Augmentation with Periareolar Mastopexy
Scott L. Spear
Mark L. Venturi
Despite decades of use, breast augmentation with periareolar mastopexy remains a complex and controversial subject. According to some, augmentation with periareolar mastopexy represents a disproportionate number of legal problems in plastic surgery. Whether this is because it is a commonly performed procedure or because it is a procedure prone to mischief is hard to tell. This operation comes into play because many women who seek breast augmentation, in fact, would benefit from a mastopexy to achieve a reasonable result without the use of an overly large implant. Certainly one of the difficulties with augmentation with periareolar mastopexy has been its use either when it was not required or, on the other hand, when it was of insufficient power to solve the problem. This chapter, therefore, will focus on the indications for augmentation with periareolar mastopexy as well as the techniques of marking and surgical execution. We finish up with a discussion of complications, revision surgery, and medical legal issues.
The ideal indication for augmentation with periareolar mastopexy is the patient who seeks a breast augmentation but has too much ptosis on the one hand for augmentation alone but, on the other hand, too little ptosis to justify a more extended mastopexy. From the outset, part of the difficulty in picking the right patient for this operation has to do with inadequate tools for measuring breast ptosis.
Historically, breast ptosis was most commonly described according to Paula Regnault’s classification of ptosis as: glandular ptosis, mild ptosis, moderate ptosis, and severe ptosis. Glandular ptosis, or pseudoptosis, was when the nipple was above the inframammary fold but the breast overhung the inframammary fold. Grade I (mild) ptosis was a nipple at the fold, grade II (moderate) was the nipple 1 to 3 cm below the fold but on the anterior surface of the breast, and grade III (severe) ptosis was the nipple more than 3 cm below the fold and pointing toward the patient’s feet. This basic classification technique, however, did not take into account the size of the breast, the amount of skin on the breast, the position of the nipple in relationship to the breast gland, and, finally, the relationship of the breast gland to the chest wall. Depending on the size of the breasts and the amount of excess skin in the breast, it would be conceivable for a periareolar mastopexy to be satisfactory for a patient with moderate ptosis and the nipple below the fold, but be inadequate for a patient with mild ptosis and the nipple at the fold. The final decision regarding whether to perform a mastopexy and what kind of mastopexy to perform depends on the total surface area of breast skin and volume of the breast. Essentially, ultimately one must tailor the skin of the breast to fit the size of the newly enlarged breast, which includes both the current breast volume or parenchyma and the added volume from the implant. Thus, for a B-cup breast, 7 cm of skin between the nipple and inframammary fold may be sufficient, but for a D-cup breast, 10 cm of skin may be needed between the nipple and the inframammary fold.
As a general guideline, a mastopexy is not required when the nipple is above the inframammary fold or the areola is above the lower border of the breast such that there is unpigmented skin visible on the frontal view below the areola and there is no more than 2 to 3 cm of breast overhanging the inframammary crease. For a 4-cm-diameter nipple, this would mean that there would be approximately 6 cm of skin available between the nipple and the inframammary fold prior to the placement of an implant. Thus, there would be 6 cm of skin between the nipple and the fold to cover the surface of the newly enlarged breast including the current breast parenchyma and the breast implant volume.
A periareolar mastopexy is most appropriate for the patient where the nipple is near the inframammary fold, either just above, at, or slightly below the inframammary fold, the lower edge of the areola sits at the lower border of the breast when seen from the frontal view, and there is no more than 4 cm of breast overhanging the inframammary fold. This scenario would typically yield 6 to 8 cm of skin from the nipple to fold particularly when combined with a periareolar mastopexy.
Again, as a general guideline, when the nipple is at the bottom of the breast or pointing inferiorly, the nipple is below the inframammary fold by more than 2 cm, and the breast overhangs the inframammary fold by more than 4 cm, then either a vertical or a Wise pattern-type mastopexy would be appropriate and necessary to adequately tailor the breast skin to the new breast volume without distorting the nipple/areola shape.
It is one of the unique features of augmentation with a periareolar mastopexy that most often it does not make sense to do the mastopexy first in these patients because the mastopexy is part of a tailoring process to fit the breast skin and the nipple to the newly enlarged breasts. However, where there is doubt, it is acceptable to perform the augmentation first, preferably through a periareolar incision, and to hold off the mastopexy until a later date once the new breast has taken shape.
Technique
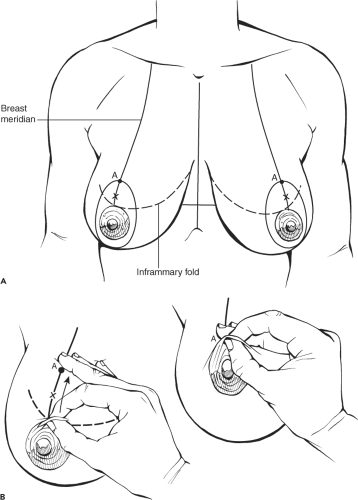
One of the interesting features of augmentation with periareolar mastopexy is the marking and the positioning of the nipple. Almost all breast surgery begins with the same standardized marks including drawing the midline, marking the inframammary folds, and drawing the meridian of the breast through the nipple and across the inframammary fold (Fig. 122.1A). A good way to check the appropriate height of the nipple is to pinch the upper edge of the areola on the patient who is sitting in the upright position and then lifting that skin up onto the breast itself to determine visually where the upper edge of the areola would best fit (Fig. 122.1B). This should be done at the same time as pulling down gently on the upper breast skin because when the nipple is sutured to the upper breast skin, it will tend to pull that skin down slightly. Again, in many patients, the nipple will need to be located 4 to 6 cm above the existing inframammary fold, which means that the upper edge of the areola will ultimately be 6 to 8 cm above the inframammary fold.
Although in breast reduction, siting the nipple at the inframammary fold or just above is often appropriate, in augmentation with periareolar mastopexy, the nipple should be located a minimum of 4 cm above the inframammary fold to allow adequate distance between the nipple and the fold once the implant has been placed. In some cases, the nipple may actually be located at as much as 5 cm or even 6 cm above the inframammary fold when performing augmentation with periareolar mastopexy. The sites of the new nipple location and the new upper edge of the areola are marked on the breast meridian. Medially and laterally, as a rule, minimal excess skin is removed and the lines are drawn so they diverge just around the areolar borders. Inferiorly, one must assess how much skin is desirable between the lower edge of the areola and the inframammary fold. Often this mark is just at the lower border of the old areola, but in some cases it may be slightly lower. After this point is drawn, an oval or somewhat circular pattern can be drawn around the existing areola. These marks are made indelibly on both sides with the patient in the upright position, and then the rest of the operation proceeds under either general anesthesia or sedation.
Although in breast reduction, siting the nipple at the inframammary fold or just above is often appropriate, in augmentation with periareolar mastopexy, the nipple should be located a minimum of 4 cm above the inframammary fold to allow adequate distance between the nipple and the fold once the implant has been placed. In some cases, the nipple may actually be located at as much as 5 cm or even 6 cm above the inframammary fold when performing augmentation with periareolar mastopexy. The sites of the new nipple location and the new upper edge of the areola are marked on the breast meridian. Medially and laterally, as a rule, minimal excess skin is removed and the lines are drawn so they diverge just around the areolar borders. Inferiorly, one must assess how much skin is desirable between the lower edge of the areola and the inframammary fold. Often this mark is just at the lower border of the old areola, but in some cases it may be slightly lower. After this point is drawn, an oval or somewhat circular pattern can be drawn around the existing areola. These marks are made indelibly on both sides with the patient in the upright position, and then the rest of the operation proceeds under either general anesthesia or sedation.
When there is doubt about whether to proceed with the mastopexy, the operation can begin with an augmentation done either through a periareolar incision (my preference) or through an inframammary or axillary incision. My preference is to perform these operations in the dual plane. That means that the pocket that is ultimately created is beneath the pectoralis major muscle in its uppermost portions but is subglandular in the lower 20% to 30% of the implant space. Going through the periareolar incision, dissection is carried out obliquely through the breast down toward the inframammary fold to damage as little of the breast parenchyma as possible (Figs. 122.2 and 122.3). After the plane between the breast and the chest wall muscles is encountered, the subglandular portion of the dissection is performed in the lowermost 20% to 30% of the anticipated pocket (Fig. 122.4). This always exposes the lower edge of the pectoralis major muscle, which is then grasped with an Allis clamp, and a subpectoral dissection is carried out superiorly, medially, and laterally. Particular attention must be paid to avoid getting beneath the pectoralis minor or serratus muscles laterally. Likewise, care should be taken not to overdissect the pectoralis major muscle medially. The pectoralis major muscle is released entirely across its lower portion but is not released along the sternal border (Fig. 122.5).
Ultimately, a confluent pocket is made which joins the pectoralis major dissection superiorly and a subglandular dissection inferiorly. The definitive implant or a sizer is then placed through the periareolar incision or through whichever incision was used. In those cases when proceeding with the mastopexy was uncertain, the patient can then be sat upright and the nipple-areola tailor tacked into the previously marked locations to assess their validity or to check whether any adjustments need to be done. In patients with whom one is more confident about the marking, the de-epithelialization can be performed first, reducing the areola down to a diameter of 38 to 42 mm.
Ultimately, a confluent pocket is made which joins the pectoralis major dissection superiorly and a subglandular dissection inferiorly. The definitive implant or a sizer is then placed through the periareolar incision or through whichever incision was used. In those cases when proceeding with the mastopexy was uncertain, the patient can then be sat upright and the nipple-areola tailor tacked into the previously marked locations to assess their validity or to check whether any adjustments need to be done. In patients with whom one is more confident about the marking, the de-epithelialization can be performed first, reducing the areola down to a diameter of 38 to 42 mm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree