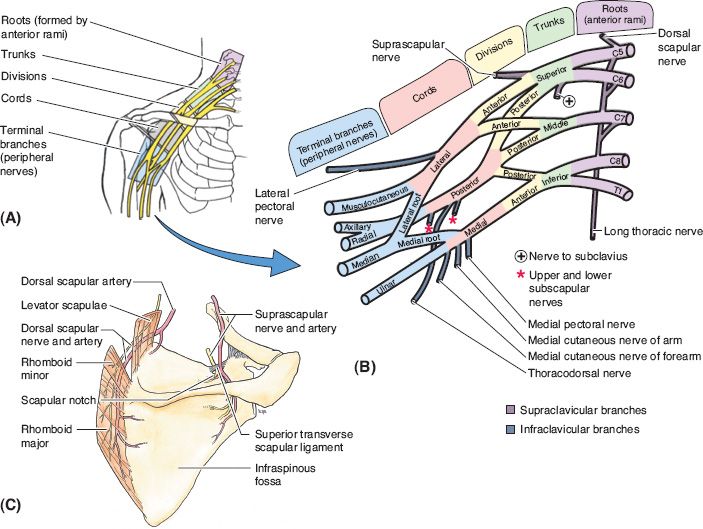
I. ANATOMY (FIG. 47-1) NERVES AND MUSCLE INNERVATION (MM.)
A. Roots (C5–T1): Formed from ventral rami
1. C5: Dorsal scapular→rhomboid minor, rhomboid major mm.
2. C5–C7: Long thoracic→serratus anterior mm.
3. C5–C8: Small root branches→scalenes, longus colli mm.
B. Trunks
1. Upper
a. Formed from C5 and C6 nerve roots
b. Nerve to subclavius→subclavius muscle (this nerve is a useful landmark)
c. Suprascapular nerve →supraspinatus, infraspinatus mm.
2. Middle
a. Formed from C7 nerve root
3. Lower
a. Formed from C8 and T1 nerve roots
C. Divisions
1. Anterior
a. From upper and middle trunk→becomes the lateral cord
b. From lower trunk→becomes the medial cord
c. Go to the flexor region of the arm.
2. Posterior: All three posterior divisions form the posterior cord and go to the extensor side of the arm.
D. Cords
1. Lateral: Lateral pectoral n.→medial aspect of pectoralis major mm.
2. Posterior (becomes radial and axillary nerves)
a. Thoracodorsal n.→latissimus dorsi mm.
b. Upper subscapular n.→subscapularis mm.
c. Lower subscapular n.→subscapularis, teres major mm.
3. Medial
a. Medial cutaneous nerve of the forearm→sensory to the skin of medial forearm
b. Medial cutaneous nerve of the arm→sensory to the skin of medial distal one-third of arm
c. Medial pectoral n.→pectoralis major and minor mm.
E. Branches
1. Musculocutaneous n. (flexors of arm)
a. Biceps mm.
b. Coracobrachialis mm.
c. Brachialis mm.
2. Radial (C5,6,7,8; posterior arm and forearm; extensors forearm and hand)
a. Triceps brachii mm.
b. Anconeus mm.
c. Brachioradialis mm.
d. Extensor carpi radialis longus mm.
e. Extensor carpi radialis brevis mm.
f. Supinator mm.
g. Extensor digitorum mm.
______________
*Denotes common in-service examination topics
Figure 47-1. Brachial plexus anatomy. A: Brachial plexus in situ. B: Brachial plexus divided into roots, trunks, divisions, cords and branches. C: Branches of brachial plexus that course over the posterior scapula. The suprascapular nerve courses under the superior transverse scapular ligament, which serves as a point of compression. This ligament may be divided to decompress the suprascapular nerve. (From Moore KL, Dalley AF, Agur AM, eds. Clinically Oriented Anatomy. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
h. Extensor digiti minimi mm.
i. Extensor carpi ulnaris mm.
j. Abductor pollicis longus mm.
k. Extensor pollicis brevis mm.
l. Extensor pollicis longus mm.
m. Extensor indicis mm.
3. Median (C6,7,8,T1; anterior forearm, thenar eminence, and first and second lumbricals)
a. Pronator teres mm.
b. Flexor carpi radialis mm.
c. Palmaris longus mm.
d. Flexor digitorum superficialis mm.
e. Anterior interosseous nerve (motor only)
i. Flexor digitorum profundus (I and II) mm.
ii. Flexor pollicis longus mm.
iii. Pronator quadratus mm.
f. Innervation to the hand—LOAF muscles
i. First and second lumbricals
ii. Opponens pollicis mm.
iii. Abductor pollicis brevis mm.
iv. Superficial head of flexor pollicis brevis (also innervated by the ulnar nerve)
a. Deltoid mm.
b. Teres minor mm.
5. Ulnar (C8,T1)
a. Forearm
i. Flexor carpi ulnaris mm.
ii. Flexor digitorum profundus (III,IV)
b. *Hand (intrinsic hand muscles except LOAF muscles)
i. Opponens digiti minimi mm.
ii. Abductor digiti minimi mm.
iii. Flexor digiti minimi brevis mm.
iv. Adductor pollicis mm.
v. Third and fourth lumbrical mm.
vi. Dorsal interossei→finger abduction
vii. Palmar interossei→finger adduction
viii. Palmaris brevis mm.
ix. Deep head of flexor pollicis brevis (also innervated by the median nerve)
F. Vascular associations
1. Supraclavicular region: Subclavian artery is in close proximity to lower roots/lower trunk
2. Infraclavicular region: Cords surround the axillary artery (cords are named with respect to the axillary artery)
3. Arm: Median nerve travels with brachial artery
G. Miscellaneous
1. Shoulder abduction→first 0 to 30 degrees: Predominantly served by supraspinatus; next 30 to 160 degrees: Mainly deltoid
2. Differentiating between C8 versus ulnar nerve injury
a. C8 root injury→Loss of all intrinsic hand muscles (both ulnar and median)
b. Ulnar nerve injury→sensory loss over ulnar aspect of the fourth and all of the fifth fingers
3. Winged scapula
a. *Serratus anterior weakness (long thoracic nerve): Most common cause of scapular winging
b. Rhomboid weakness (dorsal scapular nerve) can also cause scapular winging
c. Trapezius weakness (spinal accessory nerve) can mimic winging
d. Rotator cuff instability can also mimic winging
4. Horner’s sign is usually associated with T1 avulsion (eyelid ptosis, pupillary constriction, and anhydrosis of the skin of the affected side of the face)
5. Proximal injury (potential avulsion)
a. Injury to phrenic nerve→raised hemidiaphragm
b. Injury to levator scapulae→dorsal scapular nerve
c. Injury to serratus anterior→long thoracic nerve
H. Brachial plexus mnemonic

II. DIAGNOSIS
A. History/examination
1. Perform a detailed history asking about the time course of symptoms and pain (location, quality, radiation, exacerbation/relieving factors, autonomic changes [Horner’s→ptosis, miosis, anhidrosis], and occupational and recreational risk factors)
2. Exam should include detailed motor and sensory exam, examining the unaffected limb, range of motion (ROM), evaluation for atrophy, reflexes, and pulses
3. For proximal upper extremity nerve palsies, evaluate shoulder girdle and parascapular muscles
1. Ultrasound: Noninvasive
2. CT: CT myelogram helpful for identifying avulsion→pseudomeningocele
3. Magnetic resonance imaging
a. Magnetic resonance (MR) neurography→T2 sequence identifies edema
b. Can identify masses
C. Electromyography/nerve conduction studies (EMG/NCSs)
1. *EMG/NCSs are usually obtained at least 3 to 4 weeks after injury; nerve may still respond to electrical stimulus prior to this time
2. Neurapraxic lesion: Will see changes immediately (if you can stimulate above and below the site of injury)
3. Axonotmesis/neurotmesis: Look the same as neurapraxia on EMG/NCS
4. *Normal sensory nerve action potentials and absence of motor nerve conduction suggest root avulsion (injury proximal to dorsal root ganglion→requires nerve transfer; nerve grafting alone will not repair lesion)
D. Compound nerve action potentials (CNAPs)
1. Absence of CNAPs 2 to 6 months post injury→likely complete transection
2. Used intraoperatively to determine nerve integrity
III. PATHOLOGY/MANAGEMENT
A. Peripheral nerve regeneration→axons grow at a maximum of 1 mm/day (for injury classification see Chapter 39—nerve injuries, compression syndromes, and tendon transfers)
B. Trauma: Minimizing delay to reconstruction improves outcomes
1. Rule of 3’s: Repair within 3 days for sharp transection, 3 weeks for dirty/blunt injury, and 3 months for closed injury (except for avulsion injuries—may reconstruct sooner)
2. Upper trunk→more prone to postganglionic injury (nerve root rupture)
3. C8–T1→more prone to preganglionic injury (nerve root avulsion—may see pseudomeningocele on CT myelogram)
4. Blunt transection→ wait at least a few weeks for a neuroma to develop, can see areas that need to be resected
a. Penetrating missile/gunshot wounds
i. Result in contusion and stretch; nerve usually remains in continuity
ii. Injury caused indirectly from cavitation
5. Sharp transection (glass, knife)→acute repair within 72 hours
a. Join nerve end to end
b. Performed acutely to minimize scar and retraction of nerve
c. Nerves can potentially be electrically stimulated in the operating room before 48 to 72 hours to help define anatomy
6. Lesion in continuity (stretch, contusion, compression, injection, electrical or iatrogenic causes)—70% of cases
a. Observe for several months. Pronator teres (PT) during this time to preserve ROM
b. Can be associated with fractures or vascular injury
c. If no clinical or EMG/NCS improvement by 3 to 6 months→exploration and repair
d. Spontaneous recovery leads to better function than surgical repair in some cases
7. Fractures
a. First rib→lower trunk injury
b. Mid-humerus→radial n. injury
8. Vascular injury→if associated with vascular injury, requires immediate exploration
9. Spontaneous recovery may occur with neurapraxia and axonotmesis; not with neurotmesis
C. Tumor
1. Neurofibroma
a. Fusiform: Usually solitary, F>M, R>L side
b. Plexiform: More common in NF-1; margins less well defined
2. Schwannoma: Well-defined margins; amenable to total resection
3. Indications for resection
a. Progressive neurologic deficit
b. Significant growth
c. Intractable pain refractory to conservative management
d. Suspicion of malignant transformation
4. Malignant peripheral nerve sheath tumor: Surgical resection followed by radiation and chemotherapy
D. Inflammation
1. Parsonage–Turner syndrome (acute brachial plexitis)
a. Inflammation of BP with unknown etiology (4:1 M:F)
b. Sudden onset of pain in shoulder and upper arm followed by weakness (deltoid, biceps, supraspinatus, and infraspinatus) and numbness
c. MR neurography will show BP bright and swollen
d. Treatment: Time. Steroids are not effective. About 90% recover by 3 years. Controversial: Nerve decompression may improve outcomes
E. Entrapment
1. Thoracic outlet syndrome
a. Vascular and neurogenic causes affecting C8,T1
b. Vascular: Compression of brachial a/v→pain, pallor, coolness with arm use, overhead fatigue
c. Neurogenic: Compression of brachial plexus from cervical rib (10%), enlarged C7 transverse process, or fibrous band (most common) from C7 transverse process to clavicle or fibrotic scalene muscles
d. Mild aching pain of ulnar forearm/hand (66%). Young female with long neck = common demographic pattern. No neck pain. Bilateral in 50%.
e. Physical exam: Weakness in all hand muscles and ulnar numbness. Atrophy of the lateral thenar eminence. Thenar, hypothenar, and interossei atrophy are known as Gilliatt–Sumner hand.
i. 90-degree abduction + external rotation may provoke symptoms
ii. ± Tinel’s sign over supraclavicular fossa.
iii. Adson test: Extend neck and rotate to affected side while gently pulling down on the arms→+ if loss of radial pulse (with vascular causes)
iv. Wright test: Hyperabduct arm at shoulder and externally rotate hand→ + if loss of radial pulse
v. Roos maneuver: Hyperabduct arm at shoulder and externally rotate the hand and shoulder. Then have the patient squeeze the hand for 3 minutes. If pain and sensory symptoms are reproduced, then the test is positive.
f. Indications for surgery: Medical therapy/PT is not indicated for true thoracic outlet syndrome
g. Thoracic outlet: Contains subclavian artery and nerve. Not subclavian vein. Use a supraclavicular approach.
2. Pancoast tumor
a. C8,T1 deficit + Horner’s
b. Make sure to evaluate lung apices
F. Neonatal brachial plexus palsy (NBPP)
1. Incidence: 0.5% to 1%
2. Majority (70%) will spontaneously improve; most are upper plexus lesions
3. Must differentiate preganglionic (avulsion injuries) from postganglionic lesions (rupture). Preganglionic lesions do not recover motor function spontaneously.
4. Avulsion, rupture, and neurotmesis do not recover without surgery
5. EMG/NCS are usually not necessary and are often overly optimistic in their findings because NBPP lesions are usually partial, sparing some fibers. CT myelography helps determine whether a root avulsion is present by visualizing pseudomeningoceles and rootlets.
6. Indications for surgical intervention
a. Flail arm and Horner’s sign: Surgery before age 3 months
b. *Lack of biceps function by 3 months of age (Gilbert criterion; a classical indication) or lack of motor recovery in several muscle groups.
c. The Hospital for Sick Children Active Movement Scale and the Toronto Test Score provide a more powerful means of determining which patients would benefit from neuroma excision and grafting.
7. C5–C6 root injuries are most common and have a better prognosis than total plexus injuries. Isolated lower trunk injuries (Klumpke’s type) are extremely rare.
G. Injury types
1. *Erb’s palsy
a. Injury involving C5–C6 (upper trunk) and C7
b. “Waiter’s tip”: Shoulder internally rotated, elbow extended, forearm pronated, and palm up
c. Deltoid and supraspinatus impaired
2. *Klumpke’s palsy
a. Injury involving C8,T1 (lower trunk)
b. Claw hand, wasting, metacarpophalangeal joints extended, interphalangeal joints flexed
c. ± Horner’s syndrome
3. Pan brachial plexopathy
H. Others
1. Postradiation: Fibrosis and edema of BP causing sensory loss and pain (usually no motor deficits). EMG shows myokymic discharges.
2. Diabetic: Usually sensory polyneuropathy, but can mimic brachial plexopathy
3. Viral (2/2 to Zoster, influenza, polio): Usually sensory symptoms only
4. Inherited: Hereditary neuropathy with pressure palsies
5. Vasculitis
IV. ANATOMIC VARIATION
A. *Martin–Gruber “anastomosis”. From motor portion of median nerve to ulnar nerve in the forearm (~25% of the time)
B. *Riche–Cannieu “anastomosis”. Motor connections between median and ulnar nerves in the palm (~70% of the time); where median nerve will innervate flexor pollicis brevis
C. Prefixed plexus: Contribution from C4 (in addition to C5–T1)
D. Postfixed plexus: Contribution from T2 (in addition to C5–T1)
V. SURGICAL ANATOMY/PROCEDURES
A. Supraclavicular
1. The brachial plexus enters the posterior triangle (bordered by sternocleidomastoid muscle (SCM), trapezius, clavicle, and occiput) of the neck
2. Lies between the anterior and middle scalene muscles
3. Upper and middle trunks are in the omotrapezial triangle; lower trunks lie within the omoclavicular triangle
4. Phrenic nerve travels along the anterior scalene in a lateral to medial course
5. Exposure→through posterior triangle of neck
6. Spinal accessory nerve: Two-thirds of the way from the sternum to the mastoid along the lateral border of the SCM. May be injured during surgery involving the posterior cervical triangle (as occurs with lymph node bx).
B. Infraclavicular: Exposure→through the deltopectoral groove
C. Neurolysis
1. Removal of scar tissue from around the nerve or between the fascicles
2. Start with uninjured portion of nerve and move toward injured segment
3. If +CNAPs across the area of injury: Neurolysis alone is adequate
D. End-to-end repair
1. Possible if short nerve gap is present (after resection of surrounding neuroma)
2. Preferred over grafting, as it produces better functional results
3. Make sure to avoid tension across the repair; may need to mobilize the nerve proximally or distally
4. Approximate ends with 6-0 to 8-0 Prolene and/or fibrin glue
1. Performed when gap is to too large to perform direct end-to-end repair
2. Length of graft = length of gap + 10% of distance
3. Donor grafts→sural, superficial radial, and medial antebrachial cutaneous nerves (see Chapter 6: Microsurgery, Endoscopic Surgery and Robotic Surgery)
4. Smaller caliber graft better than larger caliber graft
F. Nerve transfer
1. Avulsion injuries are not amenable to nerve grafting and therefore benefit greatly from nerve transfer
2. Upper trunk avulsion injuries: Descending cervical plexus or spinal accessory nerve→suprascapular nerve (restores shoulder abduction)
3. Elbow flexion/shoulder abduction: Medial pectoral/thoracodorsal nerve→musculocutaneous/axillary nerve
4. Elbow flexion: Medial pectoral/intercostal→musculocutaneous n.
G. Postoperative care
1. Recovery may take years
2. Must preserve ROM with PT; nerve transfers require motor retraining
H. Others
1. Tendon transfers or free microvascular muscle transfers: For failed brachial plexus reconstructions, global avulsions
2. Wrist fusion
3. Upper extremity amputation: For painful flail arm
4. Free muscle transfer
PEARLS
1. Preganglionic (avulsion) injury is more common at C8–T1
2. Laceration injuries should be explored within 3 days and the ends coapted
3. Blunt/dirty injuries should be repaired in 3 weeks
4. Lesions in continuity should be observed for 3 months to evaluate for functional improvement
5. C5–C6 neonatal brachial plexus injuries have a better outcome than other BP injuries in this group
QUESTIONS YOU WILL BE ASKED
1. What is best timing for traction injuries of the plexus?
If no recovery is seen after 3 months, intervention and reconstruction are indicated.
2. Which nerve roots supply the brachial plexus?
C5–C8, T1.
3. Which part of the cord is most affected by obstetrical brachial plexus injury?
Upper plexus.
4. What is the clinical presentation of an upper cord injury?
Adducted shoulder, medially roated arm, extended elbow and palm up.
Recommended Readings
Borschel GH, Clarke HM. Obstetrical brachial plexus palsy. Plast Reconstr Surg. 2009;124 (1 Suppl):144e–155e. PMID: 19568147.
Colbert SH, Mackinnon SE. Nerve transfers for brachial plexus reconstruction. Hand Clin. 2008;24(4):341–361, v. PMID: 18928885.
Giuffre JL, Kakar S, Bishop AT, Spinner RJ, Shin AY. Current concepts of the treatment of adult brachial plexus injuries. J Hand Surg Am. 2010;35(4):678–688; quiz 688. PMID: 20353866.
Kim DH, Cho YJ, Tiel RL, Kline DG. Outcomes of surgery in 1019 brachial plexus lesions treated at Louisiana State University Health Sciences Center. J Neurosurg. 2003;98(5):1005–1016. PMID: 12744360.
Malessy MJ, Pondaag W. Nerve surgery for neonatal brachial plexus palsy. J Pediatr Rehabil Med. 2011;4(2):141–148. PMID: 21955972.
Piatt JH Jr. Birth injuries of the brachial plexus. Clin Perinatol. 2005;32(1):39–59, v–vi. PMID: 15777820.
< div class='tao-gold-member'>