, Shimin Chang2, Jian Lin3 and Dajiang Song1
(1)
Department of Orthopedic Surgery, Changzheng Hospital Second Military Medical University, Shanghai, China
(2)
Department of Orthopedic Surgery, Yangpu Hospital Tongji University School of Medicine, Shanghai, China
(3)
Department of Microsurgery, Xinhu Hospital Shanghai Jiao Tong University, Shanghai, China
When Song et al. published their paper in 1984 on the thigh as a donor site for three new flaps with the anterolateral thigh, they closely fulfilled all the characteristics of a perforator flap [1].
After the first description by Song, it took several years until this flap became popular for different reconstructive purposes. With different focuses on the variety and shapes possible when using the conventional technique, a great number of clinical series with many different soft tissue reconstructions have been reported since the early 1990s [2–24].
19.1 Vascular Anatomy
After it arises from the lateral circumflex femoral artery, the descending branch reaches the medial rim of the vastus lateralis muscle in its proximal segment and courses distally to communicate with the superior genicular artery (Fig. 19.1).
Fig. 19.1
Vascular anatomy of the descending branch of the lateral circumflex femoral artery
Apart from the blood supply to the vastus lateralis muscle, the descending branch divides into the myo- or septocutaneous branches, giving the anatomical basis of the myocutaneous vastus lateralis or septocutaneous anterolateral thigh perforator flap.
19.2 Illustrative Case
A 29-year-old man was struck by a motor vehicle, sustaining an avulsion injury of his left dorsum foot with tibial shaft fracture. The soft tissue defect measured 16.0 cm × 9.0 cm after thorough debridement.


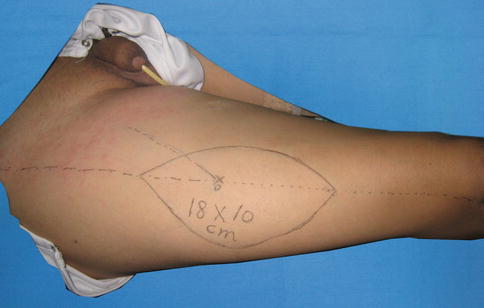
Fig. 19.2
Preoperative view
The perforators can be found a few centimeters proximal to the midpoint of the interconnection between the anterior superior iliac spine and the lateral rim of the patella (Fig. 19.4).
Fig. 19.4
Schematic drawing of the flap design
Perforator Vessel Visualization
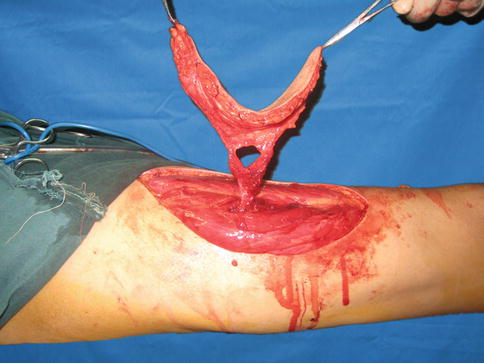
The skin incision is marked medial to the tensor muscle at the proximal thigh and straight above the rectus muscle toward the knee. Using magnifying loupe, these myocutaneous perforators become visible, entering the muscle along its undersurface at the anterior muscle rim (Fig. 19.5).
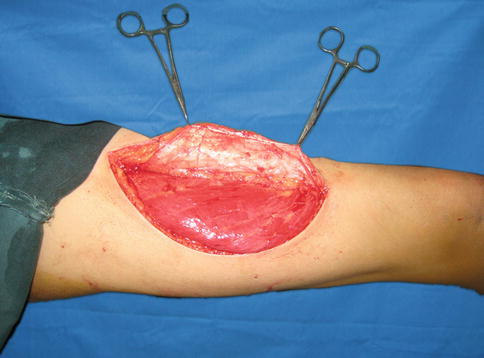
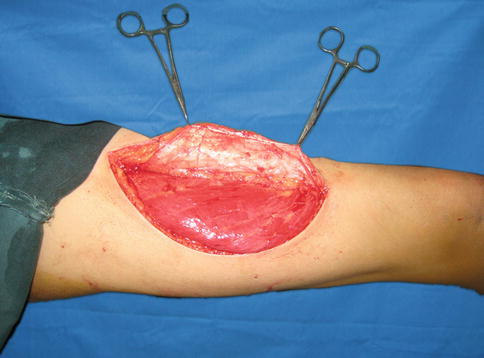
Fig. 19.5
Perforator vessel visualization
The rectus femoris and vastus lateralis muscles are bluntly separated from each other, and by retracting the rectus femoris muscle medially, the descending branch of the circumflex femoral artery with its two comitant veins becomes visible.
The myocutaneous perforator is followed through the vastus lateralis muscle.
Small side branches to the muscle are ligated or clipped, and the perforator is finally isolated with only a very small muscle cuff around it.
The skin paddle, which can now be designed in its final form, is raised completely (Fig. 19.7).
Fig. 19.7
Schematic drawing of the flap elevation
Flap Transfer and Insetting
Flap raising is finished with further dissection of the perforator in the proximal direction, until the descending branch of the lateral circumflex femoral artery is reached. The flap is now ready for microvascular transplantation (Fig. 19.8). The descending branch vessels were anastomosed with the anterior tibial vessels (A:V = 1:2) (Fig. 19.9).

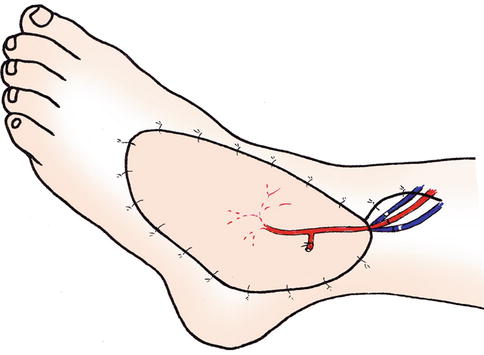

Fig. 19.8
Flap transfer and insetting
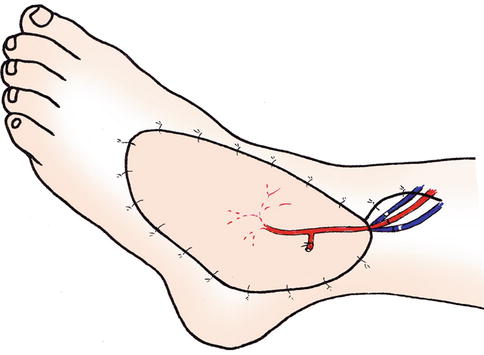
Fig. 19.9
Rebuilding the blood supply of the flap
The donor site was closed directly (Fig. 19.10).