Biomechanical Considerations Following Breast Reconstruction with Abdominal Flaps
Maurice Y. Nahabedian
Scott L. Spear
Christopher L. Hess
Introduction
The lower abdomen has been the principal donor site for breast reconstruction using autologous tissue. The reasons for this are several and include sufficient volume skin and fat, relative ease of transfer, high-quality aesthetic value, and generally acceptable donor-site morbidity. The donor-site morbidities related to flap transfer have always been a consideration when raising abdominal flaps, and numerous studies have been performed to examine this.
Since the second edition of this chapter, there have been several studies that have further evaluated the abdominal wall following breast reconstruction with abdominal flaps. In addition to the pedicle transverse rectus abdominis myocutaneous (TRAM), free TRAM, and deep inferior epigastric perforator (DIEP) flaps that were reviewed in the second edition, the superficial inferior epigastric artery (SIEA) flap will be reviewed in this chapter. These four flaps are now accepted as viable options for breast reconstruction utilizing the abdomen as the donor site. The principal differences among these flaps relate to the amount of rectus abdominis muscle and anterior rectus sheath that are removed. It is generally accepted that the transfer of one or both rectus abdominis muscles will alter the normal physiology of the trunk to some degree. Given that there are now four different flaps that can be performed from the abdominal donor site, the question that is frequently posed is whether the biomechanical changes associated with one flap or another are significantly different and whether these changes translate into a significant deficit in normal function. The intent of this review is to examine the issue of aesthetic, biomechanical, and functional changes of the trunk that occur with or without transfer of the rectus abdominis muscles.
Rectus Abdominis
Anatomy and Physiology
The rectus abdominis muscles extend from the pubic crest and symphysis pubis to the cartilages of the fifth, sixth, and seventh ribs. There are usually three tendinous inscriptions, which are located at the level of the xiphoid process, the umbilicus, and midway in between (1). These inscriptions connect the rectus muscle with the anterior rectus sheath. The innervation to the rectus abdominis is from the ventral rami of the inferior six thoracic nerves that usually enter the muscle at the junction of the central and lateral third. The blood supply is from the superior epigastric and deep inferior epigastric arteries. Upon entering the muscle, each superior epigastric artery frequently divides into three branches that include a medial and lateral muscular branch and a costomarginal branch that merges with the eighth posterior intercostal artery (2). The deep inferior epigastric artery enters the muscle near the arcuate line and frequently divides into one to three intramuscular branches, which ascend to meet corresponding vessels from the superior epigastric artery. The main intramuscular branches from the deep inferior epigastric vessel are usually located within the central third of the muscle.
The rectus abdominis muscles serve several important functions (3). Although they are thought of as the primary flexors of the trunk, their primary function is to initiate flexion of the trunk, and they are responsible for the first 30 deg of trunk flexion. The iliopsoas muscle is principally involved for 60 deg, with a lesser emphasis on the rectus abdominis. The rectus abdominis muscles are also the insertion site for the oblique musculature as well as the transverses abdominis muscle and therefore help in both rotatory movements and to compress the abdominal viscera, such as during Valsalva. In addition, these muscles work in concert with the spine to depress the ribs and stabilize the pelvis during walking. This fixation of the pelvis enables the thigh muscles to act effectively. Similarly, during lower limb lifts from the supine position, the rectus abdominis muscles contract to prevent tilting of the pelvis by the weight of the limbs. Finally, these muscles are important in stabilizing the trunk when lifting an object from the standing position.
Ever since the first use of the TRAM flap for reconstructive purposes there has been a concern regarding the mechanical compromise of the abdominal wall. Questions about perceived abdominal wall weakness, true wall weakness, and wall laxity have led many investigators to study the issue. Unfortunately, this issue is made even more complicated by the many variations of TRAM flap (single pedicle, double pedicle, bilateral, free, DIEP), the method of fascial closure (single layer, multiple layer, mesh), and the amount of muscle removed (whole muscle, muscle sparing). It is important to realize that whenever a myotomy is created, scar tissue will form. This scar tissue will compromise the normal contractile elements of the rectus abdominis muscle to some degree that may limit abdominal strength. The important question is whether these changes are clinically significant in terms of disrupting activities of daily living. To answer these questions, a number of well-controlled studies have been conducted looking at the various types of abdominal flaps with the hope of improving our understanding of this important and controversial topic.
The Abdominal Flaps
Pedicled Transverse Rectus Abdominis Myocutaneous Flaps
The pedicle or conventional TRAM flap has been and continues to be the principal method of breast reconstruction using
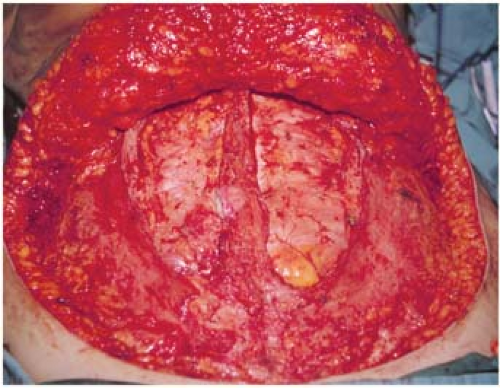
abdominal flaps. Annual procedural updates from the American Society of Plastic Surgeons demonstrate that nearly 75% of autologous reconstruction is performed using the conventional TRAM flap (4). Since its initial description in 1982 by Hartrampf et al. (5), various modifications have been proposed to improve aesthetic and functional outcomes. These include muscle-sparing techniques and additional reinforcement of the anterior abdominal wall. The pedicle TRAM flap can be performed by utilizing the entire rectus abdominis muscle (Fig. 75.1) or by sparing lateral and/or medial strips of the muscle (Fig. 75.2).
abdominal flaps. Annual procedural updates from the American Society of Plastic Surgeons demonstrate that nearly 75% of autologous reconstruction is performed using the conventional TRAM flap (4). Since its initial description in 1982 by Hartrampf et al. (5), various modifications have been proposed to improve aesthetic and functional outcomes. These include muscle-sparing techniques and additional reinforcement of the anterior abdominal wall. The pedicle TRAM flap can be performed by utilizing the entire rectus abdominis muscle (Fig. 75.1) or by sparing lateral and/or medial strips of the muscle (Fig. 75.2).
In the early era of TRAM flap surgery it became apparent that it was imperative not only to raise a viable flap, but also to ensure that the abdominal donor site remained competent. Most published studies reported an incidence of abdominal hernia or bulge that generally ranged between 0% and 2% (Table 75.1) (2,6,7,8,9,10,11). In almost all reports, a synthetic mesh such as Marlex was used to reinforce the anterior abdominal wall following transfer of the TRAM flap. Despite the reported low incidence of abdominal bulge or hernia in these studies, several other studies reported a much higher incidence of abdominal bulge or hernia that ranged between 25% and 35% (10,12). The primary explanation for the wide range of difference was most likely related to the various methods of flap harvest, variations in the technique for closure of the abdominal wall, and the definitions used of what constitutes abnormal abdominal contour.
Table 75.1 Abdominal Morbidity Following Pedicle Transverse Rectus Abdominis Myocutaneous Flaps | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
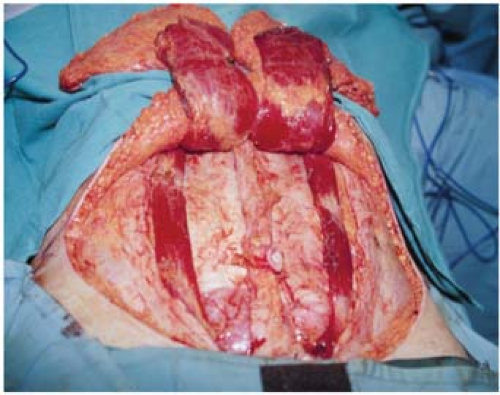 Figure 75.2. A muscle-sparing bilateral pedicle transverse rectus abdominis myocutaneous flap (MS-1). |
There have been many descriptions relating to the optimal method of closure of the anterior abdominal wall following a pedicle TRAM flap. These include the use of relaxing incisions, one- or two-layer fascial closure, use of a synthetic or biologic mesh, location of the mesh (inlay or onlay), and the type and thickness of suture material used. In 1987, Hartrampf and Bennett reported the outcome of 383 TRAM flap reconstructions in 300 patients followed at least 1 year after surgery (8). On the basis of using the muscle-sparing TRAM flap technique
with two-layered closure, there were 194 unilateral, 23 double-pedicle, and 83 bilateral reconstructions performed. Abdominal morbidities included a lower abdominal hernia in 1 woman (0.3%), a small defect of the upper anterior rectus sheath in 2 women (0.8%), and lower abdominal laxity in 2 women (0.8%). All complications occurred in unilateral single-pedicle reconstructions.
with two-layered closure, there were 194 unilateral, 23 double-pedicle, and 83 bilateral reconstructions performed. Abdominal morbidities included a lower abdominal hernia in 1 woman (0.3%), a small defect of the upper anterior rectus sheath in 2 women (0.8%), and lower abdominal laxity in 2 women (0.8%). All complications occurred in unilateral single-pedicle reconstructions.
The Hartrampf data were updated in 1994 following a 13-year experience with 662 TRAM flap reconstructions (2). A total of 296 single-pedicle, 146 double-pedicle, 214 bilateral, and 6 turbocharged TRAM flap reconstructions were performed. On the basis of using the two-layer permanent suture closure technique, the reported incidence of hernia or abdominal wall laxity was less than 2%. In bilateral reconstructions, a synthetic mesh overlay was used with a reported incidence of bulge or hernia that was slightly increased.
Utilizing a similar two-layer closure technique, Lejour and Dome evaluated 57 patients following delayed breast reconstruction with whole-muscle pedicled TRAM flaps (9). Of these patients, 33 underwent single-pedicle and 24 underwent double-pedicle or bilateral single-pedicle reconstructions. The abdominal fascial defects were closed in two layers with Teflon mesh sutured under tension to the lateral margins of the rectus sheath with the anterior fascia approximated over the mesh. Patients were evaluated subjectively by questionnaire and objectively by clinical examination and their ability to do sit-ups and reverse straight-leg raises. The authors reported no hernias or wall laxity. However, 1 patient (4%) with a bilateral reconstruction developed an infection requiring mesh removal. Subsequently, she developed abdominal weakness and bulging.
The indications for the use of synthetic mesh for abdominal closure are somewhat subjective and not always clear. Whether the mesh is used as an interposition graft or an onlay graft over a two-layered fascial closure, the literature indicates that the rate of abdominal morbidity is the same as for a two-layered closure with permanent suture (7,9,10,11,13). When the fascial defect is large and/or the quality of the anterior sheath is weak, there is a potential for the suture to pull through when placed under tension. In these circumstances synthetic mesh can be used as an inlay or onlay graft to reinforce the abdominal wall to prevent bulging. If sutured in an onlay fashion, it is recommended that the mesh be sutured to the internal oblique as well as the external oblique fascia.
Zienowicz and May examined abdominal outcomes following fascial repair with an interposition (inlay) synthetic mesh and imbrication of the contralateral rectus sheath (11). Whole-muscle, single-pedicle TRAM flap reconstruction was performed in 65 women with a follow-up that ranged from 12 to 115 months. The authors reported 1 lower abdominal hernia that resulted from disruption of a mesh suture line and 1 epigastric bulge that was only noticeable on performing sit-ups. The epigastric bulge was felt to be the dog-ear from the lower fascial closure. Thus, an overall hernia rate of 1.5% was reported, with no abdominal wall weakness.
The use of biologic graft material that include acellular dermal matrices has received increased attention as an alternative to synthetic mesh to repair or reinforce that anterior abdominal wall following TRAM flap surgery. Glasberg and D’Amico reported on the results of using an acellular dermal matrix in 54 patients following pedicle TRAM flap surgery (14). The matrix was sutured to the fascial edges in an inlay fashion. No woman developed a hernia, although the incidence of abnormal contour/bulge was 16% in the second arm of the study. Recommendations include suturing the material under tension, reducing the size of the matrix by 25% relative to the fascial defect, and aggressively using drains.
An alternative or adjunct to synthetic mesh or acellular dermal matrix is the use of relaxing incisions. Scheflan and Kalisman utilized this technique and reported on the results of 140 pedicle TRAM flaps (7). The initial method of abdominal closure was to perform a lateral relaxing incision along the external oblique and to close the anterior rectus sheath in one layer. This method resulted in weakness of the anterior abdominal wall in 15 patients (10.8%). This technique was subsequently modified by closing the anterior rectus sheath in two layers and also incorporating Prolene or Marlex mesh as an interposition graft. The authors reported that in 60 women who were closed in this fashion, only 1 (1.7%) was noted to have a bulge at the site of closure. The value of a two-layered fascial closure was emphasized in this study; however, there was no mention of the method of muscle harvest or of contralateral wall bulging or weakness.
The issue of abdominal wall weakness following pedicle TRAM flap surgery has generated significant controversy. The literature indicates that the percentage of patients who can perform a sit-up following a single-pedicle TRAM flap ranges from 23% to 83%; following bilateral/double-pedicle TRAM flaps it is 0% to 40% (9,10,13,15). Bilateral TRAM flap reconstruction can result in significant postoperative abdominal wall weakness; however, this can be minimized by limiting the amount of muscle removed and preserving the intercostal innervation to the remaining muscle. Subjective patient complaints of decreased abdominal wall strength for unilateral pedicled TRAM flaps range from 25% to 44% and for bilateral/double-pedicle TRAM flaps from 43% to 60% (9,10,13,15). Although there is a paucity of literature comparing bilateral free TRAM flaps to bilateral pedicled TRAM flaps, Kroll et al.’s paper appropriately illustrates the greater decreased sit-up ability following a bilateral pedicle TRAM when compared to a bilateral free TRAM (13).
In summary, it is clear that a two-layer closure following a pedicle TRAM flap is important to minimize the incidence of abdominal bulge or hernia. The use of adjunct maneuvers such as relaxing incisions, synthetic mesh, or biologic mesh can further minimize abdominal morbidity. Abdominal strength is compromised to varying degrees following harvest of the rectus abdominis muscle.
Free Transverse Rectus Abdominis Myocutaneous Flaps
Although first described by Holmstrom in 1979, it was not until the late 1980s that the benefits and utility of the free TRAM were appreciated (16). The initial indication for the free TRAM was to improve upon the vascularity of the flap in order to minimize the incidence of fat necrosis and partial flap loss. It was later appreciated that various muscle-sparing maneuvers could also minimize the abdominal weakness associated with full-width muscle harvest. Table 75.2 summarizes the results of several frequently cited studies (13,15,17,18,19).
It is important to understand that the free TRAM can be classified into three categories based on the degree of muscle sacrifice (12,20,21). This classification is based on a muscle-sparing concept and subdivides the rectus abdominis muscle
into thirds (medial, central, and lateral). The MS-0 (muscle sparing—none) includes the full width of the rectus abdominis muscle, resulting in a total loss of muscle continuity. This type of free TRAM is functionally no different than a pedicle TRAM in which the entire with of the muscle is harvested. The MS-1 includes either the medial or lateral segment of the rectus abdominis muscle. This has the advantage of leaving the muscle in continuity. The MS-2 includes only the central segment of the rectus abdominis muscle and spares the medial and lateral third (Fig. 75.3). This type of free TRAM usually leaves 60% to 80% of the width of the muscle intact, as well as preserves the lateral intercostal innervation.
into thirds (medial, central, and lateral). The MS-0 (muscle sparing—none) includes the full width of the rectus abdominis muscle, resulting in a total loss of muscle continuity. This type of free TRAM is functionally no different than a pedicle TRAM in which the entire with of the muscle is harvested. The MS-1 includes either the medial or lateral segment of the rectus abdominis muscle. This has the advantage of leaving the muscle in continuity. The MS-2 includes only the central segment of the rectus abdominis muscle and spares the medial and lateral third (Fig. 75.3). This type of free TRAM usually leaves 60% to 80% of the width of the muscle intact, as well as preserves the lateral intercostal innervation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree