3 Anesthesia
Topical Anesthetics
Common anesthetics include the following:
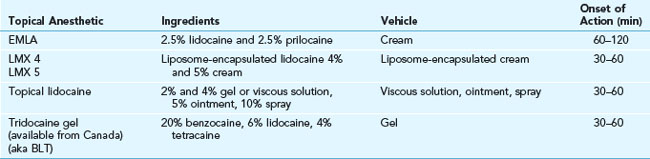
Table 3-1 shows the onset of action for the most commonly used topical anesthetics in skin procedures. EMLA (eutectic mixture of local anesthetics) cream consists of 2.5% lidocaine and 2.5% prilocaine in an oil-in-water emulsion. This anesthetic cream works best if applied for 30 minutes under occlusion or 60 minutes without occlusion before anesthesia is needed. It can be useful in treating children or a patient of any age who is afraid of needles. EMLA cream is used for some laser procedures, superficial light electrodesiccation of benign growths, and curettage of molluscum contagiosum. In Figure 3-1B the EMLA has been applied to the lower eyelids before electrodesiccation of syringomas. EMLA is available in 5-g tubes with occlusive dressings or in 30-g tubes without dressings. EMLA should not be used in infants younger than 3 months because the metabolites of prilocaine form methemoglobin. In one randomized control trial, EMLA and LMX 4 provided comparable levels of anesthesia after a single 30-minute application under occlusion prior to electrodesiccation of dermatosis papulosa nigra.1
EMLA Technique for Intact Skin
Topical Refrigerants/Cryoanesthesia
Liquid nitrogen can freeze the skin to cause a numbing effect; however, its use causes immediate pain and little real anesthesia. Rather than using liquid nitrogen for local anesthesia for skin tag excision, it is easier and less painful to use the liquid nitrogen with a Cryo Tweezer to treat the skin tags directly (see Chapter 15, Cryosurgery). Also, liquid nitrogen can be sprayed or directly applied to skin tags or molluscum rather than using it as anesthesia. This also avoids the need to deal with blood and hemostasis issues.
Contact cooling devices and assistive external devices are frequently used in laser treatments and are covered in Chapter 20, Anesthesia for Cosmetic Procedures.
Local Anesthesia by Injection
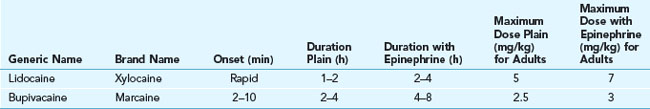
Lidocaine is the most widely used local anesthetic for injection in skin surgery. Bupivacaine (Marcaine) is used occasionally when long-lasting anesthesia is desired. Lidocaine has the advantage of having a more rapid onset (within 1 minute) and shorter duration of anesthesia than bupivacaine. This shorter duration is sufficient and preferable for most skin surgery. When lidocaine is mixed with epinephrine, it lasts almost as long as bupivacaine and hurts less.2 See Table 3-2 for a comparison of amide local anesthetics.
1% Lidocaine with Epinephrine
For most skin surgery procedures, the recommended anesthetic is 1% lidocaine with epinephrine. Its advantages include almost immediate anesthesia, adequate duration of anesthesia, and decreased bleeding because of the epinephrine. The incidence of true allergies is negligible. Lidocaine without epinephrine has a duration of 1.5 to 2 hours, whereas lidocaine with epinephrine has a duration of 2 to 6 hours.3 The most common commercial preparation contains 1% lidocaine (10 mg/mL) with 1 : 100,000 of epinephrine. In a study that measured the effect of subdermal injection of lidocaine combined with epinephrine on cutaneous blood flow, laser Doppler imaging demonstrated an immediate decrease in cutaneous blood flow, which was maximal at 10 minutes in the forearm and 8 minutes in the face.4
Note that the initial skin blanching with injection is due to hydrostatic pressure along with the effect of epinephrine. When hemostasis is critical to the procedure, it is best to wait 8 to 10 minutes for the epinephrine to produce maximal vasoconstriction. Waiting is less important for shave biopsies of lesions that are not very vascular in patients who are not anticoagulated (Figure 3-2). Injecting enough anesthetic so that the skin is firm can limit the amount of bleeding because small blood vessels become compressed by the anesthetic fluid (Figure 3-3).
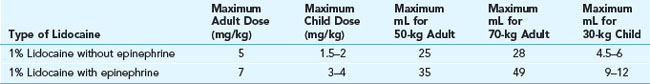
Maximal Doses
Maximal safe doses of 1% lidocaine with or without epinephrine are found in Table 3-3. Above these doses the risk of neurotoxicity and seizures is increased. In most adults (over 50 kg) up to 35 mL of 1% lidocaine with epinephrine is safe. Use of 1% lidocaine is preferable to 2% in most cases because a larger volume of anesthesia produces greater hemostasis and makes most cutaneous surgery easier to perform. Two percent lidocaine without epinephrine is useful in various nerve blocks including digital blocks when less volume is needed. Some clinicians prefer 2% lidocaine with epinephrine when they want to avoid tissue distortion from too much anesthetic volume. In this case, toxicity is not an issue because less than 5 mL of anesthesia are being used.
Decreasing the Pain of Local Anesthesia
Techniques to decrease the pain caused by injection of local anesthesia include the following:
The main technique for decreasing the pain of injection is to inject the local anesthetic very slowly using a small-gauge needle (27 or 30 gauge). The larger the gauge number, the smaller the needle diameter and the less painful the injection. Use 30-gauge needles on the most sensitive areas including the face, the ears, the fingers, and the genitals. When injecting anesthesia for a laceration repair, injecting from within a laceration is less painful than injecting into intact skin.5
Adding sodium bicarbonate (8.4% for injection) in a 1 : 10 dilution to the lidocaine and epinephrine anesthetic solution markedly decreases the pain caused by injection (e.g., 1 mL of sodium bicarbonate can be added to 9 mL of lidocaine). The addition of sodium bicarbonate neutralizes the commercially available lidocaine-epinephrine solutions that have a pH of 4 to 6. Although this takes more time, your patients will appreciate that the injection is less painful. The lidocaine-bicarbonate syringes need to be made at the time of use or may be kept for 1 week at room temperature and up to 2 weeks with refrigeration.6 In our office we make the following syringes each morning:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree