There is an increased demand for safer procedure-based therapeutic options for many diagnoses among patients with skin of color, due to differences in melanocyte distribution, melanocyte activity, and skin reactivity.
Microneedling and platelet-rich plasma (PRP) have been shown to be safe procedures on all ethnic skin types, with only a predisposition of keloid formation or active infections as relative contraindications.
Microneedling may be used safely and effectively for facial rejuvenation, acne scarring, melasma, periorbital melanosis, and striae. Enhanced absorption of topical therapies may also occur after microneedling.
To avoid adverse events like dyspigmentation and scarring after microneedling in skin of color, the authors recommend diligent UV light protection, the proper length of microneedles that correspond to the thickness/thinness of the targeted location on the face, and the avoidance of excessive pressure over bony areas of the face.
Combination treatment of microneedling with PRP shows exponential enhancement and improvement of many conditions, including the stimulation of anti-inflammatory and antifibrotic cytokines.
8.1 Introduction
In recent years, microneedling and platelet-rich plasma (PRP) either in isolation or combination have become increasingly popular treatment modalities for acne scarring, striae, scars, pigmentary disorders, hair loss, and skin rejuvenation. Particularly in skin of color, microneedling may offer a potentially safer treatment option compared to ablative and non-ablative lasers for skin resurfacing where postinflammatory hyperpigmentation and scarring are undesired potential side effects. In this chapter, we review current literature and offer treatment and safety recommendations for these modalities in skin of color.
8.2 Basic Science
8.2.1 Objective Differences in Different Ethnic Skin Types
According to the United States Census Bureau, America’s diversity continues to increase with all racial and ethnic minority groups growing at faster rates than whites. With this increase in multicultural diversity in the U.S., idealistic ethnocentric variability has not only changed the standards of beauty but also the number and types of cosmetic procedures performed on skin of color patients. As such, research continues to expand our understanding of the intrinsic differences in ethnic skin, the unique properties of its structure and function, including the amount of melanin, activity of melanocytes, variation in skin thickness, as well as fibroblastic and mast cell features, differences in pH levels, variable blood vessel reactivity, and a host of other factors currently being researched ( ▶ Table 8.1). 1
Evidence supports | Insufficient evidencea for | Inconclusive |
| Racial differences in:
| Racial differences in:
|
| ||
| ||
| ||
| ||
Abbreviations: PLS, parallel-linear striations; YEWL, transepidermal water loss. Source: Adapted from Wesley NO, Maibach HI. Racial (ethnic) differences in skin properties: the objective data. Am J Clin Dermatol 2003;4:843–880. aScan elastic recovery/extensibility, skin microflora, and poor size or labeled as “insufficient evidence for” racial differences rather than inconclusive because only two studies are fewer examine the variables. bSugiyana-Nakagiri Y, Sugata K, Hachiya A, et al. Ethnic differences in the structural properties of facial skin. J Dermatol Sci 2009;53:135–139. | ||
8.2.2 Melanocyte Distribution and its Relationship to Skin of Color
By far, the melanin content accounts for one of the most significant differences between persons with lighter versus darker skin types. This characteristic reflects both the quantitative and qualitative activity of the melanocytes. Within the cytoplasm of melanocytes are melanosomes that serve as the site for melanin production. Melanosomes are transferred to surrounding keratinocytes, thereby giving patients their characteristic “skin color.” The size, number, and accumulation of melanosomes within each keratinocyte further contribute to the differences in complexion. Larger melanosomes with abundant melanin are singly dispersed and degraded at slower rates, contributing to darker skin seen among patients characterized as Fitzpatrick skin types (FST) III to VI. In contrast, smaller collections of melanosomes with decreased amounts of melanin contribute to lighter skin colors among patients characterized as FST I to II. 1 Additionally, melanosomes are dispersed throughout all of the layers of the epidermis in skin of color, whereas they are confined to the basal and lower malphigian layer of the epidermis in Caucasian skin. 2
Findings from molecular genetics also support variations in ethnic skin types with defined pigmentation genes such as tyrosinase-related protein family members. Tyrosinase-related protein 1 increases tyrosinase activity and subsequently, leads to an increase in both melanin synthesis and melanosome size. Together, the aforementioned components help to explain the differences in response to ultraviolet (UV) light among different ethnicities. Likewise, melanocyte-stimulating hormone triggers the production of DNA repair proteins, which aid in the protection of darker skinned ethnicities when exposed to damaging UV sources. Moreover, the melanocortin-1-receptor aids in the type of melanin produced by melanocytes (pheomelanin, which is red–yellow in color, and eumelanin, which is brown–black in color). 1
8.2.3 Differences in Skin Thickness in Skin of Color
Newer studies have proposed that increased numbers of cornified cell layers and lipid content help explain increased skin thickness in darker skin types. When compared to that of whites’, darker skin types have increased numbers and larger sizes of fibroblasts, suggestive of active biosynthesis and turnover of collagen. 1, 2 An increased number of macrophages and smaller collagen fiber bundles further contribute to increased thickness in ethnic skin. 1 These features may be relevant when considering trends in aging and need for rejuvenation.
8.2.4 Microneedling: How It Works
Percutaneous collagen induction therapy, otherwise known as microneedling, has become a popular treatment modality for numerous dermatologic conditions. Mounting evidence shows a role for microneedling in the management of acne and other scars, hair loss, striae, pigmentary alterations, and rhytides (rejuvenation and resurfacing). 3, 4 Microneedling instruments are composed of rows of fine needles that either roll over or pierce the skin to create rapidly healing microchannels, with negligible injury to the epidermis, that separate bundles of collagen while concurrently stimulating the production of new collagen and elastin. 3 The dermal microchannels stimulate a cascade of inflammatory events including the release of fibroblast growth factor, platelet-derived growth factor (PDGF), and transforming growth factor α and β (TGF-α and TGF-β). 3 Subsequent fibroblast proliferation and migration result in the formation of new blood vessels and collagen, with the creation of a fibronectin network that serves as a matrix for both type III, and eventually type I collagen deposition. 3 For more detailed information on the mechanism of action of microneedling, please refer to Chapter 5.
Lasers (both fractional and nonfractional, ablative and non-ablative), chemical peels, and dermabrasion procedures have traditionally been employed for skin resurfacing. Though effective, adverse effects including scarring, postinflammatory pigmentary changes (hyper- and hypopigmentation), and prolonged recovery time, even with fractionated non-ablative lasers, have been seen, making them higher risk procedures for patients with skin of color. Microneedling has the advantage of piercing the skin while keeping the epidermis partially intact, thus resulting in an accelerated healing process with decreased risks for scarring and infections, as opposed to fully ablative procedures. The fact that microneedling involves no thermal energy and has no specific targeted chromophores is an added benefit because there is negligible risk of incidental thermal damage to melanocytes resulting in altered pigmentation. 5
There are a wide range of both electric-powered pen devices and fixed needle rollers that are used for microneedling with variable needle lengths, diameter, quantity, configuration, and material. Both function by smoothly rolling over the skin with a goal end point of fine pinpoint bleeding. The electrical pens have easily adjustable operating speeds and penetration depths. The electrical pens also have disposable needle tips that lower the risk of infection and allow for treatment of focal traumatic scars which is an advantage over the roller drum. 3
To achieve desired clinical outcomes, one must consider the location of treatment and appropriate needle depth. Understanding the relative differences in skin site, contour, and thickness help to optimize device selection and depth for different cosmetic procedures. Richard and colleagues examined 15 skin biopsy specimens from different facial sites on 3 fresh adult cadavers to determine the absolute relative values of skin thickness. As depicted in ▶ Table 8.2, the upper eyelid proved to have the thinnest skin of all sites examined compared to skin at other sites measuring at least twice as thick, with the nasal tip measuring three times the thickness of the upper eyelid. Findings of relative facial skin thickness have also been reillustrated on a facial map in ( ▶ Fig. 8.1). 4 Therefore, deeper needle penetration, 1.5 to 3.0 mm, will be required for thicker sebaceous skin, such as the cheeks, perioral regions, and scars or striae in various body parts. Comparatively, thinner skin in the periocular regions, forehead, and nasal bridge warrant needle depths ranging from 0.5 to 1.5 mm. It is important to note that the exact needle length may not correlate with the exact depth of penetration into the skin. For example, in one study devices that exceeded 1.0 mm in depth revealed a penetration depth that was lower than anticipated. 3 Therefore, there may be a discrepancy between a needle with increased length and the exact length it penetrates into the dermis. As such, we recommend assessing for pinpoint bleeding as an endpoint compared to trying to attain a particular level of depth penetration.

Fig. 8.1 Map of skin thickness on different parts of the face. While differences in skin thickness on the face of Caucasian skin versus skin of color is not known, it should be noted that studies have reported larger and more multinucleated fibroblasts in black versus white skin potentially resulting in differences in skin thickness. Note: ethnic/racial background of the subjects is not noted in the study that obtained these measurements.
(Adapted from Ha RY, Nojima K, Adams WP Jr., and Brown SA. Analysis of Facial Skin Thickness: Defining the Relative Thickness Index. Plast Reconstr Surg. 2005 May; 115(6):1769-73.)
Site | Relative skin thickness index (± SD) |
Upper lip | 2.261 + 0.539 |
Lower lip | 2.259 + 0.537 |
Philtrum | 2.260 + 0.375 |
Chin | 3.144 + 0.464 |
Upper eyelid | 1 + 0.000 |
Lower eyelid | 2.189 + 0.475 |
Forehead | 2.850 + 0.599 |
Right cheek | 2.967 + 0.661 |
Left cheek | 3.226 + 0.628 |
Malar eminence | 2.783 + 1.082 |
Submental | 2.403 + 0.500 |
Nasal tip | 3.302 + 0.491 |
Nasal dorsum | 2.020 + 0.478 |
Right neck | 1.497 + 0.824 |
Left neck | 1.530 + 0.764 |
Source: Adapted from Ha RY, Nojima K, Adams WP Jr., and Brown SA. Analysis of Facial Skin Thickness: Defining the Relative Thickness Index. Plast Reconstr Surg. 2005 May; 115(6):1769–73. 13 | |
Almost universally, estheticians may microneedle up to 0.2 to 0.25 mm in depth, which is to but not through the stratum corneum in all ethnic skin types, thus following the guidelines of being prohibited from performing any medical treatment. Microneedling devices with needles longer than 0.3 mm are classified as a class I medical device. As such, only licensed medical professionals, such as registered nurses, nurse practitioners, physician assistants, acupuncturists, and physicians, are allowed to microneedle at depths of that length or higher. Of note, needles with a longer length tend to result in longer downtimes. Currently available microneedling devices include the Eclipse Micropen (0.5–2.0 mm) and the MD Derma Dermapen (0.25–2.5 mm). 3
The stratum corneum continues to serve as one of the main obstacles to percutaneous absorption given it restricts the transient dermal delivery of topicals, including topical medications. Skin penetration can either be enhanced physically or chemically. Recently it has been shown that higher transdermal penetration can be seen on microneedle-injected sites. The microchannels created in the stratum corneum allow topicals to pass through and increased blood perfusion also results in increased delivery through the skin. 6 Vitamins A, C, and hyaluronic acid are vital in the assembly of new collagen. Thus combining microneedling with topical antioxidants, hyaluronic acid, or platelet-rich plasma (PRP), may aid in the enhancement of microneedling-induced wound healing. Priming the skin with topical prior to microneedling may also help to upsurge gene and protein expression that results in skin regeneration. 3, 6 It is recommended by the authors that any topical applied to the skin immediately pre- or post-microneedling be of a sterile nature as to avoid infection or biofilm formation.
8.2.5 Platelet-Rich Plasma: How It Works
Platelet rich plasma (PRP) is prepared by centrifuging a patient’s blood to produce a highly concentrated autologous solution of plasma with platelet concentrations of three to five times the amount found in the patient’s serum. 7, 8 The platelets will then release numerous growth factors including platelet-derived growth factor (PDGF), transforming growth factor (TGF-α and TGF-β, vascular endothelial growth factor (VEGF), and many others that stimulate the healing process via cell proliferation, differentiation, and migration. 7, 8, 9, 10, 11, 12, 13, 14 In addition, several proteins including fibrin, fibronectin, and vitronectin are included in PRP which help to provide structural support that is necessary for cell migration. As a result, increased fibroblasts and collagen contribute to the regenerative processes that are responsible for skin rejuvenation, scar revision, treatment of alopecia, and several other dermatologic conditions. 7, 10, 11 For a more in-depth background on the basic science of PRP, please see Chapters 2 and 3.
8.2.6 Summary
Melanin serves as a significant filter to block the damaging effects of UV light in darker skin types. However, melanocytes and ethnic skin show labile responses to cutaneous injury making conditions such as postinflammatory pigmentary changes, acne scarring, and melasma more common. 1, 2 Recently microneedling and PRP have been introduced into the armamentarium of cosmetic treatments used on ethnic skin. 1 Both are safer and effective therapeutic options as aesthetic treatments (whose properties may be augmented when combined together) with versatility and practicality for use on ethnic skin. 5, 9, 12
8.3 Microneedling
8.3.1 Skin Rejuvenation
As the demands for less aggressive yet effective cosmetic procedures continue to increase, recent data has shown microneedling to be effective for facial rejuvenation treating both photodamaged skin and rhytides. While genetics, behavior, gravity, and UV exposure substantially affect the overall aging process, these changes often happen at a slower rate and “later-in-life” in darker compared to fair skinned individuals. Caucasians tend to show more signs of photoaging in their fourth decade, while darker ethnic patients may not manifest signs until their fifth or sixth decade. 1 This fact is in part potentially due to increased epidermal melanin and increased fibroblasts in the dermis in ethnic patients compared to their age-matched lighter-skinned counterparts, as described above. Darker skin types exhibit fewer rhytides than Caucasians but will often develop roughly textured skin and mottled pigmentation as a result of photoaging. 1
However, there are fewer options for or higher risks when combating signs of photoaging. The risk of scarring and dyspigmentation results in less frequent use of ablative resurfacing for skin rejuvenation in ethnic patients. Posttreatment dyspigmentation after non-ablative resurfacing procedures is also a concern. 1 Multiple articles site microneedling as an effective treatment for rhytides and skin rejuvenation 2 Increased amounts of types I, III, and VII collagen and tropoelastin were found after six microneedling sessions in one study. Six months later, type I collagen and elastin persisted and no change in the number of melanocytes after the procedure was noted. 15, 16 The increased reorganized collagen and elastic fibers in the dermis are responsible for decreased rhytides and skin tightening observed in patients. 2, 15, 16 A 9-year retrospective analysis looked at 480 patients who underwent one to four microneedling sessions and achieved 60 to 80% clinical improvement when compared to baseline. 17 With regards to microneedling and rejuvenation in skin of color, there may be a lag time of up to 2 months from the start of treatment to view clinically apparent results. The recommended protocol for a treatment series is three to six biweekly or monthly microneedling sessions for facial skin to fully achieve optimal results in skin rejuvenation in skin of color. 2 For the body, sessions may need to be 4 to 8 weeks apart to allow for sufficient healing time.
8.3.2 Acne Scarring
Acne scarring and pigment changes that ensue as a result of acne vulgaris can have a dramatic impact on patients’ self-esteem and quality of life. 18, 19 Although significant advancements have been made in the development of laser resurfacing and its use on darker-skinned patients, microneedling has become a safer alternative compared to ablative or nonablative resurfacing, because microneedling does not emit significant amounts of thermal energy (heat), which can cause postinflammatory pigmentary changes and scarring. 1, 2 It mimics fractionated non-ablative laser therapy except with mechanical injury only.
Several studies demonstrate statistically significant improvement in acne scars among all or specifically darker skin types with microneedling as monotherapy but with fewer reports of postprocedure pigmentary alteration. 18, 20 Cachaferio et al conducted an evaluator-blinded randomized clinical trial in which 46 patients with atrophic acne scars underwent either non-ablative fractional erbium 1,340-nm laser versus microneedling (device: Dr. Roller, 192 microneedles, 2 mm length). While both groups demonstrated promising clinical results, 13.6% of the patients treated with laser therapy experienced postinflammatory hyperpigmentation, compared to no patients in the microneedling group. 18 In another study, 30 patients of FST IV to V with acne scars received five monthly microneedling sessions (device: Dermaroller, 192 microneedles, 1.5 mm length, 0.5 mm diameter). Photographs showed significant improvement of the scars with five patients (16.67%) developing postinflammatory hyperpigmentation, which gradually resolved in two of the patients after strict SPF compliance. The other three were lost to follow-up, so resolution was unknown. Hence, while postinflammatory pigmentary alteration can occur with microneedling, these studies and the authors’ experience demonstrate clear advantages of microneedling as a cost effective, repeatable, and relatively safe treatment for skin regeneration and scar reduction. 21
8.3.3 Pigmentary Disorders
Melasma
Microneedling has also been explored as monotherapy and as a means of transdermal drug delivery in ethnic skin for the treatment of disorders of hyperpigmentation. 2 Medium to dark brown patches on sun exposed areas, namely the forehead, cheeks, nose, upper lip, and rarely the neck or forearms, are the hallmarks of melasma. While the exact etiology is unknown, genetics; UV radiation (and to a lesser extent, infrared and visible light); as well as hormonal shifts such as those occurring during pregnancy or from contraceptive pills, hormonal replacement therapy, and even antiseizure medications may all play a role in the development of this acquired disorder. 22, 23 In addition to UV radiation itself, photo-induced hormones, growth factors, and chemical mediators of inflammation, including interleukins (IL-1a, IL-1b, and IL-6), tumor necrosis factor α, eicosanoids (prostaglandins [PGs] D2, E2, F2, and leukotriene B4), and histamine, influence the function of melanocytes directly or indirectly and may further contribute to pigmentary effects of UV light. 1, 24, 25 Topical lightening agents, chemical peels, dermabrasion, certain laser procedures, and even off-label systemic therapies have been explored but often with partial, temporary or unsatisfactory results. 22, 23 Incidental skin lightening noted during microneedling treatment for the correction of photodamage and acne scars has led to its use as monotherapy for melasma, yet there are few published studies, most with unimpressive or modest results. 26
In contrast, when used in combination with depigmenting agents, to enhance penetration, microneedling has proven to be advantageous. Recent studies have shown that topical tranexamic acid, inhibits UV-induced plasmin activity in keratinocytes by preventing the binding of plasminogen to the keratinocytes, which ultimately results in less free arachidonic acids and a diminished ability to produce PGs and thus, decreases melanocyte tyrosinase activity. 25 A randomized study of 60 patients with moderate to severe melasma (FST IV–V), compared microneedling plus topical tranexamic acid 4 mg/mL application (microneedling device: 192 microneedles, 1.5 mm length, 0.25 mm diameter) versus TA 4 mg/mL microinjections (100 U/mL insulin syringe with a 4 mm mesoneedle at 1 cm interval injections). There was 44% improvement in the microneedling group versus 35% in the microinjections group, a statistically significant difference after just 3 sessions per the Melasma area severity index (MASI) score. Furthermore, at least 50% improvement was seen in 41.38% of patients in the microneedling compared to 26.09% in the microinjection group. There were no adverse effects noted through the duration of this study. 2, 5, 22 In another trial investigating transcutaneous drug delivery via microneedling, Fabbrocini et al conducted a split-faced study of 20 women with melasma (FST III–V) who underwent microneedling (microneedling device: Dermaroller-Model CIT 8, which consists of 192 needles, needle length of 0.5 mm, and a diameter of 0.02 mm arranged in an array on a roller device) followed by application of a depigmenting serum with rucinol (a tyrosinase inhibitor) and sophora α (an α-MSH inhibitor) versus the depigmenting serum alone. After 2 months, the microneedling group improved by 10.1 points on the MASI score, while the non-microneedling group only improved by 7.1 points. 5, 6 MASI score < 10 was mild; 10 to 15 was moderate; and > 15 was severe ( ▶ Fig. 8.2). 27 The luminance index scores, a colorimetric evaluation that can objectively measure the expression of brightness in skin pigment, were also statistically significant (p< 0.05) in the patients that received combination therapy, with an increased brightness of 17.4%. 2, 6
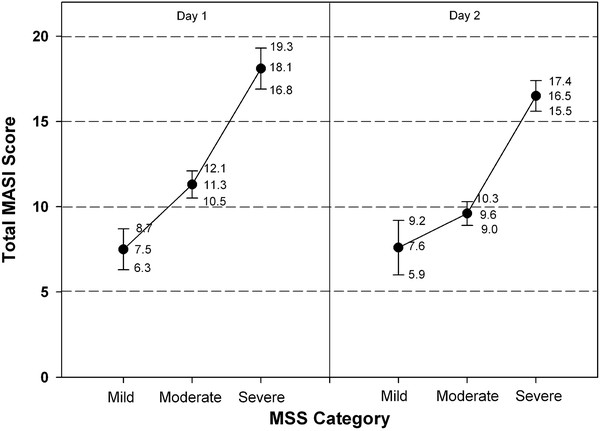
Fig. 8.2 Melasma area severity index provides representation for entry scores for patients with moderate to severe melasma. (Adapted from Pandya et al. 27 Reliability assessment and validation of the Melasma Area and Severity Index (MASI) and a new modified MASI scoring method. JAAD. 2011; 64(1); 78–83.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree