and Ziv Gil2
(1)
Division of Otolaryngology Head and Neck Surgery and Maxillofacial Surgery, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel
(2)
The Head and Neck Center Department of Otolaryngology Head and Neck Surgery, Rambam Healthcare Campus, Haifa, Israel
Keywords
Retromaxillary spaceMasticatory spaceRobotic surgeryTranscervical endoscopic approach7.1 Introduction
The parapharyngeal space (PPS) is a potential space between the skull base above and the hyoid bone below. It has an inverted teepee shape. Its borders include the nasopharynx and oropharynx medially, the masticator space anterolaterally, the deep lobe of the parotid gland posterolaterally, and the retropharyngeal space posteromedially (Fig. 7.1). The PPS can harbor tumors and infectious processes, but both infectious processes and neoplasms are rare. Tumors can originate in the PPS or can invade the space from neighboring areas. Pleomorphic adenoma is the most common benign tumor of the PPS, followed by schwannomas and paragangliomas. Malignant tumors arising in the PPS can invade the intracranial compartment, maxilla, mandible, temporomandibular joint, orbit, or skin. Hematogenous or lymphatic spread can also occur, as well as perineural invasion along cranial nerves. Perineural invasion is common in adenoid cystic carcinoma and is the pathway to the intracranial space, so imaging studies should be directed toward the foramen ovale, foramen rotundum, cavernous sinus, orbital apex, trigeminal ganglion, and dura. In addition, the radiological evaluation of any patient with suspected malignancy must include the neck, to evaluate for lymph node metastasis. Symptoms include change in voice, trismus, mass in the upper neck, cranial nerve deficits, serous otitis media (due to Eustachian tube obstruction), and obstructive sleep apnea. Standard surgical approaches to the PPS include the transcervical approach, the transparotid-transcervical approach, the transmandibular approach, the endoscopic transnasal approach, the transoral robotic surgery, and the infratemporal fossa approach. The anatomical extent of the tumor, its histologic type (benign or malignant), and the patient’s medical history (previous surgeries or radiation treatment) determine the surgical approach. This chapter describes the common surgical approaches to the PPS.
Fig. 7.1
The borders of the parapharyngeal space (PPS) include the nasopharynx and oropharynx medially, the masticator space anterolaterally, the deep lobe of the parotid gland posterolaterally, and the retropharyngeal space posteromedially
7.2 Preoperative Evaluation and Anesthesia
7.2.1 Imaging Studies
Imaging should always be used prior to surgery. A contrast CT scan and a basic MRI study with fat suppression should be used for preoperative evaluation and surgical planning. Visualization of a vascular flow void on an MRI study is usually sufficient for the diagnosis of a vascular tumor such as a paraganglioma, but MR angiography (MRA) may be added for a more precise diagnosis. Malignant tumors usually are seen as a soft tissue mass invading intracranial or adjacent spaces, accompanied by bone destruction. The CT scan may show mild enhancement, and T1-weighted MRI may demonstrate strong postcontrast enhancement. Application of a fat-suppression technique, such as short tau inversion recovery (STIR) and frequency-selected fat suppression, eliminates strong signals from adipose tissue. In addition, the definition of normal anatomical structures is significantly improved, enhancing lesions become clearer, and the margins of a lesion are better defined when fat suppression is used in combination with contrast enhancement. If a malignant tumor is suspected, radiological staging of the patient is completed by using a hybrid of positron emission tomography (PET) and CT (PET/CT) to assess the presence of regional and distant metastases.
7.2.2 Tissue Diagnosis
Tissue diagnosis should be an integral part of preoperative evaluation. Although radiological imaging could provide indications regarding the type of neoplasm, tissue diagnosis is sensitive to differences between benign and malignant lesions. Fine needle aspiration (FNA) biopsy can be performed via ultrasound, but frequently CT-guided FNA, which is technically challenging, is required. To avoid potential bleeding, radiological imaging should precede FNA if a vascular tumor is suspected. Some exceptions to preoperative biopsy include juvenile angiofibroma and paragangliomas.
7.3 Surgical Technique
Our arsenal includes various surgical approaches for the resection of PPS tumors. Table 7.1 shows the various indications for each approach described below. Figure 7.2 depicts a few of the head and neck incisions that are performed in each of these approaches.
Table 7.1
The various approaches to the parapharyngeal space and their indications
Radiological description | Likely diagnosis | Surgical approach |
|---|---|---|
Prevascular tumors | Benign salivary gland tumor | Transcervical, TORS, transcervical endoscopic |
Postvascular tumors | Schwannoma, paraganglioma | Transcervical |
Deep-lobe parotid tumors with PPS extension | Benign salivary gland tumor | Transcervical-transparotid |
Large malignant tumors with skull base involvement | Malignant salivary gland tumor, sarcoma | Transmandibular |
Large tumors with infratemporal fossa involvement | Schwannoma, paraganglioma, salivary gland tumor, sarcoma | Transcervical-infratemporal fossa |
Fig. 7.2
Some of the head and neckincisions used in various approaches tothe parapharyngeal space
7.3.1 The Transcervical Approach for Resection of PPS Tumor
The transcervical approach is the most common method for removal of benign tumors that originate in the prestyloid or poststyloid compartment of the PPS. The common tumors in this area are pleomorphic adenoma and schwannoma. Figure 7.3 shows a classic appearance of PPS pleomorphic adenoma as revealed in axial CT and MRI. If a transcervical approach is planned, the surgeon must investigate whether the tumor extends to the PPS from the parotid gland. If it does, or in case of a deep-lobe parotid tumor, a transparotid approach is required to protect the facial nerve.
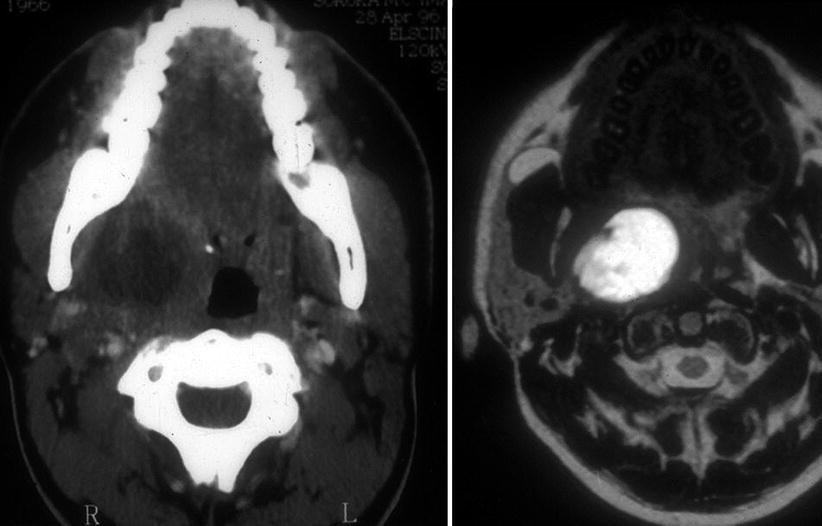
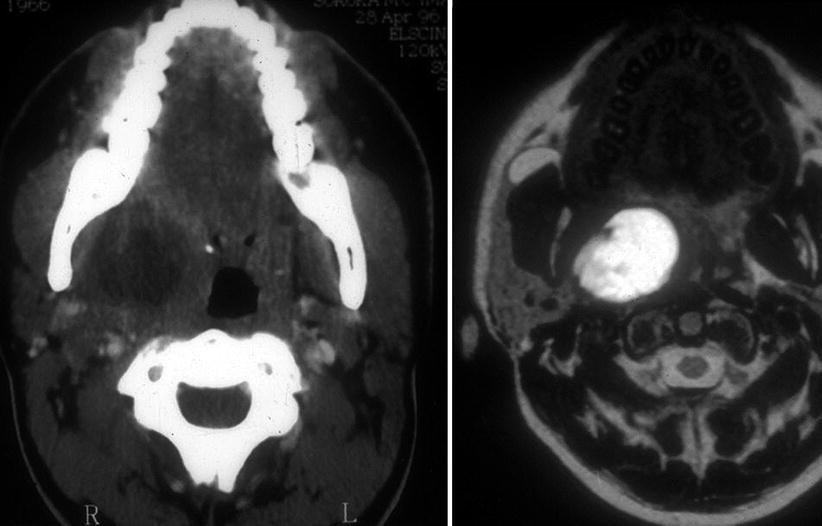
Fig. 7.3
Pleomorphic adenoma in the PPS, as revealed in axial CT and MRI
The patient is placed on the operating room table in a supine position. The head is stabilized with a soft donut holder and the whole operating table is then elevated in a head-up angle in order to minimize bleeding. The surgical incision is through a skin crease located two to three fingers below the mandible, to prevent injury to the marginal mandibular branch of the facial nerve (Fig. 7.4). Marking of the incision is preferably performed with the neck slightly flexed in order to identify the lines of relaxed skin tension. After incision marking, a roll is placed under the shoulders to hyperextend the neck, and the head is rotated toward the contralateral side.


Fig. 7.4
For a transcervical approach, the surgical incision is through a skin crease located two to three fingers below the mandible
After the prepping and dressing, the skin is incised with a #15 blade and subsequent dissection of the subcutaneous tissue and the platysma is carried out with an electrocautery device at the lowest effective setting. Subplatysmal flaps are elevated superiorly. To avoid injuring the marginal mandibular branch of the facial nerve, the flap is elevated at the level of the platysma, leaving the superficial layer of the deep cervical fascia on the submandibular gland. In this case, the nerve runs within the fascia superior to the submandibular gland.
The dissection now continues along the superficial layer of the deep cervical fascia that unwrap the sternocleidomastoid muscle. We usually start this dissection by placing hemostats on the fascia at the anterior border of the muscle, retracting the tissue medially. The dissection is started at the anterior border of the muscle, along its superior two thirds. As the dissection is continued with electrocautery, small vessels interconnecting the superficial and deep borders of the muscle are cauterized with bipolar electrocautery or LigaSure™ technology (Covidien; Boulder, CO). As the deep aspect of the muscle is approached, care is taken to avoid injury to the spinal accessory nerve, which enters the muscle at the junction of its upper and middle third and lateral to its medial border. After exposing the spinal accessory nerve, the posterior belly of the digastric muscle is identified. The next step is identifying the internal jugular vein and the common carotid artery and its branches. The vagus nerve, which runs along the carotid artery, is identified and preserved. As the dissection is continued from below toward the exposed digastric muscle, the hypoglossal nerve should be identified. This nerve lies inferior to the posterior belly of the digastric muscle, anterior to the distal portion of the internal jugular vein, and superficial to the internal and external branches of the carotid artery. The anterior branches of the ansa hypoglossi may also be used here to trace the nerve. The submandibular gland is identified and freed from the surrounding fascia (Fig. 7.5). The facial artery and vein may be divided, allowing anterior retraction of the gland. If the tumor is large, the gland may be removed, exposing the caudal margin of the PPS.


Fig. 7.5
The submandibular gland is identified and freed from the surrounding fascia
The tumor is now identified and its association with the cranial nerves should be explored. Next, the posterior belly of the digastric muscle is divided and the mylohyoid muscle is retracted anteriorly (Fig. 7.6). The stylohyoid muscle and stylomandibular ligament also may be divided to allow a wide approach to the PPS from below. This maneuver also may prevent accidental injury to the internal jugular vein at the jugular foramen. (Injury in this area may be difficult to control, and hemostasis may require tying of the vein.) The tumor is now separated from the surrounding tissue. The surgeon is advised to use meticulous dissection with a thin hemostat in order to prevent injury to the great vessels and cranial nerves. After the tumor is completely separated from its surrounding tissue, the surgery continues with a finger dissection. The tumor is gently mobilized from its surrounding tissue in a blind fashion, and small bundles are divided with the use of Hudson or Kelly clamps (Fig. 7.7). The tumor is delivered caudally (Fig. 7.8). Care is taken not to press on the tumor capsule, in order to prevent spillage (Fig. 7.9).
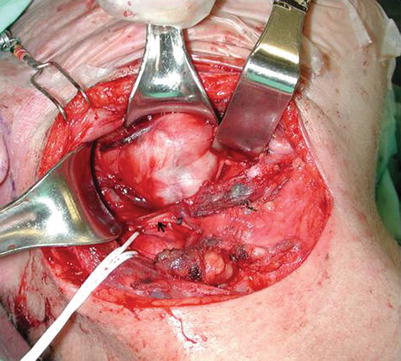
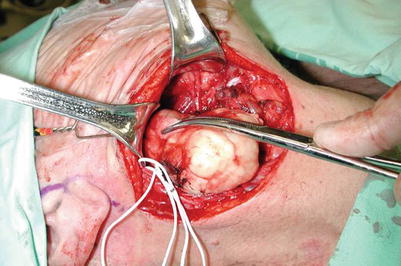
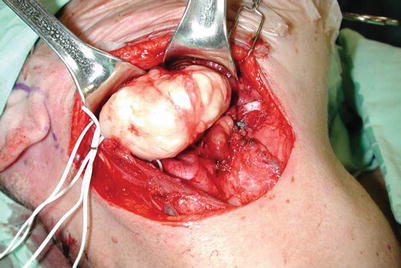
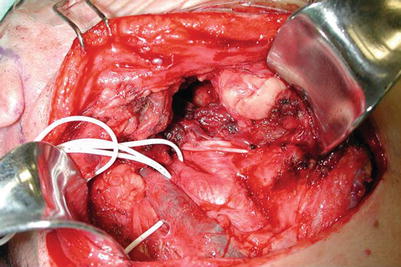
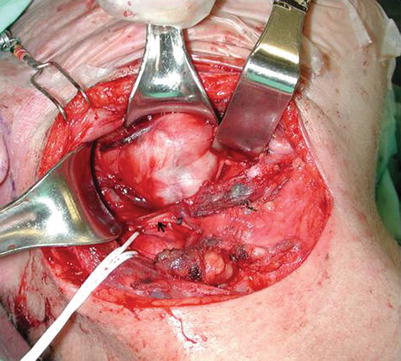
Fig. 7.6
The posterior belly of the digastric muscle is divided and the mylohyoid muscle is retracted anteriorly
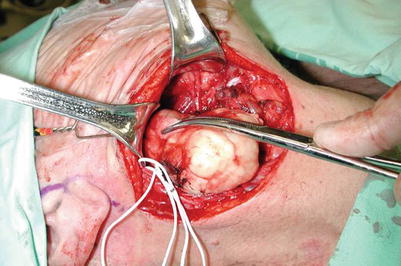
Fig. 7.7
The tumor is gently mobilized from its surrounding tissue in a blind fashion, and small bundles are divided with the use of Hudson or Kelly clamps
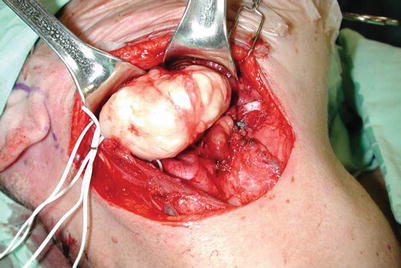
Fig. 7.8
The tumor is delivered caudally
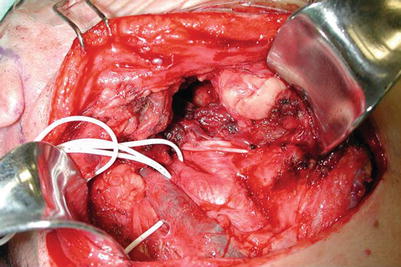
Fig. 7.9
In delivering the tumor, care is taken not to press on the tumor capsule, in order to prevent spillage
The wound is copiously irrigated and is inspected; hemostasis is performed as indicated. For adequate hemostasis, a blood pressure above 120/80 should be confirmed prior to closure. A Jackson-Pratt number 7 drain is left at the surgical bed, the platysma is sutured with absorbable sutures, and the skin is closed with 5.0 nylon sutures.
7.3.2 The Transparotid Approach for Resection of PPS Tumor
This approach is used for deep-lobe parotid tumors that extend to the PPS. These tumors typically appear as a dumbbell-shaped lesion on CT or MRI. Because the tumor originates from the parotid gland, exposure and dissection from the facial nerve are necessary. Surgery is usually performed without muscle relaxants and with nerve monitoring of the buccal and zygomatic branches of the facial nerve. Facial nerve monitoring electrodes are inserted prior to draping, to allow measurement of the electrophysiological activity of the orbicularis oculi and orbicularis oris muscles. To allow monitoring of the marginal mandibular and the buccal branches, the electrode should be placed at the commissure, to include the lower and upper segments of the orbicularis oris muscle.
The surgical access is planned through a modified Blair incision (Fig. 7.10). The incision normally extends from the tragus, encircles the lobule, and then drops down posterior to the helix, along the nuchal hair line. In young patients, the incision is performed on the free edge of the tragus, but in elderly persons it is better concealed along a preauricular vertical skin crest. For large tumors, the incision can be extended 2–3 cm below the ramus of the mandible, along a transverse skin crest in the lower neck. If neck dissection is indicated, the incision is extended medially up to the level of the cricoid cartilage. A sterile ophthalmic prep solution (Betadine®) containing 5 % povidone-iodine (0.5 % available iodine) is used for prepping of the periocular region (lids, brow, and cheek). A transparent adhesive drape sheath (Steri-Drape™) is placed on the face to allow intraoperative monitoring of facial movements during surgery. For safe and accurate identification of the facial nerve, the operation should be performed while minimizing bleeding and monitoring movements of the facial muscle.