7 days and a recovery time of 4–8 weeks. Indications: Indications for this technique include the reconstruction of large ptotic breasts, if the chest wall tissues are unsuitable for tissue expansion, or if additional skin needs to be imported following mastectomy. Additional indications include chest-wall reconstruction in locally advanced breast cancer, partial breast reconstruction after breast conservation surgery, or for salvage following loss of an abdominal tissue flap. Contraindications: The LD flap is contraindicated where it is suspected that previous surgery has damaged the flap pedicle, such as a thoracotomy or extensive and radical axillary surgery, congenital absence of the LD muscle, and significant patient comorbidity. Immediate LD breast reconstruction, even in the setting of postoperative radiotherapy, yields satisfactory results.36 Flap options: The LD flap is most commonly used as a musculocutaneous flap with either an oblique or horizontally orientated skin paddle. A muscle-only flap can be used where no additional skin is required, and where only skin is required, a muscle-sparing or thoracodorsal artery perforator flap may be used.37–40 Preoperative planning: It is necessary to confirm the presence of the LD muscle prior to surgery by asking patients to push down onto their hips and palpate the anterior axillary fold for muscle contraction. This is also particularly important following previous axillary surgery to indicate that the pedicle is likely to be intact, as the nerve lies in close proximity. Next it is important to decide how much skin needs to be replaced and to test the amount of skin that can be taken from the back whilst allowing closure of the donor site, taking into account skin-fold thickness. This is usually between 6 and 9 cm in width, with a lesser amount of skin taken in high risk patients such as smokers to reduce the risk of wound breakdown, and approximately 20 to 25 cm in length. In our experience using the extended LD flap, the total volume in a lean back can be expected to be approximately 200 cc, an average back 400–700 cc, and a variable amount more can be harvested in larger backs.
Breast reconstruction
Introduction
Timing
Immediate breast reconstruction
Delayed breast reconstruction
Delayed-immediate breast reconstruction
Techniques
Non-autologous reconstruction

Indications
Contraindications
Surgical techniques

Complications
Autologous breast reconstruction
Latissimus dorsi (LD) flap reconstruction