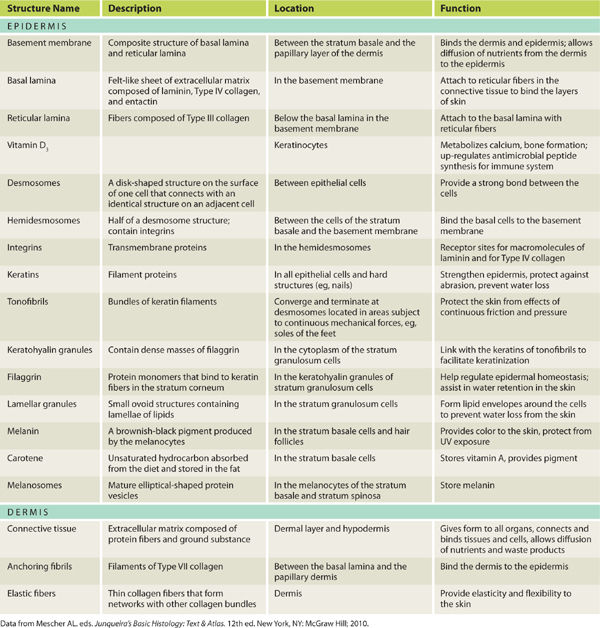
TABLE 1-2 Noncellular Components of the Skin
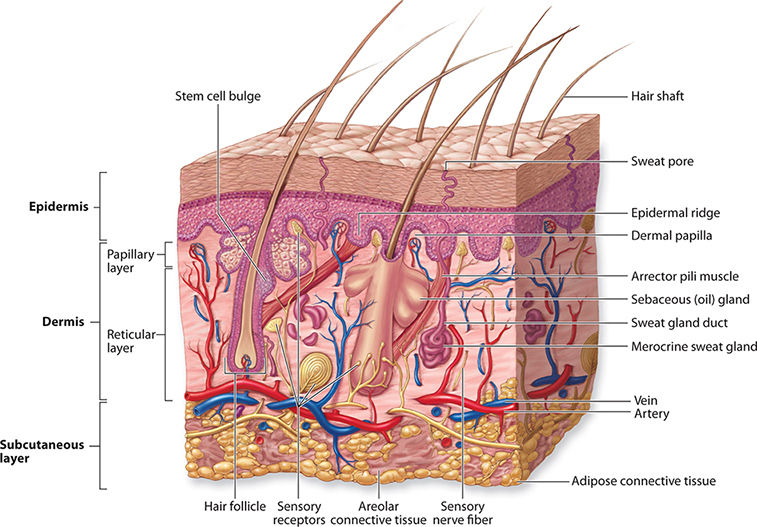
The layers of the skin are organized into the outermost epidermis and the underlying dermis. Beneath the dermis is a structure called the hypodermis or subcutaneous layer, although it is not a true part of the skin. (FIGURE 1-1) The junction of the epidermis and dermis is reticular, with an individualized pattern that forms dermatoglyphs, or the fingerprints and footprints, of the hands and feet.1 The reticular structure allows the skin to withstand the repeated friction and shear forces that occur with activities of daily living; however, as the skin ages the ridges flatten out and the skin is more susceptible to frictional tears and blistering. Between the epidermis and dermis is a laminar adhesive layer termed the basement membrane that binds the two layers of the skin.
FIGURE 1–1 Anatomy of the skin
Epidermis
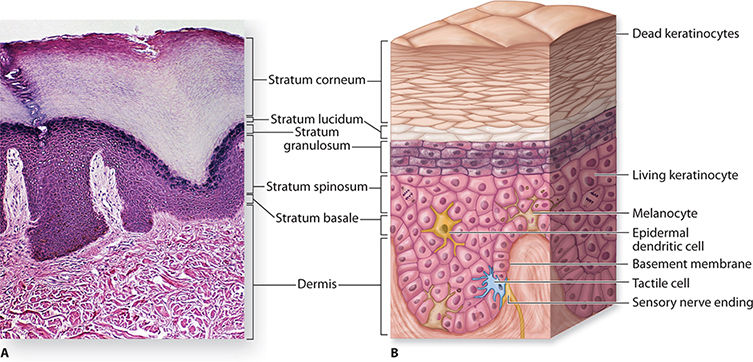
The layers of the epidermis are, from innermost to the surface, stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum; in totality the layers are 50–150 μm in thin skin, 400–1400 μm in thick skin.1,2 (FIGURE 1-2) The primary cells composing the epidermal layers are keratinocytes, with melanocytes, Langerhans cells, and Merkel cells embedded in layers. The keratinocytes are mitotically active in the stratum basale, but through a process defined as stratification, they migrate outward to the avascular stratum spinosum and begin to flatten out and become less active. When they reach the outer stratum corneum, the keratinocytes are termed corneocytes, dead flat cells that form the outer protective layer of the skin.
FIGURE 1–2 Layers of the epidermis
Stratum basale—composed of a single layer of cuboid cells, attached to the underlying dermis by the basement membrane. The stratum basale is constantly producing epidermal cells (keratinocytes) from stem cells located in both the basal layer and in the bulge of the hair follicles in the dermis.
Stratum spinosum—composed of slightly flattened cells that are responsible for protein synthesis, primarily keratin that forms bundles called tonofibrils. This is the thickest layer of the epidermis.
Stratum granulosum—composed of flattened cells that are undergoing terminal differentiation as they approach the outermost layer of skin. The intercellular spaces are filled with a lipid-rich material that forms a sheet or envelope around the cells, thereby making skin a barrier to both water loss and extrinsic foreign material.
Stratum lucidum—composed of 3–5 layers of flattened eosinophilic cells, creating a clear or translucent layer located only in the soles of the feet and palms of the hands. Cells contain densely packed keratin and are connected by desmosomes. Provides thickness and strength to withstand friction to the soles and palms.
Stratum corneum—composed of 15–20 layers of dead keratinized cells that are continuously being shed in a process called desquamation.
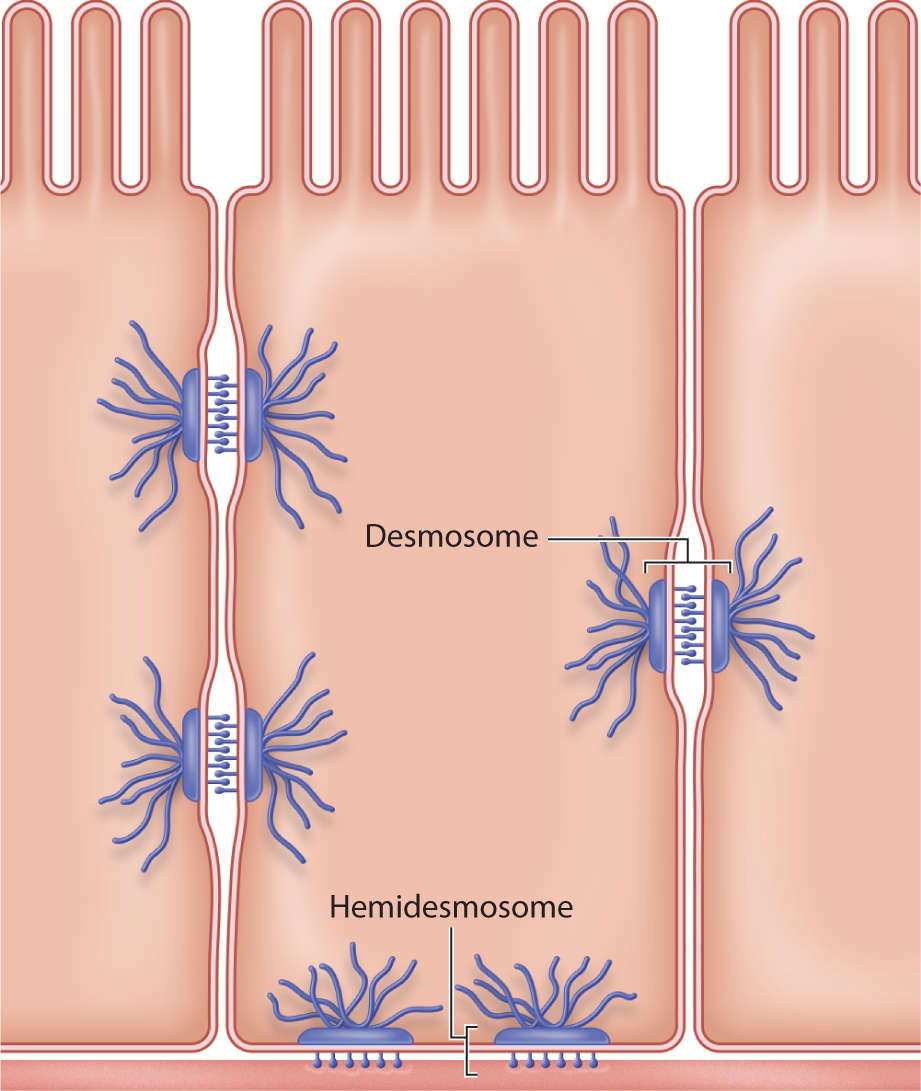
The keratinocytes are composed of keratin protein filaments, present in greater concentrations as the cells migrate toward the stratum corneum. In the stratum basale, the keratinocytes are bound to the basal lamina by hemidesmosomes; and in all the epidermal layers, to each other by desmosomes. These cell-to-cell adherent discs are composed of transmembrane glycoproteins, termed cadherins, and include four desmoglein proteins (FIGURE 1-3).3
FIGURE 1–3 Cell adherence with desmosomes and hemidesmosomes Desmosomes are adherent glycoprotein discs that bind keratinocytes to each other. Hemidesmosomes are adherent glycoprotein half-discs that bind keratinocytes to the basement membrane between the stratum basale and the dermis.
As the keratinocytes move into the stratum spinosum, they become active in keratin or protein synthesis. The keratin forms filament bundles called tonofibrils that converge on the hemidesmosomes and desmosomes to give the skin strength to withstand friction or shear force. As the keratinocytes migrate into the stratum granulosum, filaggrin (derived from “filament-aggregating protein”) binds to the tonofibrils, thereby forming an insoluble keratin matrix that “acts as a protein scaffold for the attachment of cornified-envelope proteins and lipids that together form the stratum corneum.”4 Also in the stratum granulosum, lamellar granules containing many lamellae of lipids undergo exocytosis, releasing a lipid-rich material into the intercellular spaces and forming envelopes around the protein-filled cells that are undergoing keratinization.1 This combination of tightly adhered filaments and lipid-rich envelopes is what gives the skin its ability to serve as both a barrier to loss of water from the body and protection from extrinsic foreign material.
The stratum lucidum is present primarily in the thick, hairless skin of the palms and soles (termed glabrous skin) and consists of dead, clear keratinocytes, thus the term “clear layer.” The stratum lucidum is between the stratum granulosum and the stratum corneum and provides the palms and soles more protection from friction and serves as a greater moisture barrier.
When the keratinocytes enter the stratum corneum, they are flat and keratinized with modified adhesive desmosomes, termed corneodesmosomes.5 Filled with proteins encased in plasma membranes, they are called squames, hence the term desquamation, meaning they are continually sloughed or shed. Over a period of 30 days, the entire process of migration and desquamation is completed and the epidermis is renewed.
Dermis
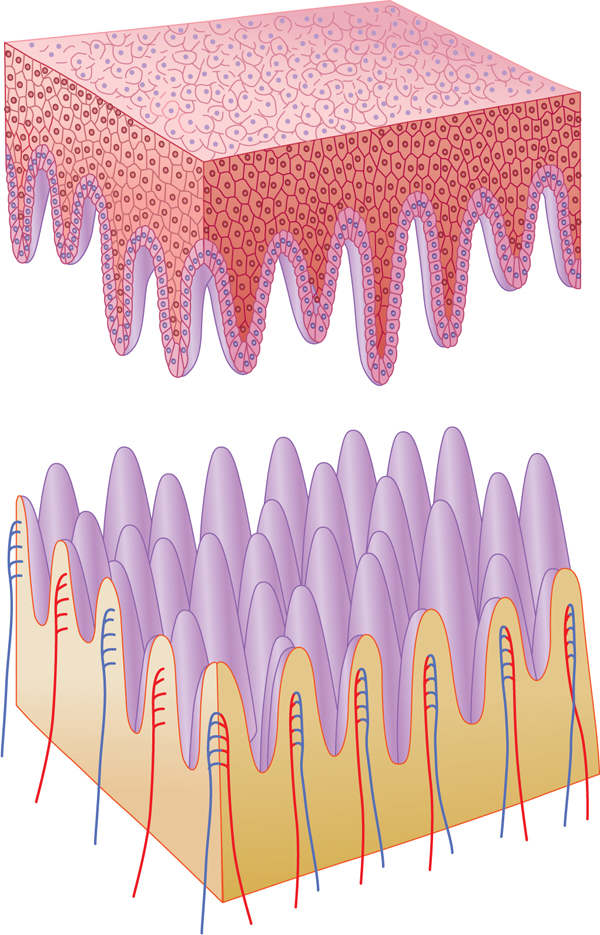
The dermis is composed of connective tissue and binds the epidermis to the hypodermis or subcutaneous tissue. The extracellular matrix of the dermis is composed of collagen (mostly Type I), elastic fibers, and ground substances such as glycosaminoglycans (GAGs) and proteoglycans. The uppermost surface of the dermis is reticular and interdigitates with the ridges of the epidermis; the structures are termed epidermal pegs and dermal papillae. (FIGURE 1-4) Between the dermis and epidermis is the basement membrane, consisting of the basal lamina and the reticular lamina. Besides holding the two layers together, the basement membrane allows the nutrients from the dermal vasculature to pass through to the avascular epidermis.
FIGURE 1–4 Dermal/epidermal junction The epidermal/dermal junction is composed of dermal papillae and epidermal pegs that interdigitate to create a bond that will withstand friction and shear forces on the skin. The junction flattens with age, making geriatric skin more susceptible to skin tears.
The acellular dermal components are the extracellular matrix, anchor fibrils of Type VII collagen linking the dermal papillae and the basal lamina, and the elastic fibers that are intertwined with the other collagen fibers to give flexibility and elasticity to the skin. The cellular components of the dermis are illustrated in FIGURE 1-1 and their role in dermal physiology is discussed in the section on function of the skin. The papillary layer contains the fibroblasts, mast cells, and macrophages, as well as some extravasated leukocytes.1 The reticular layer is composed of dense, mainly Type I collagen and contains the vasculature, nerve endings, glands, hair follicles, and more elastic fibers.
The hypodermis, or subcutaneous layer, is not anatomically part of the skin; however, it is the structure that binds the skin to the underlying structures. It is composed of loose connective tissue, vascular supply, and adipose cells that vary in number at different body areas and also among individuals. The hypodermis allows the skin to move freely over the underlying structures, thereby facilitating fluid muscle and joint movement.
SKIN PHYSIOLOGY
Vascular Supply
The dermis contains several microvascular blood vessel plexuses and lymphatic vessels that are parallel to the skin surface. (See FIGURE 1-1) The larger arterioles and venules are in the deep reticular layer with smaller vessels extending into the papillary layer and terminating in capillary loops. Blood flow through the capillary loops is controlled by highly innervated arterioles,6 and their close proximity to the basement membrane allows the blood supply to feed the deep keratinocytes of the epidermis. Between the larger deep plexus and the capillary loops are numerous arteriovenous anastomoses or shunts that play a major role in maintaining constant body temperature during hot and cold weather conditions. Lymphatic terminal vessels are little sacs interspersed with the capillary loops, controlled by a filament anchored to the connective tissue. As the filament moves, it opens a flap to the lymphatic vessels, thereby facilitating transport of excess interstitial fluid, protein molecules, and fat molecules out of the dermis. (Refer to Chapter 5, Lymphedema.)
Nerve Supply
Because of its large and superficial surface area, the skin contains the sensory receptors necessary for the body to process the external environment. The nerve endings are either unencapsulated (have no glial or collagenous covering) or encapsulated (have a covering of glia and connective tissue capsules).1,7 When the nerves cross the dermal/epidermal junction, they lose the Schwann cell covering and exist in the epidermal pegs as free nerve endings. Also in the granulosum basale are unencapsulated mechanoreceptors termed tactile or Merkel cells. It is also thought that in addition to external stimuli, the keratinocytes have a role in stimulating the nerve receptors by the release of neuropeptides.8
Skin Nutrition
Much has been written, and even more spent, on nutrients, supplements, and topicals to maintain skin nutrition and ergo youth. While there are no double-blind, placebo-controlled studies to support what is call the “inside-out” approach to maintaining skin integrity, there are certain vitamins and antioxidants that are known to play a role in skin health, in large part by their antioxidant effects.9 These substances and their functions are listed in TABLE 1-3.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree