This article discusses the surgically relevant anatomic and physiologic tenets of the aging neck. Procedures performed to rejuvenate and contour the aging neck can be challenging. A thorough understanding of the underlying neck anatomy, as well as the physiology associated with aging, is critical for surgical planning, execution, and achieving aesthetically pleasing outcomes. These topics are reviewed and used as the foundation for a discussion of various other techniques.
Key points
- •
The skin’s ability to conform to the newly contoured neck shape depends on the skin’s inherent pliability and texture, and is often related to its elastin and collagen content, which diminishes with age.
- •
Thick-skinned and overweight patients should not expect dramatic, long-lasting results of their neck contouring procedure because of gravitational forces and the weight of the tissues.
- •
The platysma courses inferolateral to superomedial, with 3 variations in patterns of interdigitation or decussation in the midline submental region.
- •
Patients with minimal or no platysmal decussation can have interplatysmal fat in the submental region herniate between the medial edges, which is contiguous with the deep subplatysmal fat, further contributing to the appearance of neck aging.
- •
Bone resorption at the level of the mentum, mandibular body, and mandibular angle contribute to the clinical appearance of aging, with changes seen at the cervicomental angle as well as the overall superficial topography of the neck.
Introduction
Neck rejuvenation and contouring procedures continue to expand and evolve, with a multitude of techniques designed to address the clinical consequences related to aging. Patients present with concerns regarding the aged appearance of their neck, often caused by changes in skin quality, fat accumulation, muscle tone, sun damage, or changes after weight gain or loss. The principal contouring techniques in neck rejuvenation are designed to transform specific regions of the neck by reduction and/or relocation of volume, redundancy, or laxity. This article focuses on the respective anatomic levels of the neck, which allows a more systematic approach when evaluating and treating patients with signs of neck aging.
Anatomy and Physiology by Anatomic Structure
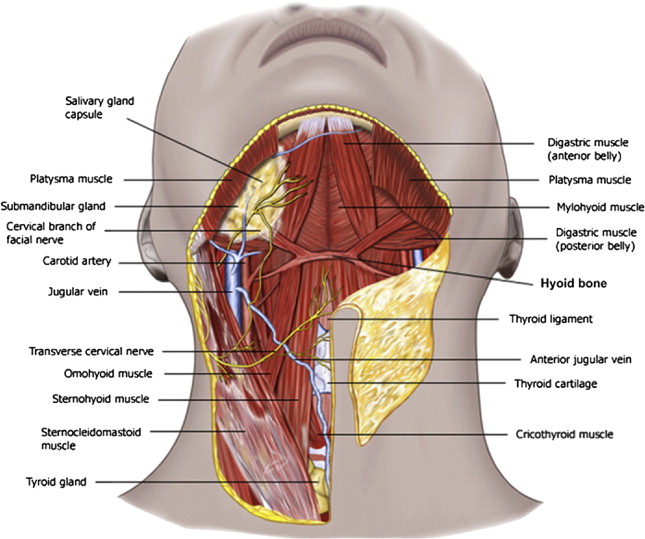
Patterns of aging are variable. Those patients with thin necks, good skeletal support, and good neck height age differently from those patients with heavy, short necks and poor mandibular support. The superficial topography of the neck also affects the perception of a youthful or aged neck. The interplay of the structures deep to the skin, and the skin’s ability to drape over them, is what determines this topography. These relationships have a bearing on the patient’s final results when a surgeon attempts to form an acute cervicomental angle (CMA), shape a distinct inferior mandibular border, or accentuate the anterior border of the sternocleidomastoid muscle (SCM), all of which have been thought to contribute to the attractiveness of the neck ( Fig. 1 ). In addition, the anatomic transition of the neck to the lower third of the face (neck-face interface) is fundamental to the overall facial aesthetic. Classification schemas have been developed by several investigators to characterize the aging process of the face and neck. When assessing candidacy for possible facial and neck rejuvenation, the senior author uses a 3-tier classification system, which focuses on skin laxity, submental lipoptosis, jowling, platysmal banding, and the CMA.
The neck can be separated into anterior and posterior triangles, and although the posterior neck can show signs of aging, this article focuses on the anterior neck. The anterior triangles of the neck are bounded inferiorly by the sternal notch and clavicles, and laterally by the sternocleidomastoid muscle (SCM) bilaterally. The trachea, thyroid, and cricoid cartilages represent the midline, dividing right from left. Posterior to the SCM demarcates the start of the posterior triangle, with the trapezius, occipital scalp, and cervical vertebrae forming the posterior boundaries. The superior aspect of the anterior neck is delineated by the chin and the lower mandibular line and angle, rising toward the mastoid processes more posteriorly.
Analyzing each layer from superficial to deep, therapies can then be tailored to specific anatomic structures and relationships, further individualizing a patient’s treatment plan based on previously agreed-on goals and expectations.
Skin
Skin changes within the neck can often be the most prominent feature seen with aging. Understanding the anatomic and physiologic processes involved with skin aging is of great importance in formulating individual treatment algorithms.
The sensory innervation of the anterolateral neck skin is derived from the transverse cervical nerves (C2, C3, C4) as they sweep across the neck from around the lateral border of the SCM. The arterial blood supply of the superficial anterolateral neck is derived from branches of the subclavian arteries, as well as perforating branches from the external carotid arteries. The intermuscular and superficial fascias serve as the framework for the vessels coursing to the skin. The external jugular vein and anterior communicating veins join the anterior jugular system and travel underneath the platysma to drain the superficial neck structures.
The skin acts as a protective barrier that is continuously in contact with the environment, undergoing not only chronologic aging but also photoaging as a consequence of primarily sun-induced damage from ultraviolet irradiation. Sun-induced skin aging (photoaging), like chronologic aging, is a cumulative process. Both processes lead to the formation of reactive oxygen species and resultant damage to cellular components, including membranes, enzymes, nucleic acids, and proteins, and disruption to the interactions between them. Additional processes that result in the clinical appearance of aging include shortening of chromosomal telomeres, hormonal influences, as well as an age-associated decline in anabolic signaling molecules and receptors, and upregulation of the reciprocal catabolic factors. These cellular perturbations manifest clinically as xerosis, laxity, wrinkles, droopiness, loss of hair, and loss of color from melanocyte depletion and decreased tyrosinase activity. Poikiloderma of Civatte is a common dermatologic condition seen in aging female patients that can cause cosmetic imperfections in the skin of the neck and chest. Often difficult to clear clinically, patients can show atrophy, pigmentary changes, as well as telangiectasia formation.
On histology, epidermal senescence primarily results in a decrease in the number of melanocytes and Langerhans cells. In contrast, most clinical aging and histologic changes occur within the dermis, with hypocellularity and flattened dermoepidermal junction rete ridges. There is disintegration of the dermal matrix leading to volume loss, as well as findings of fewer and looser collagen fibers and functional fibroblasts. A summaries of the histologic changes accompanying skin aging is shown in Table 1 .
| Epidermis | Dermis | Appendages |
|---|---|---|
| Flattened dermoepidermal junction | Atrophy (loss of dermal volume) | Depigmented hair |
| Variable thickness | Alteration of connective tissue structure | Loss of hair |
| Variable cell size and shape | Fewer fibroblasts | Conversion of terminal to vellus hair |
| Occasional nuclear atypia | Fewer mast cells | Abnormal nail plates |
| Fewer melanocytes | Fewer blood vessels | Fewer glands |
| Fewer Langerhans cells | Shortened capillary loops and abnormal nerve endings | — |
External factors, such as gravity, play a large role in the clinical appearance of the aging neck when taken in combination with the cellular changes mentioned earlier. The constant force of gravity exerts a mechanical pull on the already unsupported and lax skin. This mechanical pull exposes the changes related to fat depletion, fat accumulation, or herniation, as well as the changes related to loss of structural support from the deeper structures as the skin hangs and follows their contours.
The physiologic changes observed in skin aging affect management. Regardless of the aging process, surgical considerations should be directed at redraping of the skin over the underlying neck structures, which recreates the contour of the neck and CMA. The skin’s ability to conform to the new shape depends on the skin’s inherent pliability and texture, and often is related to its elastin and collagen content. In the setting of poor-quality or excess skin, excisional techniques are often necessary to allow redraping of the skin.
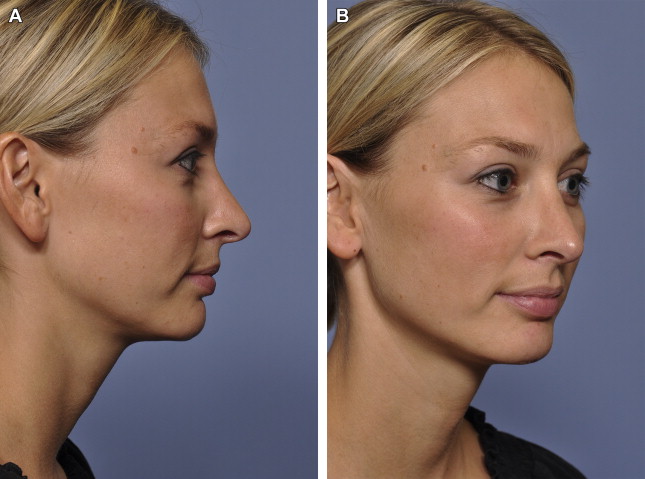
Good candidates for neck rejuvenation are patients who have moderate thickness to their skin, with minimal sun damage, and who have retained some hereditary elasticity to the skin appropriate for their chronologic age. However, some patients with smooth and nonphotodamaged skin may experience premature loss of skin elasticity, and may have an unsatisfactory duration of improvement. In addition, thick-skinned and overweight patients should not expect dramatic long-lasting results of their neck contouring procedures ( Fig. 2 ). The increased weight of the tissues, combined with gravitational forces, further limits the length of time in which the soft tissues remain firm and in an upward vector.

Cervical fascia
Superficial cervical fascia
The superficial cervical fascia is a thin layer of connective tissue between the dermis and the deep cervical fascia. This fascia covers the platysma muscle, as well as the cutaneous vessels, nerves, and lymphatics. A distinguishing feature is that this layer contains fat, which leads some clinicians to consider it to be a part of the subcutaneous tissue, and not true fascia.
Deep cervical fascia
The deep cervical fascia can be divided into 3 distinct layers with the superficial (investing) layer of the deep fascia covering the structures deep to the platysma, including the strap musculature, SCM, and trapezius muscles. The submandibular compartments are also enclosed by this fascial layer. The middle or visceral layer of the deep cervical fascia comes around to include the trachea, thyroid, and esophagus, whereas the deep layer envelopes the deep vascular (carotid, internal jugular vein) and neural structures of the neck, and includes the cervical vertebrae and vertebral musculature. Fascial laxity can occur, which is shown by changes in the superficial topography related to descent or exposure of the deep structures, including subplatysmal fat or ptosis of the submandibular glands.
Subcutaneous fat
The subcutaneous fat is found between the skin and the platysma muscle, and is also invested by the superficial cervical fascia. Subcutaneous fat varies in thickness according to the patient’s body habitus and weight, and is often a presenting concern for patients. There can be a variable distribution laterally along the surface of the platysma, with patients most often presenting with the largest volume of fat anteromedially. Fat is usually most abundant in the submental area, forming a triangular shape with the apex at the hyoid and base at the mandibular line. Often there is deep extension that is contiguous with the subplatysmal fat at the natural separation of the platysma muscles on their medial aspects. The amount of deep connection in this region depends on the degree of platysmal fibers decussating, which is variable and is discussed later. This fat does not have fibrous connections or septations, making it more easily sculpted through closed or open procedures including liposuction, as well as direct excision.
Within the same subcutaneous plane, patients can develop prominent melolabial folds or jowls descending from the face. Although they are not neck structures, their presence has a significant influence on the perception of a youthful and aesthetically pleasing neck. These structures should be considered in the preoperative analysis and in discussions with the patient, because they can be concomitantly addressed during neck rejuvenation. Most surgical alterations are targeted at reducing the bulk of fat within this area, attempting to develop a more acute CMA and establish an ideal contour. Techniques such as submental liposuction or direct excision are the most common techniques.
Lymphatics
The lymphatic drainage patterns within the neck are complex. Pan and colleagues, using lymphoscintigraphy, eloquently showed the lymphatic channels within the anterior cervical region and isolated 2 distinct layers of lymphatic vessels. The more superficial anterior neck vessels course between the dermis and the platysma, until ultimately penetrating the platysma medially to drain into the submental lymph node basin between the inferior border of the mandible and the thyroid notch. The channels seen draining to the submandibular lymph nodes course from the area just lateral to the platysma border. Deeper channels between the platysma and the deep cervical fascia can be identified draining into the anterior jugular lymph nodes, as well as the supraclavicular lymph nodes.
Superficial muscular aponeurotic system
Within the face, deep to the subcutaneous fat and superficial fascia, is the superficial muscular aponeurotic system (SMAS). Skoog first published descriptions on subfascial rhytidectomy, with Mitz and Peyronie later outlining a distinct anatomic subfascial layer and labeling it as the SMAS. These descriptions have led to the advancement and development of modern facelift techniques, with substantial lasting improvements established by addressing the SMAS layer as it relates to the neck and jawline as well. However, the literature shows significant differences of opinion in the patterns of the SMAS architecture in relation to the face and neck.
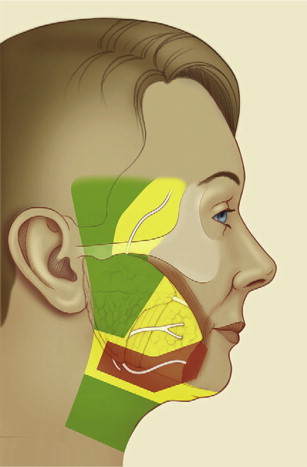
In general, the SMAS is 1 continuous and organized fibrous network within the face, contiguous with the platysma muscle as it transitions from the face into the neck. The SMAS is a multidimensional structure consisting of collagen and elastic fibers, fat cells, and muscle fibers. These fibrous extensions course from the periosteum or mimetic musculature through the subcutaneous layers connecting with the dermis. The complex attachments formed allow movement of all the layers as a single unit during rhytidectomy, which holds true for the SMAS junction with the platysma at the neck-face interface ( Fig. 3 ). The SMAS extends over the parotid gland laterally, superficial and distinct from the parotidomasseteric fascia. Following the SMAS from lateral to medial there is continuity with the zygomaticus major muscle and levator labii superioris alaeque nasi muscle, but anteriorly the SMAS becomes thin and sparse in the cheek area. There is debate regarding the role of sub-SMAS dissection as a modality in treating the prominent melolabial fold. Histologic studies have shown that, within the medial aspect of the face, there is a zone of fusion among the orbicularis oris, SMAS, and the buccinator muscle at the level of the modiolus. During rhytidectomy the SMAS flap is pulled, and the resulting tension is transmitted to the buccinator, orbicularis oris, and modiolus. This technique is associated with a pleasing result at the level of the melolabial fold, with a subsequent lateralization and elevation of the lower third of the melolabial fold and corner of the mouth. Superiorly distinct layers exist between the SMAS and the orbicularis oculi and the temporoparietal fascia, but their discussion is beyond the scope of this article.
Isolating the SMAS and dissecting within the sub-SMAS or deep plane has led to improvements in managing the neck-face interface, midface, and melolabial fold. Additional advantages of the deeper dissection, beyond of aesthetic results and longevity, are related to less subcutaneous dissection and risk of skin flap necrosis. However, there are increased risks related to injuring branches of the facial nerve when entering and dissecting within the sub-SMAS (deep) plane.
Aging of the neck secondary to significant jowling, midface descent, and melolabial prominences is common, and procedures addressing the SMAS and the neck-face interface are more appropriate, rather than an isolated neck procedure, which is likely to lead to suboptimal results.
Platysma
The platysma muscle is situated between the superficial and deep cervical fascia, and separates the subcutaneous fat from the deeper structures of the neck. The platysma originates from the superficial fascia overlying the superior aspect of the deltoid and pectoralis major muscle, with insertions at the mandible, depressor anguli oris, risorius, and mentalis muscles superiorly. The platysma is contiguous with the SMAS into the face with innervation from the cervical branch of the facial nerve. The paired, thin muscles course from inferolateral to superomedial, with a variable amount of interdigitation or decussation in the midline submental region. Cardoso de Castro further classified the patterns of decussation into 3 types. In type I, which is present in 75% of the population, there is limited decussation of the platysmal fibers, extending only 1 to 2 cm below the mandibular symphysis. Type II is present in 15% of the population, and has the platysma joining completely from the mandibular symphysis throughout the suprahyoid region, essentially behaving as a single muscle. Type III is the least common and is present in 10% of patients, with no decussation of the platysmal fibers at the midline ( Fig. 4 ).
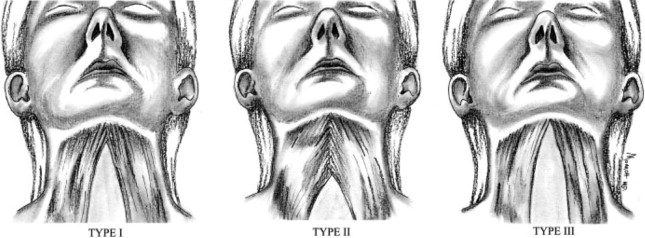
With aging, the platysma begins to lose tone and is pulled laterally, resulting in splaying of the medial fibers. In addition, there is attenuation of the deep retaining ligaments on the medial edge of the muscle contributing to loss of tone. This loss of tone allows the medial edges to descend, leading to development of platysmal bands, which can be exaggerated with contraction. Patients with minimal or no platysmal decussation can have interplatysmal fat in the submental region herniate between the medial edges, which is contiguous with the subplatysmal fat of the deep compartment, further contributing to the appearance of neck aging.
Aging can result in laxity, redundancy, and banding, which can be addressed with techniques such as submentoplasty or platysmaplasty. The goal is to resuspend and plicate the medial edges, and to excise redundant muscle and fat when necessary.
The deep compartment structures and surrounding neurovascular anatomy are at risk once the plane deep to the platysma is breeched. This anatomy includes branches of the external carotid artery and the jugular venous system as well as the cervical and marginal mandibular nerve branches of the facial nerve. The deeper neck compartment is discussed in detail later.
Subplatysmal deep compartment structures
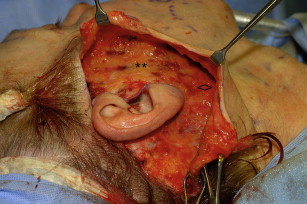
The subplatysmal compartment ( Fig. 5 ) defines the deep plane in neck rejuvenation, and the surgically relevant structures are discussed separately with specific neural and vascular structures mentioned when pertinent to an anatomic region.
Subplatysmal fat
With aging, there can be accumulation, depletion, as well as descent of the deep subplatysmal fat. Herniation through the interplatysmal region further contributes to the appearance of submental fullness and an obtuse CMA.
The deep fat can be broken down into the central, medial, and lateral compartments, with Rohrich and Pessa describing compartmentalization by color variations among the fat. The central compartment had a more discrete yellow color, whereas the medial and lateral compartments were pale, similar to buccal fat. The compartments cover the mylohyoid muscles forming a triangular-shaped adipose tissue mass that extends from the lateral third of the mandible to the thyroid cartilage.
When excising fat or liposculpting in this area, the surgeon must exercise caution when resecting centrally, because overaggressive resection may result in a hollow appearance to the neck. The surgeon should always keep in mind that the ideal appearance of the youthful neck maintains a rounded contour as opposed to a more skeletonized appearance. Dissection in this region carries a risk of injury to vascular structures, as well as the cervical and marginal mandibular branches of the facial nerve. In addition, the adipose tissue is well vascularized, with several perforators joining from the adjacent musculature. Vascularized level 1A lymphatic nodes are also encountered during surgical dissection. Fat excision in this region requires bipolar cauterization in order to obtain hemostasis and avoid hematoma formation.
Digastric muscles
The digastric muscles consist of 3 distinct parts, with the anterior belly originating from the mandibular fossa, and an intermediate tendon attaching to the body of the hyoid, which then joins the anterior belly with the posterior belly originating from the mastoid notch. The digastric muscles form the boundaries of the submandibular triangle. Separate nerves innervate the muscle bellies, with the anterior belly being innervated by the mandibular division of the trigeminal nerve via a branch of the nerve to the mylohyoid. An additional branch to the digastric muscle, slung from the facial nerve, innervates the posterior belly. The digastric muscles act to elevate the hyoid and also act as weak depressors of the mandible.
The actions of the digastric muscles on the hyoid are thought to contribute to formation of the CMA, and modifying the muscles for neck rejuvenation and contouring has been under debate, with conflicting practices published. Some techniques include plicating the muscles in the midline and shaving or excising hypertrophic components of the muscles, whereas others release the suprahyoid tendon aponeurosis connected to the hyoid to deepen the CMA. The authors do not advocate maneuvers intended to augment the digastric muscles.
Submandibular glands
The submandibular glands are located within the submandibular triangle, which is formed by the digastric muscle bellies with the inferior mandibular edge acting as the superior boundary. The glands are sheathed by the investing (superficial) layer of the deep cervical fascia. The mylohyoid muscle divides the gland into deep and superficial sections, with the deep portions of the gland resting over the hyoglossus muscle. The glands primarily function in the production of saliva, which additionally acts as a carrier for digestive enzymes and immunologic factors.
With aging, patients may develop ptosis or hypertrophy of the glands, with both contributing to contour irregularities in this region. Routine dissection or excision of the glands is controversial because of the inherent risk to the surrounding structures. The marginal mandibular nerve, lingual nerve, hypoglossal nerve, Wharton duct, facial artery, and facial vein are all at risk when manipulating the gland. In addition, neural injury, xerostomia, sialocele, or hematoma formation, possibly resulting in airway compromise, are all complications that surgeons should be aware of when counseling patients regarding partial or total gland resection. Simply suspending the platysma or the fascia overlying the glands to act as a sling can be advantageous in the treatment of ptotic glands without taking on substantial risk, and is the choice of most surgeons. The authors do not encourage the manipulation of the submandibular glands in neck rejuvenation.
SCM
The youthful neck is described as having a distinct outline of the anterior SCM border. The anatomy of the SCM defines the lateral boundary of the anterior triangle, which often is the extent of dissection needed in neck rejuvenation. The muscle originates at the manubrium sterni and medial one-third of the clavicle coursing posterosuperiorly to insert on the mastoid process and lateral one-half of the superior nuchal line. The superficial layer of the deep cervical fascia invests the SCM. The muscle is innervated by the spinal accessory nerve, and is involved in turning the head to the opposite side, as well as flexing the head.
Running deep to the platysma and along the lateral aspect of the SCM are the external jugular vein and great auricular nerve (discussed separately). The vein and nerve are separated from the SCM by the investing layer of the deep cervical fascia. This separation becomes surgically relevant when dissecting posterolaterally, because the surgeon should transition to a plane superficial to the fascia of the SCM to ensure that the elevation does not pass deep to the fascia or the SCM. A plane of dissection deep to the fascia could then allow injury to the external jugular vein and greater auricular nerve. The dissection is often difficult posteriorly because of the attenuation of the fat in this area and the stronger dermal attachments of the skin to the fascia and muscle.
Great auricular nerve
The great auricular nerve is formed by the second and third ventral primary rami of the cervical plexus, and ascends along the SCM to innervate the lobule, the skin behind the auricle, and skin overlying the parotid gland. The great auricular nerve is described as the most commonly injured nerve during rejuvenative procedures of the face and neck, which emphasizes the necessity of having a thorough understanding of its course to avoid injury. As described earlier, it runs parallel to the external jugular vein, crossing the SCM at the junction of the superior third and lower two-thirds of the muscle. This region is referred to as the Erb point, and the nerve divides approximately 6.0 to 6.5 cm inferior to the external auditory meatus into its auricular, mastoid, and facial branches.
The great auricular nerve can be preserved by exercising the precautions discussed earlier and maintaining a plane of dissection superficial to the fascia overlying the SCM.
Facial nerve
The cervical and marginal mandibular nerves are the most frequently encountered branches of the facial nerve during deep dissection within the neck. The cervical branch runs anteroinferiorly from its emergence at the caudal end of the parotid, coursing under the platysma as it innervates the muscle. Disruption of this nerve can lead to lip depressor dysfunction; however, this is rarely clinically relevant, and, if present, full recovery is expected.
The marginal mandibular nerve runs toward the mandibular angle in a subplatysmal plane before turning across the body of the mandible to supply the muscles of the lower lip and chin. The course of the nerve has been described as passing 1.2 to 1.3 cm, or less than 2 finger breadths, below the body of the mandible, with multiple branches encountered in most individuals. Owsley and Agarwal described anatomic danger zones for the cervical and mandibular branches in a subplatysmal plane. The zone is encompassed by the angle of the mandible laterally, the oral commissure medially, a line 1 cm above and parallel to the mandibular border cephalically, and a line 2 cm below the mandibular border as the caudal boundary ( Fig. 6 ). By maintaining deep dissection above the investing cervical fascia the surgeon can protect the branches of the marginal mandibular nerve, with reports of injury ranging from 0.5% to 2.6% during rejuvenative procedures.