Hip arthroscopy is a minimally invasive technique to address a variety of painful hip conditions in the athletic and prearthritic population.
 A surge in technologic development since the mid-1990s has allowed surgeons to effectively and reliably treat a variety of painful hip conditions arthroscopically.
A surge in technologic development since the mid-1990s has allowed surgeons to effectively and reliably treat a variety of painful hip conditions arthroscopically.
 The outcomes of hip arthroscopic techniques are equivocal to traditional, more invasive open techniques.2
The outcomes of hip arthroscopic techniques are equivocal to traditional, more invasive open techniques.2
 There is a tremendous learning curve when compared to knee and shoulder arthroscopy.
There is a tremendous learning curve when compared to knee and shoulder arthroscopy.
ANATOMY
 The hip is a constrained ball-and-socket joint, with the femoral head (ball) articulating with the acetabulum (socket) of the pelvis (FIG 1).
The hip is a constrained ball-and-socket joint, with the femoral head (ball) articulating with the acetabulum (socket) of the pelvis (FIG 1).
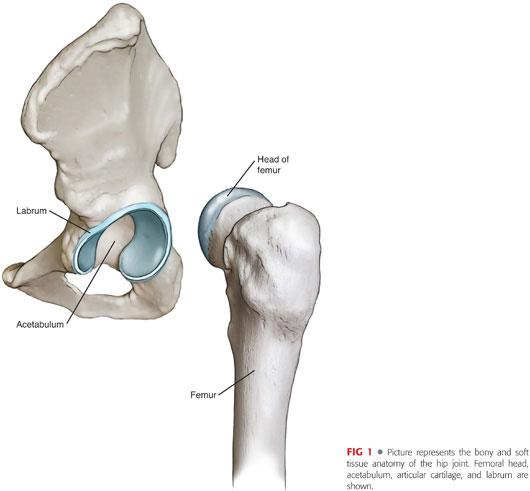
 The labrum is a pad of fibrocartilage attached to the acetabulum that deepens the acetabulum and provides stability to the hip as well as a “suction-seal” effect around the femoral head, providing a secure environment for the articular cartilage and synovial fluid6 (FIG 2).
The labrum is a pad of fibrocartilage attached to the acetabulum that deepens the acetabulum and provides stability to the hip as well as a “suction-seal” effect around the femoral head, providing a secure environment for the articular cartilage and synovial fluid6 (FIG 2).

 The alignment and shape of the hip is critical when determining the etiology of hip pain and thus proper treatment.
The alignment and shape of the hip is critical when determining the etiology of hip pain and thus proper treatment.
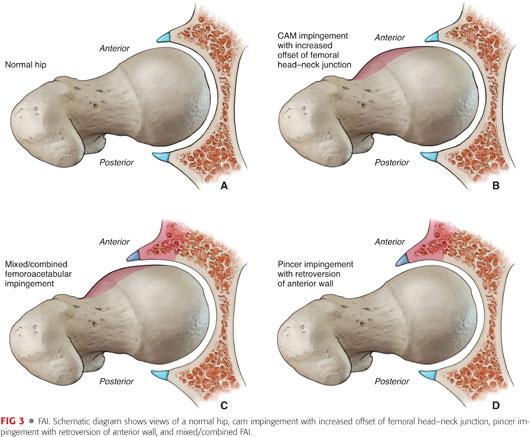
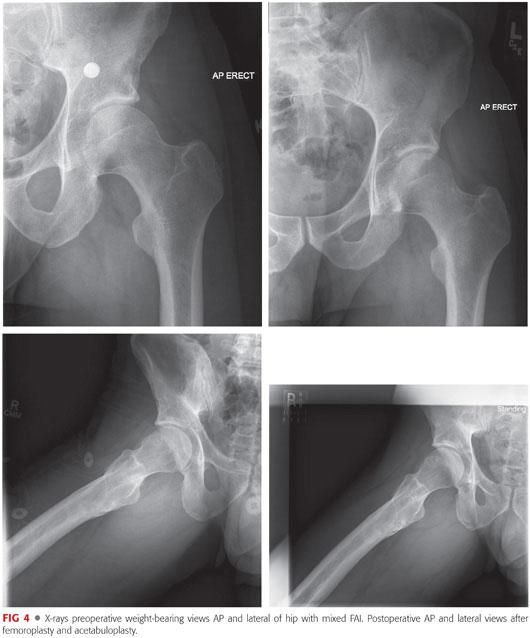
 Femoroacetabular impingement (FAI) refers to a bony over-constraint of the joint either from the femur (cam) or acetabulum (pincer) or both (combined)11 (FIGS 3 and 4)
Femoroacetabular impingement (FAI) refers to a bony over-constraint of the joint either from the femur (cam) or acetabulum (pincer) or both (combined)11 (FIGS 3 and 4)
 Dysplasia refers to a shallow acetabulum, undercoverage of the femoral head, or both12 (FIG 5).
Dysplasia refers to a shallow acetabulum, undercoverage of the femoral head, or both12 (FIG 5).

PATHOGENESIS
 Hip and groin pain in athletic and prearthritic population has a wide variety of etiologies:
Hip and groin pain in athletic and prearthritic population has a wide variety of etiologies:
Labral tear
FAI
Loose bodies
Osteoarthritis
Core muscle injury (also known as sports hernia)
 Labral tear is the most common cause of hip pain and dysfunction in this population.
Labral tear is the most common cause of hip pain and dysfunction in this population.
 Labral tears are usually secondary to FAI or dysplasia or both.
Labral tears are usually secondary to FAI or dysplasia or both.
 If left unchecked, FAI may lead to early development of degenerative joint disease.7
If left unchecked, FAI may lead to early development of degenerative joint disease.7
NATURAL HISTORY
 Labral tear
Labral tear
If left untreated, labral tears can lead to continued pain and dysfunction as well as damage to the adjacent articular cartilage.
 FAI
FAI
If left untreated, many believe that FAI is a precursor to arthritis.
If treated at the appropriate time before irreversible articular cartilage damage occurs, the hip may be preserved.
 Loose bodies
Loose bodies
If left untreated, loose bodies will lead to articular cartilage damage and continued pain and dysfunction.9
 Snapping hip
Snapping hip
In general, snapping hip will cause no damage to the hip joint proper; but if left untreated, it can lead to continued pain and dysfunction.
Internal snapping hip can impinge on the anterior labrum, leading to tears in this area.
PATIENT HISTORY AND PHYSICAL FINDINGS
 A thorough and focused physical examination is essential.
A thorough and focused physical examination is essential.
 Observe gait, manual motor testing, palpation of bony prominences and tendons, range of motion (ROM), and provocative maneuvers for reproducing pain and symptoms.
Observe gait, manual motor testing, palpation of bony prominences and tendons, range of motion (ROM), and provocative maneuvers for reproducing pain and symptoms.
 Perform the examination on the asymptomatic hip first to assess the ROM and stability of the normal hip when possible.
Perform the examination on the asymptomatic hip first to assess the ROM and stability of the normal hip when possible.
IMAGING AND OTHER DIAGNOSTIC STUDIES
 Weight-bearing x-rays (anteroposterior [AP] pelvis, frog lateral, false profile, and Dunn 45-degree views)10
Weight-bearing x-rays (anteroposterior [AP] pelvis, frog lateral, false profile, and Dunn 45-degree views)10
 High resolution magnetic resonance imaging (MRI). Direct MRI arthrogram allows injection of lidocaine to determine if pain is generated from hip.
High resolution magnetic resonance imaging (MRI). Direct MRI arthrogram allows injection of lidocaine to determine if pain is generated from hip.
 Computed tomography (CT) scan allows the best detailed determination of FAI and alignment (dysplasia or version) and allows for detailed preoperative planning for decompression of FAI.10
Computed tomography (CT) scan allows the best detailed determination of FAI and alignment (dysplasia or version) and allows for detailed preoperative planning for decompression of FAI.10
DIFFERENTIAL DIAGNOSIS
 Labral tear
Labral tear
 FAI
FAI
 Loose bodies
Loose bodies
 Synovitis
Synovitis
 Snapping hip
Snapping hip
 Articular cartilage disease
Articular cartilage disease
 Arthritis
Arthritis
NONOPERATIVE MANAGEMENT
 Nonoperative management is always the first step in the treatment of painful hip conditions in the athletic and prearthritic population.
Nonoperative management is always the first step in the treatment of painful hip conditions in the athletic and prearthritic population.
 Activity modification; physical therapy aimed at restoring strength, motion, and balance; and nonsteroidal anti-inflammatory drugs or other medications are the mainstays of nonoperative treatment.11
Activity modification; physical therapy aimed at restoring strength, motion, and balance; and nonsteroidal anti-inflammatory drugs or other medications are the mainstays of nonoperative treatment.11
 The success of treatment depends on the etiology of the hip pain and the patient’s activity level (college or professional athlete or “weekend warrior”) and age.
The success of treatment depends on the etiology of the hip pain and the patient’s activity level (college or professional athlete or “weekend warrior”) and age.
SURGICAL MANAGEMENT
 The vast majority of patients treated with hip arthroscopy have a combination of labral tear and FAI.
The vast majority of patients treated with hip arthroscopy have a combination of labral tear and FAI.
 The goal of surgical treatment is to repair the labrum, treat any articular cartilage injury, and restore the normal biomechanics of the hip joint (ie, decompressing the FAI).
The goal of surgical treatment is to repair the labrum, treat any articular cartilage injury, and restore the normal biomechanics of the hip joint (ie, decompressing the FAI).
Preoperative Planning
 Weight-bearing x-rays (AP pelvis, frog lateral, false profile, and Dunn 45-degree views)
Weight-bearing x-rays (AP pelvis, frog lateral, false profile, and Dunn 45-degree views)
 Be sure to determine that the pain generates from the hip joint and is not referred (lumbar spine or sacroiliac joint) or from muscular pathology (core muscle injury or sports hernia).
Be sure to determine that the pain generates from the hip joint and is not referred (lumbar spine or sacroiliac joint) or from muscular pathology (core muscle injury or sports hernia).
 Be wary of other pathology such as dysplasia, connective tissue disorders, or myofascial pain syndrome.
Be wary of other pathology such as dysplasia, connective tissue disorders, or myofascial pain syndrome.
 Make sure all appropriate equipment and personnel (eg, radiology technician) are available.
Make sure all appropriate equipment and personnel (eg, radiology technician) are available.
Positioning
 Distraction is required for hip arthroscopy as well as fluoroscopic visualization of the joint in all planes.
Distraction is required for hip arthroscopy as well as fluoroscopic visualization of the joint in all planes.
 Place the patient in the supine or lateral position on either a fracture table or commercially available distraction table to allow appropriate distraction of the hip (FIG 6).
Place the patient in the supine or lateral position on either a fracture table or commercially available distraction table to allow appropriate distraction of the hip (FIG 6).

 A well-padded perineal post, preferably with a lateralized post, should be used to allow distraction in the plane of the femoral neck.
A well-padded perineal post, preferably with a lateralized post, should be used to allow distraction in the plane of the femoral neck.
Approach
 Standard portals (FIG 7)
Standard portals (FIG 7)
Anterolateral
Anterior
Midanterior
Posterolateral

 Accessory portals
Accessory portals
Modified anterior
Proximal midanterior
Distal lateral portal
Proximal lateral portal
TECHNIQUES
 Positioning
Positioning
Allow free access around the hip with fluoroscopic access as well (see FIG 6).
Use fluoroscopy to confirm appropriate distraction (TECH FIG 1).
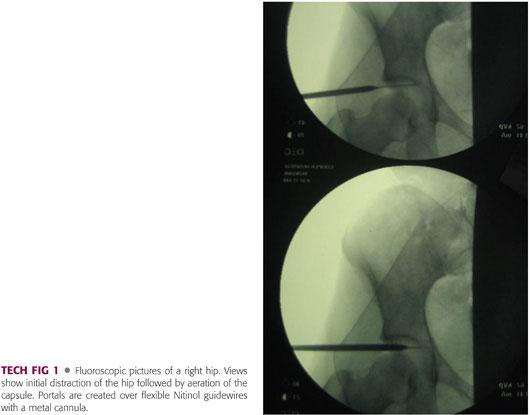
If appropriate distraction cannot be easily obtained, place a needle in the hip under sterile conditions to release the negative intra-articular pressure of the joint and allow distraction.3
 Portals
Portals
Anterolateral (see FIG 7)
Initial portal established under fluoroscopic guidance
Start needle 1 to 2 cm proximal and 1 to 2 cm anterior to the tip of greater trochanter at a sufficient angle to enter the hip joint without damaging the cartilage.3,5
• Removing the obturator from the needle releases the negative intra-articular pressure of the joint and allows increased distraction with the same amount of traction.
• Some surgeons inject the hip with 20 to 40 mL of sterile saline prior to placing the guidewire through the needle.
After placing needle in hip, flexible guidewire is placed for creation of the portal.
Place cannula with gentle steady pressure and be careful not to bend or break the pin.
• Use fluoroscopy as you are creating this portal.
Anterior
Consists of the intersection of sagittal line from anterior superior iliac spine distal and line from tip of greater trochanter3,5
Placed after triangulation when viewing from the anterolateral portal
Most use a modified anterior portal, which is 2 cm more lateral than a standard anterior portal.
After establishing the anterior portal and performing appropriate capsulotomies (see next step), view initial anterolateral portal from anterior portal and complete capsulotomy.
Capsulotomies
After entering the joint, perform capsulotomy with a banana blade or beaver blade under arthroscopic visualization (TECH FIG 2; Video 1).

Capsulotomies are required to allow sufficient movement of instruments in the hip.
Horizontal capsulotomy connecting the anterolateral and midanterior or modified anterior portal is generally required.
• Try to keep a proximal flap of cartilage in case you want to close the horizontal capsulotomy at the end of the case.
“T capsulotomy” can be used for access to peripheral compartment for large cam lesions.
• Must be repaired at the end of the case.
Midanterior
Approximately 45-degree angle between anterolateral and anterior portals and starting distal1,3
Used for anchor placement or for access to peripheral compartment
Used for T capsulotomy when performed
Accessory
See description of portal creation discussed earlier.
The steps are same for establishment of accessory portals.
 Diagnostic Arthroscopy
Diagnostic Arthroscopy
Perform a complete diagnostic arthroscopy of the hip in the same order as a routine arthroscopy (the order of structures inspected does not matter, but it is important to be consistent in your method).
Perform diagnostic arthroscopy of the central compartment and complete repairs before removing traction and going on to the peripheral compartment.
Inspect all structures in the central compartment with traction and peripheral compartment after traction released (list is not complete or comprehensive):
Central compartment (TECH FIG 3A)
• Labrum, articular cartilage acetabulum, ligamentum teres, articular cartilage femoral head, and loose bodies

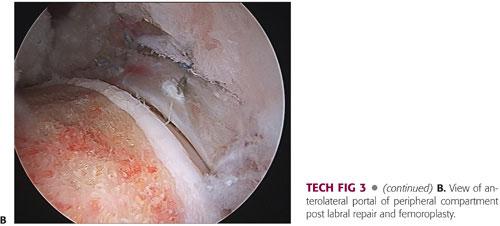
Peripheral compartment (TECH FIG 3B)
• Medial synovial fold, medial head-neck, middle head-neck, lateral head-neck, labrum, lateral synovial fold, lateral gutter, and medial gutter
Other areas are listed below but not covered in detail in this chapter:
Peritrochanteric space
Subgluteal space
Iliopsoas tendon
 Labral Repair or Débridement (Video 2)
Labral Repair or Débridement (Video 2)
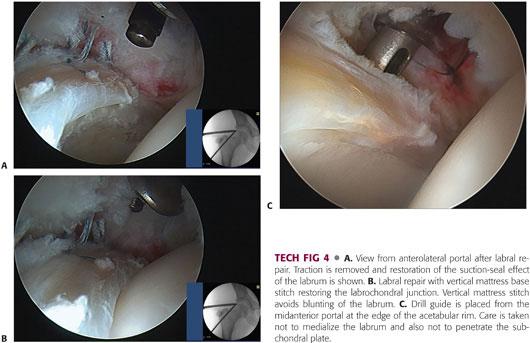
We prefer to repair the labrum to reestablish the suction-seal effect (TECH FIG 4A).
If débridement is required, use a combination of shaver and radiofrequency device to remove pathologic tissue while preserving as much healthy and stable tissue as possible.
Remove loose bodies, chondroplasty, and microfracture as indicated.
Repair
Suture anchors or knotless device (according to surgeon preference)
The goal is to repair labrum to the edge of the articular margin of the acetabulum to restore the anatomy and the suction-seal effect of the labrum (TECH FIG 4A).
Vertical mattress or base stitch should be used when possible (tissue quality and size) because it gives the best restoration of the labral anatomy8 (TECH FIG 4B).
Elevate and mobilize labrum off acetabulum and try to preserve the labrocartilaginous junction.
Perform acetabuloplasty/rim trimming when indicated or decorticate acetabular rim to provide a healing surface for labral repair.8
Place anchors through the midanterior portal at a 30- to 45-degree angle relative to the edge of the acetabulum (TECH FIG 4C).
Place anchors from anterior (medial) to anterolateral while viewing from anterolateral portal.
Pass a single arm of suture under labrum at labro-cartilagenous junction and retrieve the same suture through the labrum to create a vertical mattress stitch.
• You may do a single pass around labrum in a “wrap around” fashion as well.
Pass-retrieve-tie, move to next anchor, and repeat.
Keep knots off articular surface (TECH FIG 4B; Video 3).
 Acetabuloplasty/Rim Trimming
Acetabuloplasty/Rim Trimming
Typically done as noted earlier during labral repair while under traction
May also perform acetabuloplasty without labral detachment or repair
Follow preoperative plan regarding location and amount of acetabulum to trim.
Round burr (side cutting) or flat-top burr (end and side cutting) (TECH FIG 5)
Use combination of arthroscopic elevators, rasps, shaver, and a radiofrequency device to clear acetabular rim of periosteal coverage.
Use fluoroscopy to help guide resection (it is critical to obtain true AP of hip to allow appropriate resection).

Can take down to edge of articular cartilage damage in small defects
Preserve the labrum while performing acetabuloplasty.
Exercise caution with resection to prevent overresection and subsequent iatrogenic instability.
 Femoroplasty
Femoroplasty
Careful preoperative planning for location and amount of femoral resection for femoroplasty (Video 4)
Allows access to peripheral compartment after completion of work in the central compartment and removal of traction
Initially assess peripheral compartment through the capsulotomies.
Flex hip to approximately 45 degrees and slight abduction to relax the capsule and allow access to peripheral compartment and head–neck junction.4
Can access further lateral with internal rotation of the leg
Begin with assessment and localizing the cam lesion and confirming access arthroscopically (TECH FIG 6A).
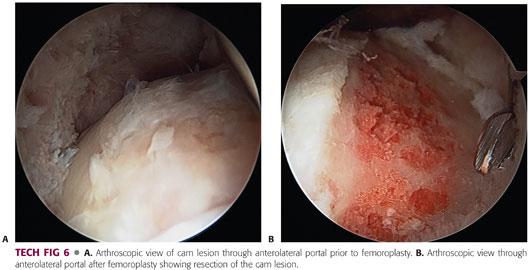
Begin resection proximally with round burr slightly into the articular margin (usually in line with physeal scar but not always) (TECH FIG 6B).
Work from anterior to anterolateral to lateral and proximal to distal, setting a proximal template and contouring distally in a gentle progression to the femoral neck.4
Switch between anterolateral, midanterior, and anterior portals for viewing and working, depending on the area to be resected.
Perform a dynamic examination at the end of femoroplasty, putting the hip in the impingement position to confirm resolution of the bony conflict.
May need to perform a T capsulotomy to access large lesions or distal and lateral
Close the “T” with side-to-side sutures at end of femoroplasty (Video 5).
 Loose Bodies
Loose Bodies
Loose bodies that form in the hip can be located in the central and peripheral compartments.
Removal of all loose bodies from central compartment typically requires use of the posterolateral portal.9
Thorough examination of peripheral compartment is needed to remove all loose bodies.
 Microfracture
Microfracture
Typically used for acetabular cartilaginous defects
Use curettes and a shaver to stabilize the edges of cartilage and remove calcified layers of cartilage in area of microfracture.
Various angle picks are available.
However, you must be careful with the angle to avoid cutting off the acetabulum.
 Iliopsoas Snapping (Internal Coxa Saltans)
Iliopsoas Snapping (Internal Coxa Saltans)
The iliopsoas tendon may snap or pop over the femoral head or iliopectineal line, causing pain.
Tendon release can be done transcapsular at the level of the joint in the central compartment or extracapsular at the lesser trochanter.
A radiofrequency device or beaver blade is used for release.
PEARLS AND PITFALLS | |
Confirm appropriate joint distraction prior to prep and drape and then release; replace traction after prep and drape. This will allow you to minimize traction time. |
|
After placing initial needle into hip for anterolateral portal, remove under fluoroscopy and replace to ensure that it does not penetrate the labrum. |
|
Use fluoroscopy judiciously as needed, especially early in the learning curve, until you are comfortable with portal and instrument placement. |
|
When placing anchors, get close to the edge of acetabulum without penetrating subchondral bone to prevent medialization of the labrum. Keep angle of drill guide at 30–45 degrees, relative to the acetabulum. |
|
Expose rim fully to allow appropriate anchor placement on edge of rim. |
|
POSTOPERATIVE CARE
 Outpatient procedure and discharge with crutches and a hip brace
Outpatient procedure and discharge with crutches and a hip brace
 Continuous passive motion is to be performed at home during the first week to 10 days.
Continuous passive motion is to be performed at home during the first week to 10 days.
 For labral débridement with or without FAI, crutches for 1 to 2 weeks.
For labral débridement with or without FAI, crutches for 1 to 2 weeks.
 For labral repair, crutches and protected weight bearing for 2 to 4 weeks.
For labral repair, crutches and protected weight bearing for 2 to 4 weeks.
 Begin physical therapy 1 week after surgery.
Begin physical therapy 1 week after surgery.
 Advance to formal physical therapy and home programs throughout the recovery period.
Advance to formal physical therapy and home programs throughout the recovery period.
OUTCOMES
 Multiple studies have reported good to excellent outcomes for hip arthroscopy used to treat FAI.
Multiple studies have reported good to excellent outcomes for hip arthroscopy used to treat FAI.
 A systematic review showed that 10 of 12 studies reported good to excellent outcomes in 75% or more of patients treated with hip arthroscopy.
A systematic review showed that 10 of 12 studies reported good to excellent outcomes in 75% or more of patients treated with hip arthroscopy.
 One of the keys to successful outcome is the stage of arthritis at the index surgery.
One of the keys to successful outcome is the stage of arthritis at the index surgery.
COMPLICATIONS
 Complication rates reported in the literature are low.
Complication rates reported in the literature are low.
 Iatrogenic
Iatrogenic
Cartilage damage from cannulas or instrumentation
Damage from misplacement of anchors
Iatrogenic instability (overresection of acetabulum or capsular insufficiency or both)
 Neurologic
Neurologic
Positioning: perineal numbness/pudendal nerve
Traction: sciatic nerve
Portals: lateral femoral cutaneous nerve
Regional pain syndrome
 Procedure
Procedure
Iatrogenic injury
Failure of fixation
Medialization of labrum with repair
 Postoperative
Postoperative
Deep vein thrombosis/blood clot
Fracture: overzealous resection of femoral neck for cam
 Other
Other
Avascular necrosis
Stiffness
REFERENCES
1. Alwattar BJ, Bharam S. Hip arthroscopy portals. Op Tech Sports Med 2011:19(2):74–80.
2. Botser IB, Smith TW, Naser R, et al. Open surgical dislocation vs. arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy 2011;27:270–278.
3. Byrd JW. Hip arthroscopy: applications and technique. J Am Acad Orthop Surg 2006:14(7):433–444.
4. Byrd JW, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Ortho Relat Res 2009;3:739–746.
5. Byrd JW, Pappas JN, Pedley MJ. Hip arthroscopy: an anatomic study of portal placement and relationship to the extra-articular structures. Arthroscopy 1995;12:603–612.
6. Fergunson SJ, Bryant JT, Ganz R, et al. The acetabular labrum seal: a poroelastic finite element model. Clin Biomech 2000;15:463–468.
7. Ito K, Leunig M, Keller I, et al. Impingement-induced damage of the acetabular labrum: a possible initiator of hip arthrosis. Eighth Annual Meeting, European Orthopaedic Research Society, 1998:55.
8. Kelly BT, Weiland DE, Schenker ML, et al. Arthroscopic labral repair in the hip: Surgical technique and review of the literature. Arthroscopy 2005;21:1496–1504.
9. Krebs VE. The role of hip arthroscopy in the treatment of synovial disorders and loose bodies. Clin Ortho Relat Res 2003;406:48–59.
10. Nepple JJ, Prather H, Trousdale RT, et al. Diagnostic imaging of femoroacetabular impingement. J Am Acad Orthop Surg 2013;21:S16–S19.
11. Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg 2007;15:561–570.
12. Sanchez-Sotolo J, Trousdale RT, Berry DJ, et al. Surgical treatment of developmental dysplasia of the hip in adults: I. Nonarthroplasty options. J Am Acad Orthop Surg 2002;10:321–333.
< div class='tao-gold-member'>








