Ambulatory Phlebectomy
 INTRODUCTION AND HISTORY
INTRODUCTION AND HISTORY
This safe, aesthetic, and effective operative technique developed by dermatologists enables the physician to remove nearly any incompetent vein after saphenofemoral and saphenopop-liteal reflux has been eliminated by endovenous ablation. The saphenofemoral junction (SFJ) and saphenopopliteal junction (SPJ) should never be treated by simple phlebectomy but require endovenous ablation. Large truncal veins can be removed by this method, together with their major tributaries, perforators, and reticular veins, including small reticular veins that supply annoying telangiectasias. A sharp phlebectomy hook enables the extraction of veins through skin incisions or needle punctures as small as 1 mm. A vein that has been removed by this method is gone permanently. The small size of the skin punctures usually results in minimal or no scar. In comparison with sclerotherapy, surgical extraction avoids the risks of intra-arterial injection, extravasation skin necrosis, and residual hyperpigmentation.
The discovery of foam sclerotherapy, however, has greatly reduced the need for ambulatory phlebectomy (AP).
Phlebectomy, first described by Cornelius Celsus (25 BC–45 AD), has been performed since ancient times. Phlebectomy hooks were in regular use as early as 1545, as illustrated in the Textbook of Surgery of W.H. Ryff, published in that year.1 Phlebectomy was forgotten during the Middle Ages, but the technique was later reinvented and (with later research) rediscovered in 1956 by Dr. Robert Muller, a Swiss dermatologic surgeon in private practice in Neuchâtel, Switzerland. Dr. Muller developed his method following modern surgical principles2,3 and taught it to a great number of disciples.4–6 A modest man, Muller always attributed the technique to his historic predecessor, calling his operation Celsus’ phlebectomy. In recent years, Muller’s technique has been further refined by a Swiss dermatologist, Dr. Albert-Adrien Ramelet.7
 INDICATIONS
INDICATIONS
The goals of AP depend on a patient’s particular clinical situation. Phlebectomy is rarely a definitive treatment that addresses both the root source of reflux and its visible expression, as endovenous ablation by radiofrequency (RF) and laser is required. Often used in conjunction with a definitive method to resolve saphenous reflux, phlebectomy can also be used when a painful varicose vein is removed in a patient unwilling or unable to consider a more extensive treatment. Sometimes, phlebectomy may be used to eradicate a short varicose segment or feeding vein that is responsible for a leg ulcer.4–8
Most types of primary and secondary varicose veins (truncal, reticular, and perforating) may be removed by AP, except when junctional saphenous incompetence is present. Veins most readily treated by phlebectomy include accessory saphenous veins of the thigh, pudendal veins, reticular varices in the popliteal fold or on the lateral thigh or leg, veins of the ankles, and the dorsal venous network of the foot. When patients do not want to wait for sclerotherapy results after endovenous ablation, AP may be performed on branch varicosities on the same day as endovenous ablation.
Phlebectomy can also be used in the immediate treatment of superficial phlebitis: a typical needle-puncture or incision is made, intravascular coagulum is expressed, and the vein segment is then extracted through the same incision, assuring definitive treatment and immediate relief of pain. The indications for phlebectomy are listed in Table 22-1.
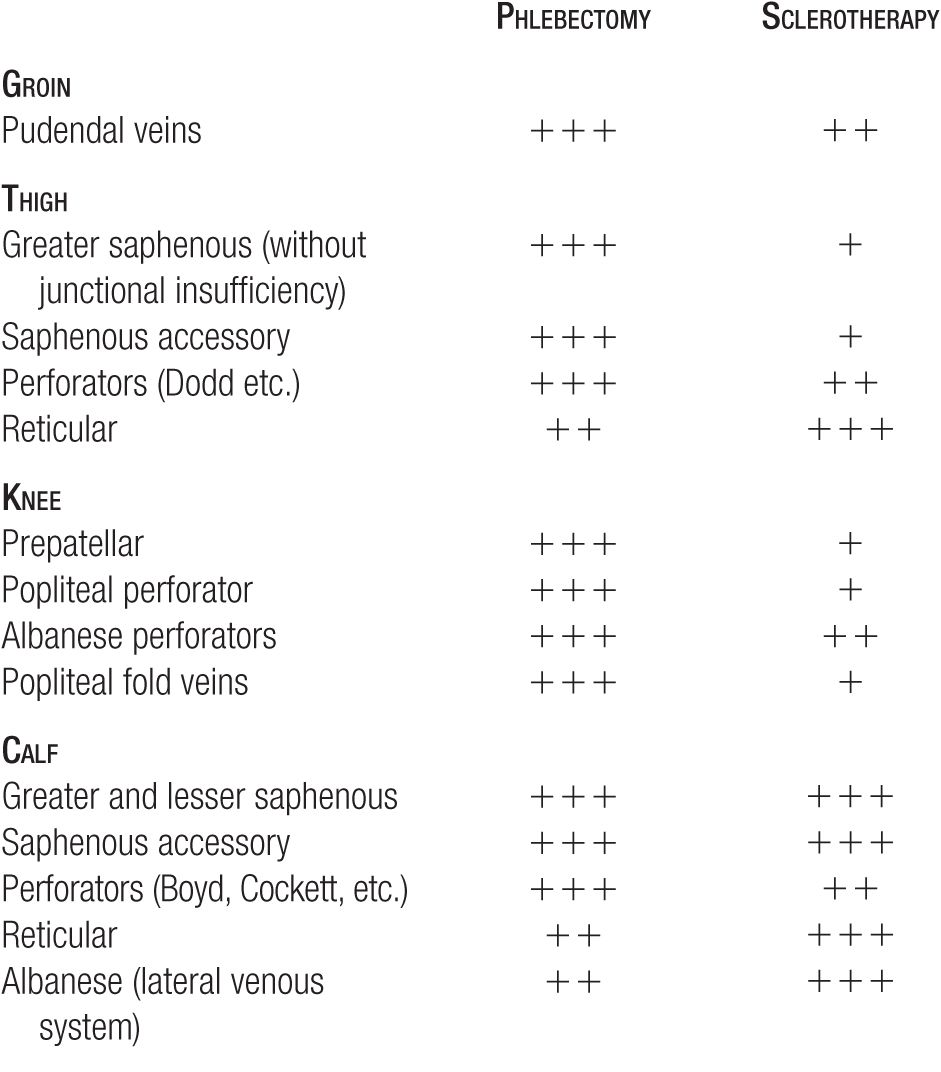
TABLE 22-1
Comparative Indications of Phlebectomy and Sclerotherapy (With ++++ Most Indicative and + Least Indicative)
Although any varicosity may be removed by hook extraction, inexperienced phlebologists should avoid the popliteal fold, the dorsum of the foot, and the prepatellar and pretibial areas because they often result in a higher incidence of side effects. Extraction is more difficult in these regions. Recurrent varicose veins after phlebitis or sclerotherapy also may be particularly difficult to extract because prior inflammation produces adhesions and local scar tissue.
Preoperative Evaluation of the Patient
A detailed general and phlebological examination is in order before AP in order to detect reflux that needs to be treated by endovenous ablation.4 Careful attention must be paid to the patient’s medical history and to the general health of the patient, including any contraindications to local anesthesia or to the surgical procedure itself. The integrity of the deep venous system and the proper function of the calf muscle pump should be assessed by Duplex ultrasound, and it is also essential to perform preoperative clinical and ultrasonographic detection and mapping of all types of varicosities and of their origin. To reiterate, important sources of reflux (such as the SFJ or SPJ) should be corrected before any effort is made to address end-branch disease by AP.
Operating Environment and Operative Materials
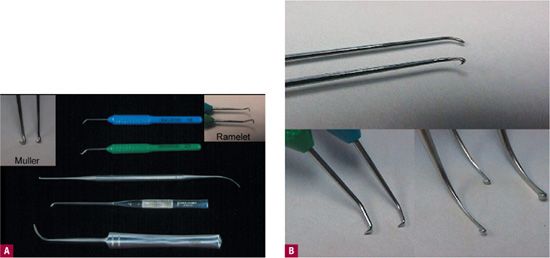
This ambulatory procedure requires an operating table, which rotates into a Trendelenberg position to exsanguinate veins by reduction of hydrostatic pressure. Good lighting is essential for visualization of markings and puncture sites. The presence of a circulating nurse or an assistant for this outpatient procedure is not quite mandatory but is highly suggested. Emergency equipment and supplies should be at close hand, although the likelihood of significant complications is reduced by the use of tumescent anesthesia. Tumescent anesthesia to elevate the vein and push it close to the surface for easier capture is essential as discussed later. Only a small number of surgical instruments are required to perform AP (see Table 22-2; Figure 22-1). A number 11 scalpel or an 18-gauge NoKor needle (Becton-Dickinson, Franklin Lakes, NJ) is used to perform microincisions. Tiny ophthalmological scalpels are available but offer few advantages to offset their expense. Phlebectomy hooks are used to pick up the vein and bring it through the incision, and mosquito forceps are used to grasp the veins as they are extracted.

![]() FIGURE 22-1 Typical ambulatory phlebectomy surgical tray.
FIGURE 22-1 Typical ambulatory phlebectomy surgical tray.
TABLE 22-2
Surgical Supplies for Phlebectomy
• Permanent or skin marking pen
• Antiseptic solution
• Disposable facemask, sterile gloves
• Local anesthetic, saline or Ringer solution, syringes, needles
• Resuscitation material
• Clamps, sterile gauzes
• Needle 18-gauge, NoKor needle, scalpel #11
• Mosquito forceps
• Hydrogen peroxide for postoperative washing of the leg
• Absorbant dressings
• Tubular dressings
• Elastic bandages
Phlebectomy Hooks
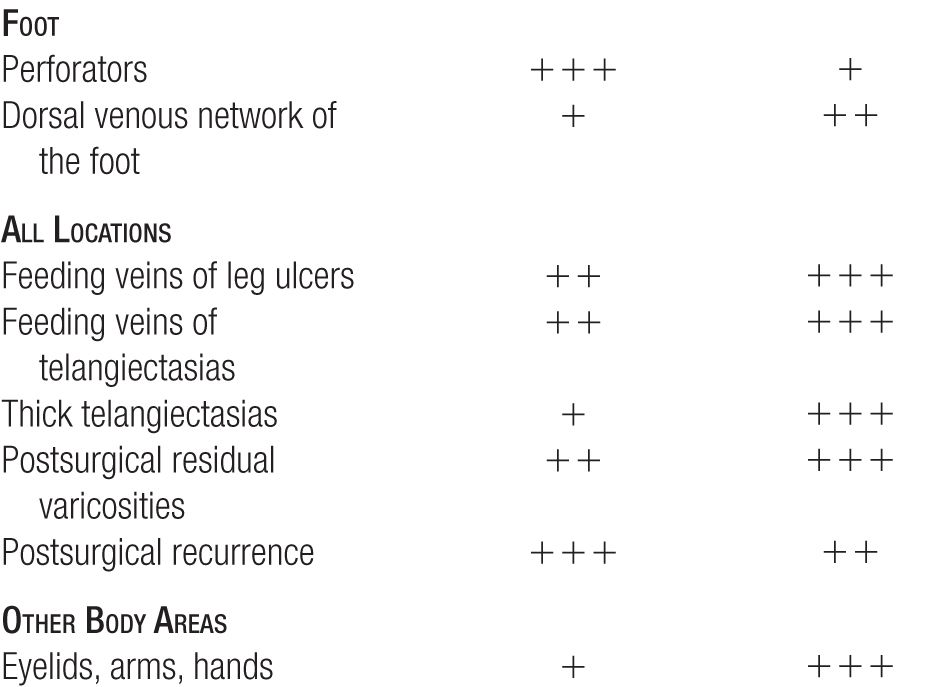
The ideal hook should have a comfortable grip to prevent fatigue and a sharp barbed end to snag the adventitia of the vein. Blunt hooks (boot-hook type) have been used by some surgeons but require a larger incision and a more aggressive venous dissection and are not recommended (Figure 22-2).
![]() FIGURE 22-2 A. The ideal hook should have a sharp harpoon to grip the adventitia of the vein, allowing its removal through a minimal incision. B. A larger incision is needed if using blunt hooks (boot-hook type). Adapted with permission from Ref. 4.
FIGURE 22-2 A. The ideal hook should have a sharp harpoon to grip the adventitia of the vein, allowing its removal through a minimal incision. B. A larger incision is needed if using blunt hooks (boot-hook type). Adapted with permission from Ref. 4.
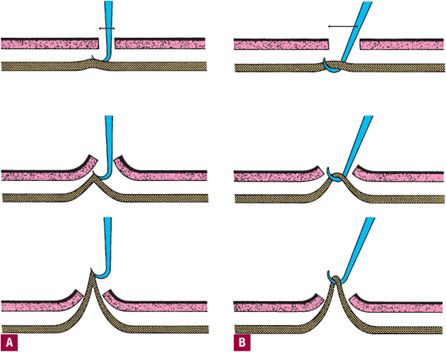
Two sizes of hook are enough to perform all types of phle-bectomies. A large hook with a thicker stem is indicated in extraction of larger truncal varicosities and perforators. A thinner device is necessary to remove smaller reticular venous networks. Several types of hooks are listed in Table 22-3 and shown in Figure 22-3. The choice of hook type is personal, although we often have all sets of hooks available on the surgical tray.
![]() FIGURE 22-3 A. Phlebectomy hooks. Top to bottom: Ramelet (blue and green), Varady, Muller-Padulli, Oesch. B. Detail of stems and hooks (from top to bottom) Muller, Ramelet, Oesch.
FIGURE 22-3 A. Phlebectomy hooks. Top to bottom: Ramelet (blue and green), Varady, Muller-Padulli, Oesch. B. Detail of stems and hooks (from top to bottom) Muller, Ramelet, Oesch.
TABLE 22-3
Phlebectomy Hooks: Set, Manufacturer, and Distributor
• Muller’s hooks (four sizes, also available for left hander)
Etablissements L. Padulli, Pont-Astier, F-6390 Lezoux, France Salzmann AG, Unterstrasse 52, CH-9001 St-Gallen, Switzerland Tel (+41) 71 228 43 13, Fax (+41) 71 228 43 10
Venosan North America Inc., 718 Industrial Park Ave., P.O. Box 4068, Asheboro, N.C. 27204-4068, USA. Fax 888.639.7642 Voice Mail 800 619 3705
• Oesch’s hooks (three sizes, also available for left hander)
Theodor Tüscher, Ziegelackerstrasse 11, CH-3027 Bern, Switzerland Salzmann AG, Unterstrasse 52, CH-9001 St-Gallen, Switzerland Tel (+41) 71 228 43 13, Fax (+41) 71 228 43 10
Venosan North America Inc., 718 Industrial Park Ave., P.O. Box 4068, Asheboro, N.C. 27204-4068, USA. Fax 888.639.7642 Voice Mail 800 619 3705
• Ramelet’s hooks (two sizes, also available for left hander)
Maillefer SA, CH-1338 Ballaigues, Switzerland Salzmann AG, Unterstrasse 52, CH-9001 St-Gallen, Switzerland Tel (+41) 71 228 43 13, Fax (+41) 71 228 43 10
Venosan North America Inc., 718 Industrial Park Ave., P.O. Box 4068, Asheboro, N.C. 27204-4068, USA. Fax 888.639.7642 Voice Mail 800 619 3705
• Varady’s hooks (four sizes, two phlebodissectors; may be used by both right- and left-handed)
Aesculap AG, D-7200 Tuttlingen, Germany
Tel (+49) 74 61 95 0, Fax (+49) 74 61 95 2600
MULLER Muller’s hook, available in four sizes, was the first modern hook device to be developed. It is based on the design of crochet hooks. It is believed that Muller grabbed his wife’s crochet hooks to perform the first procedure, although this is not substantiated. The grip is not very comfortable, but the stem and its angulation are suitable. The barb or harpoon portion at the tip is not sharp enough to penetrate through adventitia. This hook is best used to scoop under the entire vein and lift.
OESCH Oesch’s hook, available in three sizes, is characterized by a massive grip, although one cannot roll it between the fingers. The “barb” or spike end is of relative help for “harpooning” the vein and cannot be modified. This sensible device, highly valued by many surgeons, is very effective for removing larger veins, but less efficacious for reticular veins.
VARADY Varady’s phlebextractor combines two devices on one stem. The vein is first dissected with the spatula end, and then grasped with the hook end of the vein extractor. The device must be frequently reversed in the operator’s hand. Because the hook end is blunt, harpooning of the adventitia is not possible. The spatula-dissector portion has little advantage except in patients with very fibrous peri-venous tissue such as in frequent runners. Some believe that blunt dissection injures the surrounding tissues and does not expedite the procedure or improve the result, but there is no consensus.
RAMELET Ramelet’s hook9 was developed to address perceived shortcomings and fill voids of other existing instruments. The instrument is very economically priced compared with other hooks, yet offers several advantages. Ramelet hooks are produced in two sizes that are easily distinguishable by the different color of each handle. A smaller, fine hook is designed to remove reticular or medium-sized truncal varicose veins, while a larger hook with a thicker stem is useful for extracting large truncal and perforating veins. The hook includes a plastic-coated aluminum handle and a stainless steel stem, ensuring strength and durability. The grip is easy to grasp, well adapted to the operator’s hand, and does not slip or risk tearing the surgeon’s gloves. The cylindrical shape of the grip permits a gentle rolling of the hook between the fingers, diminishing the amount of rotation of the wrists and minimizing wrist and hand stress during the procedure. The shape of the handle also does not cause fatigue during long operations. The hook stem is short, allowing precise and close work as well as vigorous traction. The hook angulation facilitates vein dissection and anchoring. The sharp barb allows one to grasp the vein by the perivenous collagen bundles and tunica externa (Figure 22-4), limiting the damage to the surrounding tissues and lymphatics. This is the hook of choice for beginners and to start the phlebectomy after the initial puncture.

![]() FIGURE 22-4 Ramelet hook with the sharp harpoon grips the vein by the perivenous collagen bundles and tunica externa, limiting the damage to the surrounding tissues and lymphatics.
FIGURE 22-4 Ramelet hook with the sharp harpoon grips the vein by the perivenous collagen bundles and tunica externa, limiting the damage to the surrounding tissues and lymphatics.
Patient Preparation and Tumescent Anesthesia
Premedication is rarely required and should be avoided as much as possible, as it may hinder immediate postoperative walking, which is the best means of prevention of potential complications such as deep venous thrombosis. Varicose veins are carefully marked with an indelible marking pen on the standing patient and once again when the patient is supine. As the vein collapses when the patient becomes supine, the area is marked with transillumination (Figure 22-5). The transillumination technique is invaluable in marking pre-phlebecomy, as veins may shift as much as 6 mm when the patient moves from a standing position to a supine position.10 Cutaneous transillumination is also helpful in locating less obvious reticular veins. Local anesthesia is injected after routine skin disinfection with a surgical scrub solution (Figure 22-6A). The recommended anesthetic for phlebectomy is perivenous infiltration with tumescent anesthesia.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


