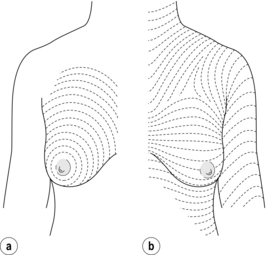
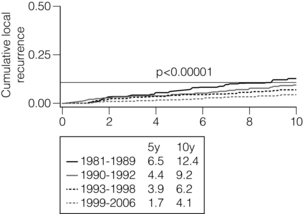
4 One of these reviews (search date 1995) analysed data from six randomised controlled trials that compared breast conservation treatment with mastectomy.4 A meta-analysis of data from five of these six trials involving 3006 women found no significant difference in the risk of death at 10 years (odds ratio 0.91, 95% confidence interval (CI) 0.78–1.05). The sixth randomised trial used different protocols. In the second systematic review, nine randomised controlled trials involving 4981 women randomised to mastectomy or breast-conserving treatment were included in the analysis.5 A meta-analysis of these nine trials found no significant difference in the risk of death over 10 years: the relative risk reduction for breast-conserving surgery compared with mastectomy was 0.02 (95% CI − 0.05 to + 0.09).5 There was also no difference in the rates of local recurrence in the six randomised controlled trials involving 3006 women where data were available: the relative risk reduction for mastectomy versus breast-conserving surgery was 0.04 (95% CI − 0.04 to + 0.12).4 Traditionally, single cancers clinically measuring 4 cm or less, without signs of local advancement, have been managed by breast-conserving treatment (Box 4.1). Different units have different size criteria and many units have a tumour size cut-off for breast-conserving surgery of 3 cm or less clinically. Clinical tumour size overestimates actual tumour size. There is a much better correlation between pathological tumour size and the size measured on imaging, with ultrasound assessment being more accurate than mammographic measurements.8 Magnetic resonance imaging (MRI) appears better than ultrasound in assessing disease extent, particularly in invasive lobular carcinoma.9 The problem with MRI is that it has a low specificity and a low positive predictive value in that only two-thirds of lesions identified by MRI as suspicious of malignancy are subsequently confirmed as malignant.10 The role of MRI in assessing patients for breast-conserving surgery has been investigated in a randomised study and the conclusions of this study were that routine use of MRI is not worthwhile.8,11 MRI did not reduce the rate of incomplete excisions and was not associated with a reduction in short-term local recurrence but did significantly increase the mastectomy rate in patients who were otherwise considered good candidates for breast-conserving surgery. It is the balance between tumour size as assessed by imaging and breast volume that determines whether a patient is suitable for breast-conserving surgery rather than tumour size per se. Options for patients with tumours considered too large, relative to the size of the breast, for breast-conserving treatment include neoadjuvant systemic therapy to shrink the tumour, an oncoplastic procedure (see Chapter 6) involving either transfer of tissue into the breast or remodelling of the breast with surgery to the opposite breast to obtain symmetry (see Chapter 6).12,13 In a patient with small breasts, excision of even a small tumour may produce an unacceptable cosmetic result. Patients with multiple tumours in the same breast have not previously been considered good candidates for breast-conserving treatment because they were reported to have a high reported incidence of in-breast recurrence14,15 and so have usually been treated by mastectomy, combined in appropriate patients with immediate reconstruction. Recent evidence has, however, demonstrated similar rates of local recurrence for both patients with unifocal and with multifocal and even multicentric disease.16,17 If it is feasible to excise the separate cancers in different parts of the breast and produce an acceptable cosmetic outcome then such patients should no longer be treated routinely by mastectomy. Satisfactory rates of local control following breast-conserving treatment for multifocal or multicentric cancers are achieved providing all disease is excised to clear margins.16,17 Early studies on multifocal and multicentric cancers often failed to achieve clear margins and this explains the high rates of local recurrence reported in these early series.15 Patients with bilateral cancers can also be treated by bilateral breast conservation. The rates of breast-conserving surgery vary significantly between countries and within countries. These rates are clearly influenced as much by the views of the surgeon treating the patient as the availability of radiotherapy locally. Failure to offer breast-conserving surgery to suitable and appropriate patients has become a medico-legal issue. If a patient who fulfils the criteria for breast-conserving surgery is treated by mastectomy then the exact reasons for the decision to proceed to mastectomy should be recorded legibly in the patient’s notes. Some patients choose mastectomy in preference to breast-conserving surgery but do so based on an inadequate understanding that outcomes for the two treatments are identical. In one series of patients choosing mastectomy rather than breast-conserving surgery, over half of patients did not know that mastectomy and breast-conserving surgery produces identical rates of survival.18 Two surgical procedures have been studied extensively: quadrantectomy and wide local excision. Quadrantectomy was based on the belief that the breast is organised into segments, with each segment draining into its own major duct, and that invasive cancer spreads down the duct system towards the nipple.19 Both of these premises are incorrect. The effectiveness of quadrantectomy relates to the large amount of tissue excised around the tumour rather than to the removal of a cancer and its draining duct. In an early randomised study of lumpectomy or quadrantectomy, a significantly greater number of patients who had lumpectomy had incomplete local excisions.20 Not surprisingly, therefore, local recurrence was more common after lumpectomy than after quadrantectomy, although survival was no different.20 Other non-randomised studies have shown similar rates of local recurrence for both quadrantectomy and wide local excision, providing margins of excision are clear.21 Quadrantectomy or segmental excisions are no longer appropriate breast-conserving options because they produce identical rates of local recurrence to wide excision but produce a significantly poorer cosmetic outcome compared with wide excision.22 The aim of wide local excision is to remove all invasive and any ductal carcinoma in situ with a margin of normal surrounding breast tissue. Controversy has surrounded which incisions give the best cosmetic results. The predominant orientation of collagen fibres in the skin was described by Langer25 and these skin crease lines around the breast are essentially circular (Fig. 4.1). Subsequent work by Kraissl26 demonstrated that the lines of maximum resting skin tension run in a more transverse orientation across the breast (Fig. 4.1). In general, scars that are parallel both to the lines of maximum resting skin tension and to the orientation of collagen fibres are quickest to heal and produce the best cosmetic outcomes, with the lowest rates of scar hypertrophy and keloid formation. Figure 4.1 The direction of Langer’s lines (a) and lines of maximum resting skin tension in the breast (b) (so-called dynamic lines of Kraissl). Having made the skin incision, the skin and subcutaneous fat are dissected off the breast tissue. Care should be taken when elevating skin not to remove subcutaneous fat unnecessarily as thin skin flaps give a poor postoperative cosmetic result. Where the cancer is close to the skin, hydrodissection infiltrating 1 in 400 000 adrenaline in saline can help to separate the skin and subcutaneous fat from the breast tissue and breast fat, and facilitates skin elevation over the cancer. Skin flaps beyond the edge of the cancer for at least 1–2 cm are mobilised. This allows the fingers of the non-dominant hand to be placed over the palpable cancer. The breast tissue is then divided beyond the fingertips. The line of incision through the breast should be approximately 1 cm beyond the limit of the palpable mass. Having incised through the breast tissue, dissection continues under the cancer. In the majority of patients it is necessary to divide the whole thickness of breast tissue down to the pectoral fascia, to ensure that there is an adequate margin of tissue removed deep to the cancer. If the lesion is superficial, and there is a significant amount of breast tissue deep to the cancer, it may not be necessary to remove full thickness of breast tissue. Likewise if the lesion is deep, more tissue can be left superficially on the skin flaps. Having reached the deep margin, which is usually the pectoral fascia, the breast tissue and cancer are lifted from this fascia. It is not necessary to excise pectoral fascia unless it is tethered to the tumour or the tumour is involving it. If a carcinoma is infiltrating one of the chest wall muscles, then a portion of the affected muscle should be excised beneath the tumour, the aim being to remove sufficient muscle to get beyond the limits of the cancer. Having dissected under the cancer, the cancer and surrounding tissue are grasped between the finger and thumb of the non-dominant hand and excision of the cancer at the other margins is completed. The specimen should be orientated immediately following excision with Liga-clips, sutures or metal markers, prior to specimen radiography and submission to the pathologist.27 Metal markers or Liga-clips are preferred because they can be seen on specimen radiography. Routine X-ray of orientated specimens is recommended because it has been shown to help the surgeon confirm the target lesion has been excised and allows assessment of completeness of excision at the radial margins.27 If the specimen radiograph shows the cancer or any associated microcalcification is close to a particular margin, then further tissue can and should be removed from the margin of concern, before being orientated and sent to pathology. A number of studies have evaluated the use of cavity shavings and bed biopsies, but few have compared these with standard assessment of margins. A minority of surgeons continue to take cavity shavings and bed biopsies routinely. Neither has been shown to be reliable indicators of local recurrence. A major concern of taking cavity shavings routinely is that significant amounts of extra breast tissue can be removed, particularly if the whole cavity is shaved; this unfortunately can adversely affect cosmetic outcome. Most importantly, however, centres who do not use these techniques report excellent local control rates, which have continued to fall over time.28,29 Wide excision with standard examination of margins thus provides sufficient information on margin status for clinical use. Bed biopsies or cavity shavings are only of value and warranted where there is concern at operation that one particular margin is involved. Having excised the cancer from the breast, suturing the defect in the breast without mobilisation of the breast tissue usually results in distortion of the breast contour. Defects in the breast are best closed by mobilising surrounding breast tissue from the overlying skin and subcutaneous tissue and in some patients mobilisation from the underlying chest wall is required. Large defects (> 10% breast volume) that are left open fill with seroma, which often absorbs later, following which scar tissue develops and contracts and can result in an ugly distorted breast. Following large-volume excisions, after mobilisation it is usually possible to close the defect in the breast tissue by a series of interrupted absorbable sutures. Given the success of lipofilling or lipomodelling for improving some patients with poor cosmetic outcomes following breast-conserving surgery and radiotherapy, a number of surgeons are exploring whether immediate lipofilling after wide local excision can improve outcomes, particularly for women with small breasts. Very large defects require oncoplastic breast reshaping (see Chapter 6) or a latissimus dorsi miniflap.12,13 Drains are not necessary after wide local excision and should not be used routinely. They do not protect against haematoma formation and increase infection rates. Breast skin wounds should be closed in layers with absorbable sutures, finishing with a subcuticular suture. As for palpable lesions, all specimens should be orientated with Liga-clips or metal markers, or secured to an orientated grid so that an orientated specimen radiography can be performed. Radiography is best performed in an X-ray machine designed specifically to X-ray specimens, such as a Bioptics® machine. There have been conflicting reports about whether compressing the specimen affects the incidence of subsequent positive margins as reported by the pathologist. Orientated specimen radiography improves the rate of complete excision of impalpable cancers.27 Cooperation between surgeon and pathologist is required so that the area of concern can be identified and assessed by the pathologist to ensure adequacy of excision. Until recently there was a reported large variation between different centres in recurrence rates following breast-conserving surgery combined with whole breast radiotherapy for invasive breast carcinoma. Over 80% of all local recurrences were reported to be located adjacent to the site of initial excision. This is no longer true and an increasing percentage of ‘recurrences’ in treated breasts are actually second primaries.25 Megavoltage radiation therapy delivered to the whole breast in a dose of 4000–5000 cGy given over 3–5 weeks continues to be used in most patients after breast-conserving surgery because radiotherapy both reduces the rate of local recurrence and improves overall survival.30 Studies continue to evaluate whether localised radiotherapy delivered either during or within a few days of surgery is as effective as whole-breast radiotherapy. As yet it has not been possible to identify groups of patients who do not require radiotherapy. However, there is likely to be a group of older patients with low-risk cancers (completely excised, node negative and hormone receptor positive on hormone treatment) and women of any age whose cancers have an extremely good prognosis (small grade 1 or special type cancers that are completely excised, node negative and hormone receptor positive on hormone treatment) whose rates of local recurrence without radiotherapy are acceptable. Following whole-breast radiotherapy, it is possible to increase the local dose of radiotherapy by boosting the tumour bed. This reduces local recurrence rates, particularly in younger women, although there are cosmetic penalties associated with the use of boost.31 The rates of in-breast tumour recurrences continue to fall over time28,29 (Fig. 4.2). Whereas a 1 % annual rate of in-breast cancer events was formerly considered acceptable, rates are now less than 0.5 % per annum. The rates of in-breast tumour events continue at a similar rate for at least 20 years. This needs to be borne in mind when considering surveillance programmes for such patients. Figure 4.2 Local recurrence rates in Edinburgh over four separate time periods showing a significant and continued fall in local recurrence rates over time. (Data unpublished, courtesy of Gill Kerr, Edinburgh Cancer Centre.) In contrast, local recurrence is much less of a problem in older patients (> 65 years). Recurrence is less frequent in women with large breasts but whether this relates to the larger excisions that can be performed in these patients or to alterations in steroid metabolism (fat is known to be an important site of conversion of androgens to oestrogens) is uncertain.36 A family history of breast cancer, particularly carriage of a mutation in one of the breast cancer genes, predisposes a patient to an increased rate of second primary cancers in both the treated and contralateral breast unless these women undergo a prophylactic oophorectomy, when local recurrence rates fall to levels similar to those of the general population.37,38 Tumour location, tumour size, the presence of skin or nipple retraction, and the presence or absence of axillary node involvement have not been shown consistently to predict for local recurrence after breast-conserving surgery.39–42 The hormone receptor status of a breast cancer does not seem to exert any influence on local control rates.31–35,39–42 In-breast tumour recurrence has been reported to be more common in human epidermal growth factor receptor (HER2)-positive cancers. Size is not significantly associated with local recurrence. Only 3 of 28 series that have examined the relationship of tumour size and occurrence have shown any significant association between tumour size in breast recurrence.43,44 A large study from Boston44 demonstrated that cancers over 4 cm in size that were treated by breast conservation surgery had a rate of recurrence similar to that of smaller cancers (Table 4.1). Table 4.1 Size of tumour related to local recurrence Data from Eberlein TG, Connolly JN, Schnitt JS et al. Predictors of local recurrence following conservative breast surgery and radiation therapy. The influence of tumour size. Arch Surg 1990; 125:771–9. A number of reports have analysed the relationship between tumour grade and local recurrence. Although some series report a higher recurrence rate in grade 3 compared with grade 2 cancers, this is by no means universal.31–35,39–42
Breast-conserving surgery
the balance between good cosmesis and local control
Introduction
Selection of patients for breast conservation
Breast-conserving surgery
Special technical details: wide local excision
Excising impalpable cancers
Factors affecting local recurrence after breast-conserving surgery
Patient-related factors
Tumour-related factors
Tumour size
Size (cm)
Local recurrence (%)
0–1
21
1.1–2
8
2.1–3
13
3.1–4
17
4.1–5
4
Tumour grade
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Breast-conserving surgery: the balance between good cosmesis and local control




