Arthroscopy
Michael S. Bednar
Charles A. Goldfarb
General Principles
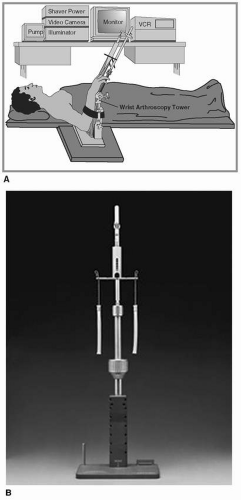
I. Setup
Arthroscopy for the hand and wrist is performed with the patient in supine position and the extremity on a stable arm table. A nonsterile tourniquet is placed and inflated after exsanguination. A traction tower is utilized to allow the elbow and forearm to be stabilized while the wrist or finger joints are distracted using weight applied through finger-traps. For a wrist arthroscopy, either 2 or 4 finger-traps are applied to the digits; for a thumb or finger arthroscopy, a single finger-trap is applied. The arthroscopy tower is placed at the foot of the operating table for easiest viewing of the monitor. If a mini fluoroscopy machine is utilized, it can be brought into the operative field from the end of the arm table. Complications of the traction tower include over distraction of a joint (limit traction to 10 lb) and heat or pressure injury from the metal traction tower (assure tower is cool and pad extremity).
II. Equipment and General Guidelines (Fig. 5.1)
Wrist arthroscopy is performed using a 2.4 or 2.7 mm, 30-degree arthroscope.
Due to the close proximity of the cutaneous nerves, portals are created with a skin incision only. A small curved clamp is used to dissect through the tissue to the capsule of the joint
A blunt trochar in the arthroscope cannula is used to establish the viewing portal.
A shaver is utilized through the working portal. The shaver is typically 2.9 mm in size, and the aggressiveness is dependent on the type of blade. Suction tubing is attached to the shaver to remove the debris created in the shaving process.
Lactated Ringer fluid is used during arthroscopy. The fluid flows into the joint through gravity (i.e., fluid pumps are not typically utilized).
A probe is used as a tool to evaluate the soft tissues of the joint including the ligaments and the triangular fibrocartilage complex (TFCC). For arthroscopy of the hand, these probes are also useful for reducing displaced ligaments. The probes typically have a 2 to 3 mm curved tip for measurement and manipulation purposes.
Toothed graspers are helpful for the removal of debris or loose bodies.
Suction punches allow biting of tissue and removal through suction tubing.
A 2.9 mm burr may be utilized for bone removal such as a distal ulna resection or partial trapeziectomy.
A TFCC repair kit allows a minimally invasive technique for TFCC repair with curved needles allowing the passage of suture and a snare to retrieve the suture.
Tuohy needles (blunt tip anesthesia needles) may also be used to repair TFCC tears, especially ulnar-sided tears.
A suction trap may be placed in the suction tubing to “trap” shaved particles, synovitis, and debris; the collected tissue can then be sent to the lab for analysis.
Small joint radiofrequency probes may be utilized for tissue removal or for heat shrinkage applications such as scapholunate (SL) instability or carpometacarpal (CMC) joint instability.
Hand Arthroscopy
I. Introduction
Arthroscopy of the hand is gaining popularity as it allows a minimally invasive technique for evaluation and treatment of selected joint-based problems. The joints most amenable to arthroscopy are the thumb CMC joint, the thumb metacarpophalangeal (MCP) joint, and the finger MCP joints. The principles of and setup for a hand arthroscopy follow the guidelines summarized earlier in this chapter with a few caveats. First, a 2.4 or 2.7 mm arthroscope will provide excellent visualization but, in some patients, a 1.9 mm arthroscope may be more appropriate as the smaller size allows for easier mobility inside the joint (with a downside of increased fragility of the scope). And second, while thermal devices may be utilized in the hand, care must be utilized given the close proximity of the cutaneous nerves and the smaller fluid volume of the joints (the fluid helps dissipate the heat).
II. Thumb CMC Joint Arthritis
The thumb CMC joint is the second most commonly arthritic joint in the hand and postmenopausal women are the most frequently affected. Patients present with localized pain and decreased function. When nonoperative treatment fails, surgical intervention can be very helpful in alleviating symptoms. One surgical option is the arthroscopic treatment of CMC arthritis.
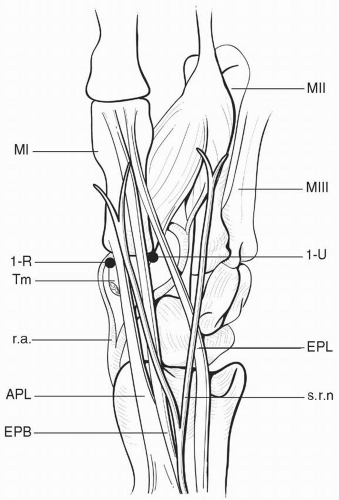
Setup/portals (Fig. 5.2)
A high brachial tourniquet is used.
The patient is in supine position on the operating table with the arm on a stable arm board.
The arm is exsanguinated, and the thumb is suspended in a traction tower through a finger-trap with 8 to 10 lb of traction applied.
A needle is used to localize the joint (and insufflate with saline). A minifluoroscopy machine may be used to confirm needle placement.
The 1U portal is established just ulnar to the extensor pollicis brevis (EPB) tendon by incising the skin only and bluntly dissecting to and through the joint capsule.
The small joint arthroscope is placed into the CMC joint.
Needle localization of the 1R portal (radial to abductor pollicis longus [APL]) or the thenar portal (more volar and through thenar muscle bulk) is performed to help establish a working portal.
Alternating the viewing and working portals will facilitate complete joint evaluation and treatment.
Procedure
Arthroscopy allows a minimally invasive approach, and, when compared to open procedures can offer equal effectiveness.
Arthroscopy allows joint evaluation, debridement (including loose body removal), and synovectomy.
In patients with early stage disease, joint debridement may be combined with an extra articular procedure such as a dorsal closing-wedge osteotomy of the metacarpal to change the loading pattern of the joint.
In patients with notable loss of cartilage, a partial trapeziectomy (3 mm of distal trapezium) utilizing a 2.9 mm burr may be performed. A distraction pinning of the joint or a tendon interposition (most commonly the palmaris longus tendon) can be performed.
Complications of this approach include the following:
Cutaneous nerve irritation from portal placement (the s-2 or s-3 branches of the superficial branch of the radial nerve)
Injury to the radial artery (rare given it is several millimeters more proximal at the scaphotrapezial trapezoid joint)
Interpositional graft extrusion (rare given small capsular opening for arthroscopy)
Failure to relieve pain
One benefit of the arthroscopic approach is that the larger, open procedure may be performed if the minimally invasive procedure fails.
III. Thumb MP Joint Ulnar Collateral Ligament Injury
An injury to the ulnar collateral ligament (UCL) of the thumb MCP joint is typically managed with cast or splint immobilization for 4 to 6 weeks. However, in patients with a complete ligament tear with retraction of the ligament superficial to the adductor aponeurosis (Stener lesion), healing of the ligament to bone cannot occur. Those patients with a Stener lesion typically have marked MCP joint instability, and a risk of chronic instability at the thumb MCP joint if not addressed. Open reduction of the UCL and reattachment to the base of the proximal phalanx (often with suture anchor) is a reliable procedure.
An alternative treatment is an arthroscopic joint assessment and manipulation of the UCL with a probe to allow it to assume its natural position deep to the adductor aponeurosis. If the tendon can be restored to its normal position adjacent to the base of the proximal phalanx, healing should occur reliably with immobilization alone. This avoids the need for an open incision and hardware placement. The setup is the same as for CMC arthroscopy. The portals are established on the dorsal ulnar and radial aspect of the extensor mechanism.
IV. Idiopathic MCP Joint Synovitis
Rarely, one or more MCP joints may be affected with painful synovitis. Laboratory evaluation including inflammatory labs may also be helpful in establishing a diagnosis. Typically anti-inflammatory medications or a steroid injection will resolve the inflammation. However, if these evaluations and treatments are unsuccessful in confirming a diagnosis and improving symptoms, arthroscopy evaluation, debridement, and biopsy may be helpful. The benefit of the arthroscopic approach is the avoidance of an open incision with detachment (and repair) of the sagittal band. Arthroscopy allows a biopsy of the tissue and a complete synovectomy with a 2.9 mm shaver.
Wrist Arthroscopy
I. Introduction
Diagnostic wrist arthroscopy provides a visual inspection of the articular surfaces, triangular fibrocartilage complex, intra-articular portions of the intercarpal and intracarpal ligaments, and wrist capsule of the radiocarpal and midcarpal joints.
Therapeutic wrist arthroscopy is used for
Synovial, ligamentous, cartilaginous, or loose body debridement
Arthroscopic assisted repairs of peripherial TFCC tears
Treatment of ulnocarpal impaction syndrome, including lunotriquetral (LT) ligament debridement, central TFCC debridement, and distal ulnar resection
Ganglion excision
Reduction of intra-articular fractures
II. Diagnostic Wrist Arthroscopy
Portals (Fig. 5.3)
Radiocarpal
1-2 portal is located in the anatomic snuffbox between the EPB and extensor pollicis longus (EPL) tendon and is within 3 mm of the radial artery and dorsal sensory branch of the radial nerve. This can be used as a working portal for arthroscopic radial styloidectomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree