For the clinician a clear knowledge of the most common benign tumors and important. Identifying a lesion that falls outside of the spectrum of common benign tumors and requires further evaluation or referral is critical. This fundamental insight will help alleviate the concern of a patient who presents with an otherwise benign lesion. It will also allow the clinician to first screen and differentiate common lesions that may have simple treatments, or no required treatment, from those lesions that are of more concern.
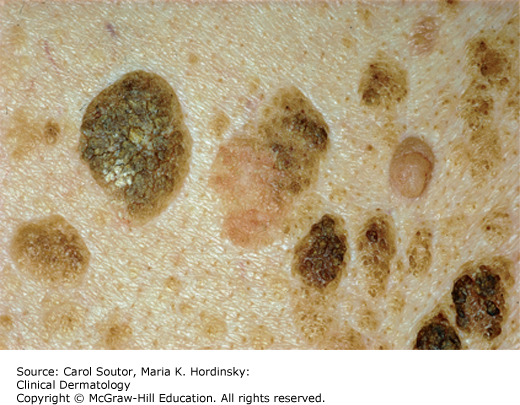
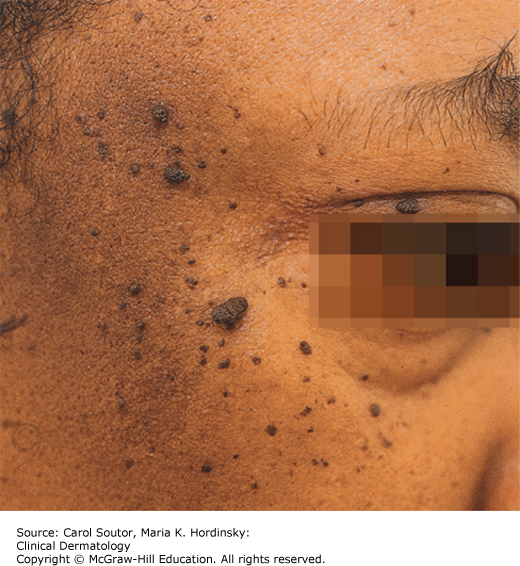
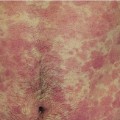
Seborrheic keratoses are present in approximately 50% of adult patients. Many patients present with a history of a changing pigmented “mole” and a concern about melanoma. Patients may complain of pruritus or irritation from clothing. A classic seborrheic keratosis has a predilection for the trunk and presents as a well-defined hyperpigmented papule or plaque with a waxy hyperkeratotic surface, ranging in size from a few millimeters to several centimeters in diameter (Figure 16-1). They are often oval in shape with their long axis following the natural tension lines of the skin. The astute clinician can quickly recognize these lesions and avert the need for a biopsy, but occasionally even with the most trained eye a biopsy is indicated. Variants include the macular seborrheic keratosis of the face and scalp that present as a slightly raised velvety plaque or pigmented macule on the head and neck. These lesions are often misdiagnosed as a lentigo with concern for lentigo maligna melanoma. A facial variant is dermatosis papularis nigra which presents primarily in African Americans with small dark papules (Figure 16-2). Stucco keratosis is another variant and presents as smaller scattered lightly pigmented or white keratotic papules on the distal lower extremities (Figure 16-3).
Histopathology shows that all variants of seborrheic keratosis are limited to thickening of the epidermis with trapping of keratin in elongated tracks called horn pseudocyts. These can be seen under dermoscopy or by careful observation with the unaided eye.
✓ Lentigo: Macule with even hyperpigmentation and a smooth scalloped border, most commonly on sun-exposed areas of face and hands.
✓ Nevus: Tan to black macules or papules; surface is not hyperkeratotic or waxy.
✓ Melanoma: Hyperpigmented macule/papule with irregular color, border, and shape.
There is no specific treatment that is required other than differentiated seborrheic keratoses from other lesions that would have malignant potential. For irritated or disfiguring lesions, cryotherapy (Chapter 7) can be beneficial. Care must be taken however to not over-treat as a scar can replace the lesion. Patients must be warned that with any treatment persistent hypo- or hyper-pigmentation may occur. Alternative treatments include electrocautery or desiccation with or without curettage.
Lesions that cannot be clearly defined as benign.
American Academy of Dermatology: www.aad.org/skin-conditions/dermatology-a-to-z/seborrheic-keratoses
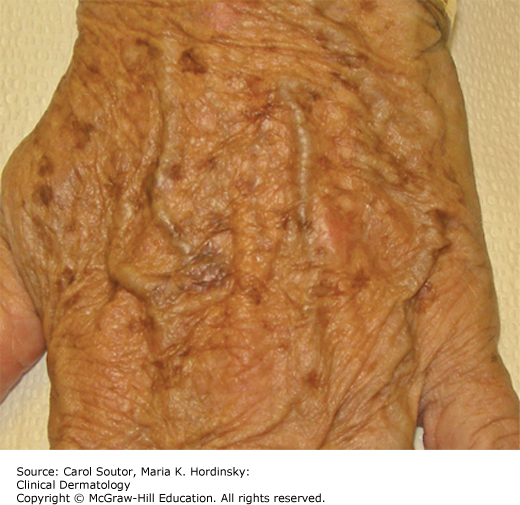
Lentigines are common benign hyperplasias of melanocytes. They are usually acquired, but occasionally are congenital, especially as part of congenital syndromes such as LEOPARD (Moynahan) syndrome and Peutz–Jeghers syndrome. They commonly begin in the third decade of life and present as light or dark brown macules with sharp borders in sun-exposed skin, primarily dorsal hands (Figure 16-4), forearms, and shoulders. They may also occur on mucous membranes and the nail bed. Lentigo simplex occurs without ultraviolet exposure and can develop as early as the first decade of life. These present as sharply marginated monochromatic light or dark brown macules. Patients rarely bring lentigines to medical attention except in the context of “unsightly” age spots or concern for melanoma.1
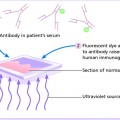
Histopathology shows an increased number of melanocytes in the basal cell layer of the epidermis.
✓ Lentigo maligna: Macular hyperpigmentation, in a similar distribution, but with variations in color and irregular border, typically in older adults.
Lentigines do not have a medical indication for removal. Common cosmetic management techniques include bleaching creams (eg, hydroquinone) and cryotherapy. Prevention is the best approach to solar lentigines with the regular use of sunscreens. The natural history of lentigines is to persist over time and darken with age and sunlight exposure.
Cosmetically bothersome lentigines can be referred for laser and intense pulsed light treatment (monochromatic noncoherent light visible light).
Most patients present with concern over a symptomatic “mole.” The classic presentation of a dermatofibroma is a firm 3- to 10-mm papule or nodule on the distal lower extremities that may have an associated increase in pigmentation (Figure 16-5). The etiology of these lesions is not certain, but is thought to be related to a healing process from a minor traumatic event that leads to proliferation of dermal fibroblasts. The pigmentation of these lesions is symmetrical often with a lighter central area and a collaret of darker pigmentation. Horizontal compression, or pinching of the lesion, leads to dimpling due to the deep collagen connection (dimple sign). Dermatofibromas can entrap nerves within the scar leading to sensations of itch or sensitivity.
Histopathology shows a localized area of spindle cell proliferation of fibroblasts in the dermis.
✓ Nevus: Tan to dark, brown, soft macule or papule. Dimple sign is negative.
✓ Dermatofibrosarcoma protuberans: Firm nodule similar to a dermatofibroma, but larger in size and has progressive growth with time.
✓ Melanoma: Flat or raised lesion with variable pigment and irregular borders.
Treatment options are limited. Intralesional triamcinolone injections and cryotherapy can be used, but may have limited success. Reassurance of the benign nature of the lesions with no treatment is appropriate for asymptomatic lesions. Those lesions with prominent itch or tenderness can be surgically removed with the caveat that the patient is trading the round scar of a dermatofibroma for a linear scar of the excision.
Lesions with continued growth, poorly defined lesions.
British Association of Dermatologists: www.bad.org.uk/site/809/Default.aspx
Skin tags are very common skin-colored papules with a thin stalk (Figure 16-6). The stalk contains a central blood vessel. They most commonly present in patients in their mid-40s to late 60s in sites of friction such as the neck, axillae, and groin. Weight gain correlates with an increased incidence.
Histopathology shows loose fibrous tissue in the dermis of a polyp with a thin epidermis.
✓ Neurotized nevus: Very similar appearance to skin tags, but presents as single lesion.
✓ Neurofibroma: May be polypoid, but typically are larger than skin tags, and may present within the context of a genetic syndrome.
Cryotherapy can be useful in treating multiple skin tags, but success is limited to lesions that have a narrow stalk. Broad-based lesions are best treated with thin shave excision. Electrodessication and removal with iris scissors can be used for smaller lesions. Any treatment often leaves behind a small hypopigmented macule.
Numerous lesions.
PubMed Health: www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001851/
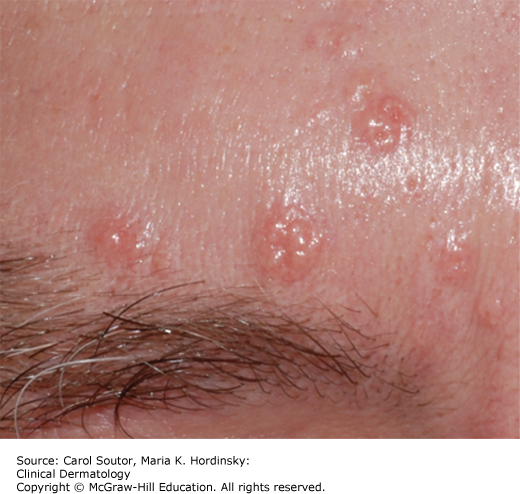
Sebaceous hyperplasia presents as a 2- to 4-mm yellow- to skin-colored papule(s) on the central face and forehead (Figure 16-7). They represent a hyperplasia of sebaceous glands. They often have a central depression.
Histopathology shows hyperplasia of sebaceous glands.
✓ Milia: 1- to 2-mm white cyst with no central depression.
✓ Basal cell carcinoma: Small basal cell carcinomas, have a similar appearance, but grow continuously.
✓ Acne: Transient erythematous inflammatory papules lasting less than 2 months.
Lesions that are progressive or show symptoms of tenderness or bleeding should be biopsied to rule out basal cell carcinoma. Observation is sufficient for stable lesions. Cosmetically bothersome lesions can be treated with shave removal with or without electrodessication. Electrodessication on its own can be used as well for smaller lesions. A small scar is often left after treatment.
Lesions with progressive growth.
A lipoma represents a localized overgrowth of fat cells. A lipoma often presents as a rubbery nodule in areas of potential inadvertent trauma (Figure 16-8). The tendency to form lipomas appears to run in families and a number of syndromes present with multiple lipomas that may number from a few to hundreds. Lipomas come in two main variants, classic and angiolipoma. The angiolipoma variant clinically is similar to the classic lipoma but may have an associated tenderness. These lesions lead to a deep aching sensation with minor pressure or trauma and can be quite distressing to the patient.
Figure 16-8.
Lipoma. Soft skin-colored nodule on back.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree