Chapter 49 Anterior Cruciate Ligament Reconstruction Using a Mini-Arthrotomy Technique with Either an Ipsilateral or a Contralateral Autogenous Patellar Tendon Graft
Introduction
In the past 24 years, I have performed more than 5000 ACL reconstructions, and I have always used an autogenous patellar tendon graft for all the surgeries. I prefer to use the patellar tendon graft because it allows for quick and predictable bone-to-bone healing, is viable throughout the entire postoperative course,1 and can respond to stress during rehabilitation. Although any biological graft that is properly placed in the knee can achieve the same stability after surgery, the patellar tendon graft may allow for the fastest postoperative rehabilitation program because bone–bone healing is quicker than tendon–bone healing. Regardless of graft choice, proper rehabilitation must be done to give the best result.
Preoperative planning
Radiographs
Radiographs are obtained preoperatively to assist with surgery planning.
Plain radiographs, including standing posteroanterior 45 degrees flexed weight bearing,2 lateral, and Merchant3 views are obtained. The radiographs allow us to measure the width of the intercondylar notch, length of the patellar tendon, tibial slope angle, and width of the patella, which is usually twice the width of the patellar tendon. These measurements are helpful for planning the angle and length of the femoral tunnel and help determine the amount of notchplasty that may be needed to accommodate for the width of the new ACL graft. A magnetic resonance imaging (MRI) scan is not necessary for our preoperative evaluation but is reviewed if it has already been obtained elsewhere.
Rehabilitation
There is never a reason to do an isolated ACL reconstruction as an emergency surgery. Previous studies have shown that acute ACL reconstruction has a higher rate of postoperative arthrofibrosis than delayed ACL reconstruction when the patient has the opportunity to undergo rehabilitation to allow the knee to return to a quiescent state.4,5 All patients are evaluated by a physical therapist at the time of my initial evaluation. The physical therapist measures knee range of motion and strength before surgery and determines when the patient is ready to undergo surgery. The patient must have full knee range of motion equal to the contralateral normal knee, good leg control, and no knee swelling before he or she can undergo surgery. Furthermore, the patient must be mentally prepared for surgery. The surgery and rehabilitation program are fully explained to the patient and his or her caregiver so that they fully understand what is expected of them after surgery. The surgery date is planned for a time when the patient has at least 1 week off school or work and when a family member or friend can be at home with him or her during the first week postoperatively.
Technique
Exposure
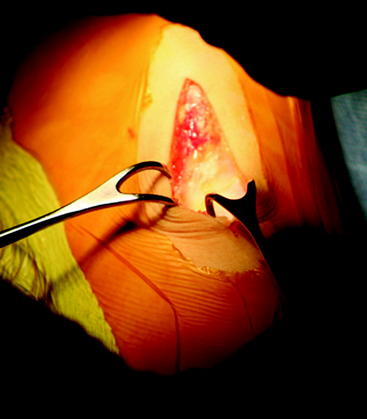
The tourniquet is left inflated to 300 mHg/psi (350 mHg/psi for larger thighs). The Ioban drape is taken off the skin just over the site where the skin incision is to be made. A 6-cm incision is made down to the deep fascia along the medial side of the patellar tendon, starting 1 cm above the inferior pole of the patella and extending 4 cm distal to the joint line (Fig. 49-1). The subcutaneous tissue is separated from the deep fascia medially where the tibial tunnel is to be drilled 4 cm distal to the joint and 1 cm medial to the tibia tubercle. The subcutaneous tissue is separated from the deep fascia with Metzenbaum scissors and finger dissection approximately 1 to 2 cm medial to the patellar tendon.
Tibial Exposure
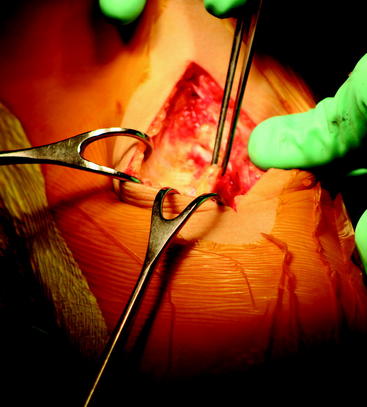
The deep fascia and periosteum of the proximal tibia are incised with electrocautery starting from the joint line and extending distally along the medial edge of the patellar tendon for 4 cm, then cutting at a right angle for another 2 cm to outline a flap to the level just proximal to the pes anserinus. The periosteum/fascial flap is lifted with a periosteal elevator to expose bare bone where the tibial tunnel will be created, made, and drilled (Fig. 49-2). Exposure at this level will ensure the tibial tunnel will be at least 40 mm long for the 25-mm bone plugs. The flap is kept as thick and continuous as possible to allow for closure of the soft tissue over the polyethylene button used for fixation, which has reduced the need for postoperative hardware removal.
Femoral Exposure
The table is elevated so that the femur is close to eye level. The foot of the bed is lowered so that the knee is flexed to 90 degrees. The bump under the thigh may need to be adjusted to allow for 90 degrees of flexion. The goal is to expose the flat surface of the lateral femoral cortex above the metaphyseal flare. The 3-cm lateral oblique incision is made about 4 to 5 cm above the superior pole of the patella along Langer’s lines (Fig. 49-3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree