Blepharoplasty
Mark A. Codner
Renee M. Burke
INTRODUCTION
The eyes are the focal point of the face and require detailed analysis before attempts at rejuvenation. The goal of blepharoplasty is to restore a more youthful appearance to the upper and lower eyelids while preserving their natural shape and appearance. Aging results in changes in the skin, muscle, fat, bone, and ligamentous attachments. One surgical technique is not suitable for all patients. For example, volume changes of the soft tissue can be addressed with soft tissue fillers or soft tissue transfer. Bone resorption can be addressed with bone fillers or implants to build up the underlying skeletal support. Distinct differences in surgical technique are applied to patients of differing gender and ethnicity. There are fundamental differences between blepharoplasty methods for men and women and for patients who are of Asian, African, or Occidental origin. Furthermore, patients who have signs of periorbital aging such as the tear trough deformity or malar bags require a unique surgical approach; traditional blepharoplasty techniques alone may exacerbate these findings.
Despite being one of the most commonly performed surgical procedures, blepharoplasty is a more complex and challenging procedure than has been traditionally appreciated. Complications are not only common but are noticeable, extremely bothersome to patients, and can be functionally devastating. One must be familiar with the nonsurgical as well as the surgical management of complications, including treatment of corneal irritation, ectropion, lid malposition, chemosis, and hemorrhage.
While blepharoplasty is aimed at the eyelids, the entire periorbital region requires evaluation and treatment. In upper blepharoplasty, goals include preservation, stabilization, and/or elevation of the brow and maintaining natural upper orbital fullness. Brow ptosis and eyelid ptosis are ideally corrected at the time of blepharoplasty.
During lower blepharoplasty, it is ideal to create a smoother transition between the junction of the lower lid and the cheek. Malar bags and descent of the malar fat pad may require treatment. Analysis of globe position relative to the inferior orbital rim and Hertel exophthalmometry to define the relationship of the globe to the lateral orbital skeleton are performed. To maintain the natural shape of the eyelids, treatment of tarsoligamentous laxity may be required with lateral canthal support via lateral canthopexy or canthoplasty.
SURFACE ORBITAL ANATOMY AND AGE-RELATED CHANGES
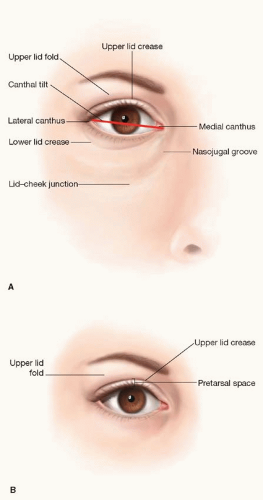
The distance from the medial to lateral palpebral fissure is 28 to 30 mm transversely and 8 to 10 mm vertically. While there is great individual variability, the lateral commissure is ideally positioned approximately 2 mm superior to the medial canthal angle, defining an upward lateral canthal tilt (Figure 46.1). The position of the lateral canthus, however, varies with age, family traits, race, and sex. In primary gaze, the upper eyelid margin forms a smooth arch with the highest point positioned superior to the pupil. With age, there is a gradual lateral shift of this apex as the tarsal plate migrates laterally due to weakening of the medial levator horn.
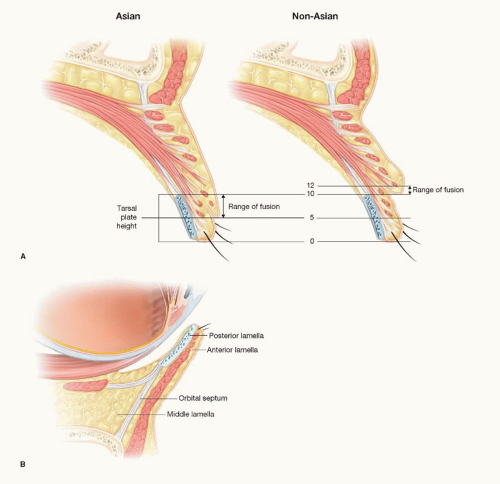
The upper eyelid crease is formed by the insertion of the levator aponeurosis into the dermis after it has penetrated the orbicularis oculi muscle. The lid fold is formed by excess skin and muscle that overhangs the crease. In the Occidental eyelid, the crease is approximately 7 mm above the lash margin at the midpupillary line in males and 8 to 10 mm in females. In the Asian upper eyelid, if a crease is present at all, it is approximately 4 to 6 mm above the lash margin. An absent crease results from the lack of levator insertion into the skin, causing preseptal fat to descend into the pretarsal space.
With aging, numerous changes are observed in the orbital region and at the multiple levels. Loss of skin elasticity presents as periorbital rhytids and the eyelids become puffy due to orbital fat bulging through the weakened orbital septum. Furthermore, periorbital hollowing develops from atrophy of periorbital soft tissue. The combination of soft tissue loss and descent around the fixed points of the retaining ligaments creates an aged surface contour defined by a series of convexities and concavities. The eyelid bags accentuate the appearance of the deepening lid-cheek junction and vice versa. Brow ptosis is recognized by lateral upper eyelid hooding as well as a narrowed brow-eyelash distance. Brow ptosis accentuates the amount of loose skin in the upper lid. Vertical creases between the brows are commonly seen and are the result of corrugator and procerus activity.
EYELID ANATOMY
The eyelid is traditionally described as a bilamellar structure comprising an anterior lamella and a posterior lamella. The anterior lamella consists of skin and orbicularis oculi muscle; the posterior lamella includes the tarsoligamentous sling, which is comprised of the tarsal plate, medial and lateral canthal tendons, capsulopalpebral fascia, lid retractors, and conjunctiva. The septum originates at the arcus marginalis along the orbital rim separating the two lamellae and is therefore often referred to as the “middle lamella” (Figure 46.2).
The Anterior Lamella
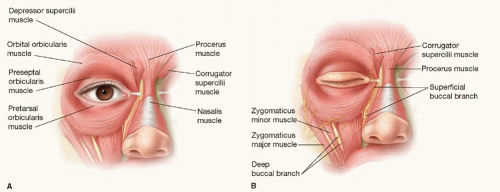
The orbicularis oculi muscle lies posterior to the thin eyelid skin, originating from the medial canthus and the bone of medial orbit and inserting at the lateral canthus and lateral orbital rim. The orbicularis oculi muscle is divided into
three components: the pretarsal, preseptal, and orbital divisions (Figure 46.3). The pretarsal portion of the orbicularis is superficial to the tarsal plate and functions to close the lid during involuntary blinking. The preseptal orbicularis assists in voluntary blinking and functions as part of the lacrimal pump mechanism for tear drainage. The pretarsal and preseptal orbicularis each have a deep and superficial component. The orbital orbicularis is the largest division of the orbicularis muscle, extruding well beyond the lids, and functions to protect the globe with forced eyelid closure.
three components: the pretarsal, preseptal, and orbital divisions (Figure 46.3). The pretarsal portion of the orbicularis is superficial to the tarsal plate and functions to close the lid during involuntary blinking. The preseptal orbicularis assists in voluntary blinking and functions as part of the lacrimal pump mechanism for tear drainage. The pretarsal and preseptal orbicularis each have a deep and superficial component. The orbital orbicularis is the largest division of the orbicularis muscle, extruding well beyond the lids, and functions to protect the globe with forced eyelid closure.
Orbicularis Muscle Innervation.
The motor innervation to the orbicularis oculi muscle is multiple in nature with contributions from several branches of the facial nerve, including the frontal, zygomatic, and buccal branches (Figure 46.3). Cadaver dissection reveals a diffuse network of nerves innervating the orbicularis oculi. It is important to recognize that the buccal branches supply a plexus of nerve branches to the medial orbicularis in both the upper and lower eyelids that contribute to voluntary and involuntary lid closure (Figure 46.4). Therefore, proper lateral canthal anchoring and preservation of buccal innervation are important principles in avoiding lower lid malposition and problems with eyelid closure following lower lid blepharoplasty.
The Posterior Lamella and the Tarsoligamentous Structures
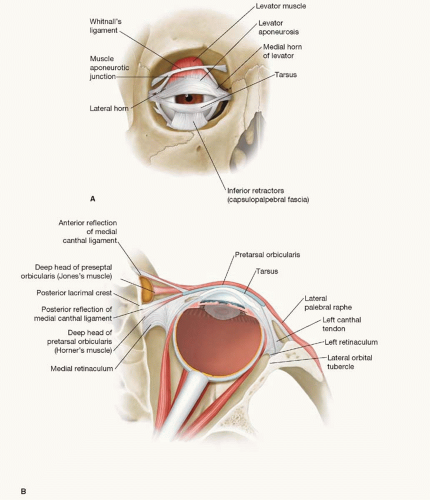
While the skin and muscle make up the anterior lamella, the tarsoligamentous sling creates the support structure for the posterior lamella (Figure 46.5). The tarsal plates constitute the connective tissue framework of the upper and lower eyelids. The upper lid tarsal plate is approximately 24 mm horizontally and 8 to 10 mm vertically at its widest dimension. Attachments of the upper lid tarsal plate include the pretarsal orbicularis and levator aponeurosis on the anterior surface, Muller’s muscle on the superior border, and conjunctiva on the posterior surface. The lower lid tarsal plate is approximately 24 mm in horizontal dimension and 4 mm in vertical dimension. Attachments to the lower lid tarsal plate include the pretarsal orbicularis, capsulopalpebral fascia, and conjunctiva. The tarsal plates of the upper and lower eyelid are attached to the orbit by the medial and lateral canthal ligaments and retinacular support structures.
The medial canthus is a complex support structure that forms the medial fixation point for the medial commissure. It consists of an anterior reflection, which inserts anterior to the lacrimal sac on the nasolacrimal crest, and a posterior reflection, which inserts deep to the lacrimal sac on the posterior lacrimal crest. The medial retinaculum is formed by several structures, including the deep head of the pretarsal orbicularis, orbital septum, and medial extension of Lockwood’s ligament, medial horn of the levator aponeurosis, medial rectus cheek ligaments, and Whitnall’s ligament. The medial retinaculum represents a fixed point maintaining medial canthal position, allowing the orbicularis muscles to act on lid position rather than medial canthal position (Figure 46.6). The lateral canthus also functions as an integral fixation point for the lower lid. The lateral canthal ligament is formed by the fibrous crura, which connects the tarsal plates to Whitnall’s bony lateral orbital tubercle within the lateral orbital rim. In addition, the lateral retinaculum is formed by several ligamentous structures from the lateral horn of the levator aponeurosis, lateral rectus check ligaments, Whitnall’s suspensory ligament, and Lockwood’s inferior suspensory ligament. Although the lateral retinaculum represents the lateral point of fixation, there is some mobility of the lateral commissure to increase the visual field upon lateral gaze. This mobility predisposes the lateral canthus to laxity and medial migration with age or trauma compared with the immobile medial canthus.
In addition to the tarsal plates and canthal ligaments, support structures in the upper and lower eyelid stabilize the tarsoligamentous sling. The superior transverse ligament of Whitnall is partially formed by the fascia of levator palpebrae superioris. Whitnall’s ligament inserts medially at the trochlea of the superior oblique and laterally at the lacrimal gland pseudocapsule and the frontal bone of the lacrimal sac fossa. The lower eyelid has an analogous inferior suspensory ligament, Lockwood’s ligament, which arises from the medial and lateral retinaculum and fuses with the capsulopalpebral fascia inserting on the inferior tarsal border. It functions to stabilize the lower lid on downward gaze, while the lower lid retractors cause depression of the lower lid to increase the inferior visual field during downgaze.
Retractors of the Upper and Lower Lids
The upper eyelid retractors include the levator palpebrae superioris muscle and Muller’s superior tarsal muscle. The
levator muscle is striated muscle innervated by the oculomotor nerve (cranial nerve III). The levator muscle originates from the lesser wing of the sphenoid and inserts along the anterior surface of the tarsal plate. The levator muscle becomes aponeurotic 5 to 7 mm above the superior border of the tarsus and 10 to 14 mm below Whitnall’s ligament. The levator aponeurosis has a lateral horn that divides the lacrimal gland into orbital and palpebral lobes and inserts into the lateral orbital tubercle and lateral retinaculum as well as the capsulopalpebral fascia of the lower eyelid. The medial horn of the levator aponeurosis inserts into the posterior reflection of the medial canthal tendon. Together, the medial and lateral horns distribute the force of the levator muscle equally along the aponeurosis, causing the majority of lid elevation to occur centrally.
levator muscle is striated muscle innervated by the oculomotor nerve (cranial nerve III). The levator muscle originates from the lesser wing of the sphenoid and inserts along the anterior surface of the tarsal plate. The levator muscle becomes aponeurotic 5 to 7 mm above the superior border of the tarsus and 10 to 14 mm below Whitnall’s ligament. The levator aponeurosis has a lateral horn that divides the lacrimal gland into orbital and palpebral lobes and inserts into the lateral orbital tubercle and lateral retinaculum as well as the capsulopalpebral fascia of the lower eyelid. The medial horn of the levator aponeurosis inserts into the posterior reflection of the medial canthal tendon. Together, the medial and lateral horns distribute the force of the levator muscle equally along the aponeurosis, causing the majority of lid elevation to occur centrally.
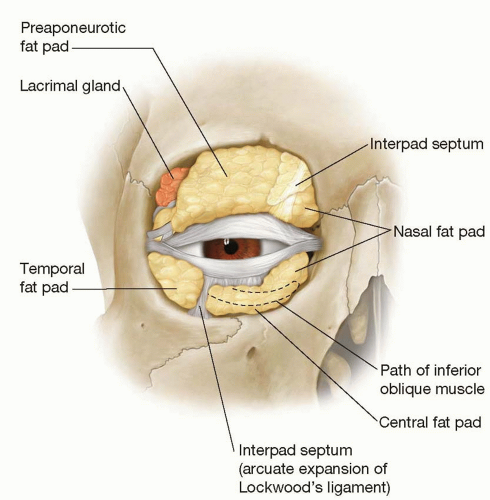 FIGURE 46.6. Anatomy of the orbital fat pads and the interpad septae that are addressed during blepharoplasty. |
Muller’s muscle is smooth muscle, which originates from the posterior surface of the levator muscle and inserts into the superior tarsal border. Muller’s muscle is innervated by the sympathetic nervous system.
Upper lid ptosis can be caused by mechanical dehiscence of the levator aponeurosis, abnormalities of cranial nerve III, or loss of sympathetic nerve supply causing Muller’s muscle weakness (Horner’s syndrome).
The lower lid retractors include the capsulopalpebral fascia and the inferior tarsal muscle, which are closely applied. The capsulopalpebral fascia originates from the inferior rectus fascia and envelops the inferior oblique muscle. The capsulopalpebral fascia is analogous to the levator aponeurosis of the upper lid and the inferior tarsal muscle is analogous to Muller’s muscle.
The Orbital Septum and Orbital Fat Pads
The orbital septum separates the anterior and posterior lamella and helps maintain periorbital fat within the anatomic confines of the orbit. The orbital septum originates from the orbital rim at the arcus marginalis and is discontinuous at the medial canthus. In the upper eyelid, the septum fuses with the levator aponeurosis, several millimeters above the tarsal plate. In the lower lid, the septum fuses with the capsulopalpebral fascia below the tarsal plate. There are numerous fibrous structures that separate the central and nasal fat pads in the upper eyelid and the central and lateral fat pads in the lower eyelid. Appreciation of the anatomy of the septum is important particularly when surgical procedures such as resetting, tightening, and excising the septum are performed.
The periorbital fat pads are found posterior to the orbital septum (Figure 46.6). There are two main fat pads in the upper eyelid and three fat pads in the lower eyelid. The two upper fat pads are referred to as the central and nasal fat pads and are located in the preaponeurotic space just superficial to the levator aponeurosis. The interpad septum separates the central and nasal fat pads and is continuous with a septal fascial connection to the trochlea. The nasal fat pad is more fibrous and pale in color compared with the central fat pad. The medial palpebral artery is located in the medial fat pad and can cause significant bleeding during blepharoplasty. The central fat pad is superficial to the levator aponeurosis in the so-called preaponeurotic space and contributes to the fullness of the upper lid fold.
There are three fat pockets in the lower eyelid: central, nasal, and lateral. The nasal compartment in the lower eyelid is similar to its counterpart in the upper eyelid. The inferior oblique muscle commonly visible during blepharoplasty separates the nasal and central fat compartments. The central and lateral fat compartments are also separated by an interpad septum as well as a fascial extension from Lockwood’s ligament, the arcuate expansion. The arcuate expansion of Lockwood’s ligament should be preserved during lower lid dissection to maintain lateral lid support. Since the nasal and central fat pads envelope the inferior oblique muscle, aggressive fat transposition techniques that suture the fat below the rim can result in diplopia from impaired inferior oblique function. The lateral extent of the lateral fat pocket includes the lateral retinaculum and lateral canthal tendon.
The Lacrimal Gland
The lacrimal gland lacks a true capsule and is divided into the orbital and palpebral lobe by the lateral horn of the levator. The orbital lobe is positioned in the fossa glandulae lacrimalis, which is a shallow fossa in the frontal bone at the superolateral orbit. The smaller palpebral lobe is connected to the orbital lobe by an isthmus posterior to the lateral horn of the levator. Lacrimal gland ptosis is caused by dehiscence of Sommering’s ligaments, which are the fibrous interlobular septa that connect the gland to the orbital rim fossa. Fullness in the lateral aspect of the upper eyelid is often caused by lacrimal gland ptosis. Lateral to the lacrimal gland is a separate compartment, just above Whitnall’s tubercle, called Eisler’s pocket. Eisler’s fat pad is a small accessory fat pad located in Eisler’s pocket, which serves as a useful anatomical landmark for Whitnall’s tubercle. The location of this fat pad is clinically useful during placement of the lateral canthoplasty suture.
The Conjunctiva
The most posterior layer of the eyelid is the conjunctival lining, which continues over Tenon’s capsule. The palpebral portion of the conjunctiva is closely adherent to the posterior surface of the tarsal plate and the lid retractors. At the fornix, the conjunctiva is termed bulbar conjunctiva and overlies the globe up to the corneoscleral limbus. Small accessory glands are located within the conjunctiva creating the aqueous portion of the tear film.
Forehead Anatomy
In the superior and lateral orbit, the forehead is more firmly attached to the underlying periosteum. Specifically, there is fibrous fusion between the orbicularis fascia and the underlying periosteum and deep temporal fascia. These attachments are released to mobilize the forehead for browlifting. The frontalis muscles are brow elevators and are continuous with
the galea aponeurotica and the occipitalis posteriorly. The frontalis muscles insert into the dermis above the supraorbital rim and are responsible for transverse forehead furrows.
the galea aponeurotica and the occipitalis posteriorly. The frontalis muscles insert into the dermis above the supraorbital rim and are responsible for transverse forehead furrows.
The orbital orbicularis oculi, depressor supercilii, oblique and transverse heads of the corrugator supercilii, and procerus muscles act in synergy to depress the medial brow and produce glabellar furrows. Motor innervation to the frontalis and superior orbicularis oculi is by the frontal (temporal) branches of the facial nerve. The brow depressors receive motor innervation from the buccal and zygomatic branches in addition to the frontal branches.
Midfacial Anatomy
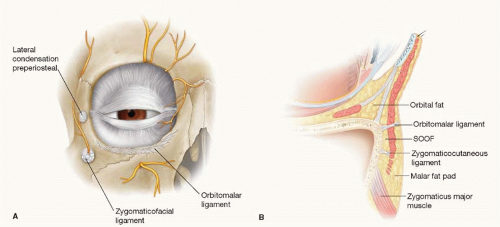
Knowledge of anatomy in this region allows understanding of the changes seen in the lower eyelid/cheek junction. Mendelson described the prezygomatic space. The upper border of the prezygomatic space is formed by the orbitomalar ligament (also called the orbicularis retaining ligament), a structure that arises from a thickened area of periosteum inferior to the inferior orbital rim inserts on the deep surfaces of the orbicularis muscle (Figure 46.7). The orbitomalar ligament along with the origin of the orbicularis from the bone below the infraorbital rim is responsible for defining the tear trough and its lateral continuation, the lid-cheek junction (Figure 46.8). The lower border of the prezygomatic space is framed by the zygomatic ligaments. From the skeletal plane, these osteocutaneous ligaments radiate outward to insert into the dermis of the cheek. This prezygomatic space is triangular in shape with the apex being nasal. Malar mounds are the result of edematous fat in the prezygomatic space.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree