Ankle Reconstruction With Free Flap
Sean S. Li
Ahmed Suliman
Deepak M. Gupta
DEFINITION
The ankle has limited soft tissue for protection of vital structures, and trauma or tumor extirpation often leads to exposed tendons, bone, vessels, or nerves.
There are few reliable local flaps that can be used for coverage in this area.
Impaired blood flow is also typical of the distal lower extremity especially in high-risk patients with comorbidities such as smoking, diabetes, peripheral arterial disease, and venous insufficiency, which may result in ulceration, infection, and necrosis of the soft tissues ultimately requiring free flap coverage.
Due to the complexity of the ankle, reconstruction ideally should be approached in a multidisciplinary fashion consisting primarily of collaboration between plastic and orthopedic surgeons but also with consideration of consultation of infectious disease and vascular surgery.
ANATOMY
The ankle is a hinge joint with articulations between the tibia, fibula, and talus.
Defects in the ankle commonly expose bone or orthopedic hardware, usually at the tibia or the medial and lateral malleoli.
Five nerves supply the foot and ankle—saphenous, sural, deep peroneal, superficial peroneal, and tibial nerves.
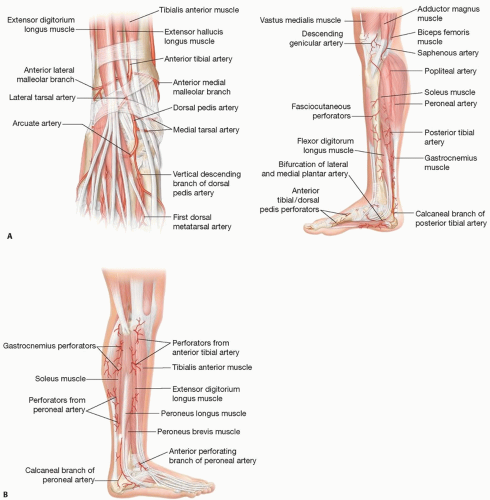
Knowledge of the ankle’s vascular anatomy is essential for limb salvage. The distal lower extremity’s arterial supply is primarily supplied by three vessels: posterior tibial (PT), anterior tibial (AT), and peroneal.
The AT artery branches from the popliteal artery, and its course across the ankle is shown (FIG 1, left).
The PT and peroneal arteries originate from the tibioperoneal trunk, and their courses across the ankle are shown (FIG 1, right).
PATHOGENESIS
Defects of the ankle requiring free flap reconstruction originate from trauma (FIG 2), tumor extirpation, and peripheral vascular disease.
PATIENT HISTORY AND PHYSICAL FINDINGS
Evaluation of the patient begins with history and physical focusing on the following:
Eliciting the etiology of the wound and presence of comorbidities including smoking, diabetes, obesity, and peripheral vascular disease
Assessing the overall function of the patient and considering the potential outcomes for the patient and bearing in mind the patient’s rehabilitative potential, motivation, and compliance. Location, size, depth, character of the wound, and exposed structures
Neurological, vascular, and skeletal evaluation of the lower extremities utilizing physical exam, imaging, and Doppler
IMAGING
Plain films of the defect should be obtained to evaluate for fractures and bony defects with further computed tomography imaging to be considered depending on complexity of the injury.
If physical or Doppler exam reveals inconclusive vascular status or if peripheral vascular disease is suspected, preoperative arteriography may be obtained.
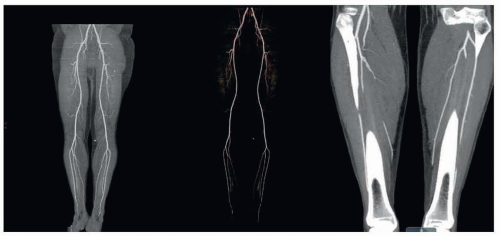
Computed tomographic angiography (CTA) (FIG 3) can obtain vascular information valuable for flap planning and assessing the recipient site without risk of complications associated with arterial puncture of the groin.
Selective preoperative CTA may be considered in patients who have lost peripheral pulses, had a neurological deficit secondary to the injury, or of a compound fracture that has undergone reduction and external or internal fixation.2
NON OPERATIVE MANAGEMENT
Defects in the ankle that typically require free flap reconstruction have exposed hardware, tendon devoid of paratenon, vessels, nerves, open joint(s), or bone denuded of periosteum.
These defects if managed nonoperatively will not heal and can potentially lead to further tissue loss, osteomyelitis, loss of function, or amputation.
SURGICAL MANAGEMENT
The goal of reconstruction is to achieve a healed wound to allow function.
In the ankle, the aims are to allow the patient to wear normal footwear, avoid bulky flaps, and return to weight bearing and ankle motion.
Selection of flaps is based on morbidity of the donor site and accessibility of local tissue.
Regardless of the flap selection, the principles for reconstruction include adequate debridement, restoring skeletal support, and anastomosing of the flap vessels outside of the zone of injury.3
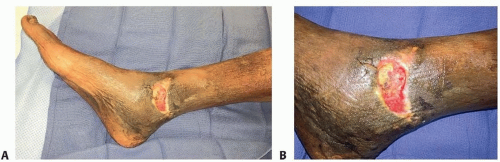
FIG 2 • A. Exposed bone of medial malleolus, denuded of the periosteum, chronic inflammation, and scarring of surrounding soft tissues. B. Necrotic bone within medial malleolus wound.
After the evaluation of the patient as a whole in regard to their systemic conditions, socioeconomic factors, extent of injury, and rehabilitative potential, a decision for amputation versus salvage can be made.
The decision for free flap reconstruction goes hand-inhand with the patient’s orthopedic injuries and potential for functional recovery.
Scores such as the Mangled Extremity Severity Score (MESS), Predictive Salvage Index, and the Limb Salvage Index can be used to assist in the decision-making for amputation versus salvage.4
Absolute indications for amputation include complete disruption of the posterior tibial nerve in adults and crush injuries with warm ischemia time greater than 6 hours.
Relative indications of amputation include serious associated polytrauma, severe ipsilateral foot trauma, and prolonged anticipated course to soft tissue coverage and tibial reconstruction.
Preoperative Planning
If reconstruction is indicated, the following must be considered:
Bony stability is first established by utilizing external or internal fixation devices.
External devices are usually preferred if there is significant bone loss or bone devascularization.
In contaminated wounds, multiple stages of debridement may be required until an adequate wound bed without devitalized or infected tissues is achieved.
Vacuum-assisted closure decreases need for dressing changes and can promote healing.5
Osteomyelitis can follow severe open fractures with massive contamination or devascularized tissue; management includes resection of dead or infected bone, flap coverage with obliteration of dead space, and antibiotic treatment.6
Timing of reconstruction
If the general condition of the patient and the status of the wound are adequate, definitive coverage should not be delayed.
Zone of injury9
Many lower extremity wounds result from high-energy trauma that creates a significant “zone of injury.”
This zone is highly thrombogenic and extends beyond what is macroscopically evident.
Failure to recognize the true extent of the zone is a leading cause of microsurgical anastomotic failure.
Within this zone, there is increased friability of the vessels and increased perivascular scar tissue.
Selecting a recipient vessel outside of this zone of injury with good vessel wall pliability and high-quality blood flow from the transected end of the vessel is essential for successful microsurgical anastomosis.
Coverage after tumor extirpation
Free flap reconstruction must withstand radiation therapy and/or chemotherapy with the goal of preserving function and achieving an acceptable appearance and function.
Close cooperation with oncologists and knowledge of prognosis/risk of recurrence/survival, tumor characteristics, behavior, and adjuvant treatment is necessary to plan for the correct type of reconstructive procedure.
Exposed hardware
Traditionally management involved irrigation and debridement, antibiotics, and removal of hardware.
However, if the hardware is clinically stable, exposure is less than 2 weeks, the infection is controlled, and the hardware is utilized for bony consolidation, then the likelihood of salvage with soft tissue coverage is increased.10
Reconstruction in patients with a two- or one-vessel extremity
Consider vascular bypass surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree