Chapter 16 Alternative wound coverings
![]() Access the complete reference list online at http://www.expertconsult.com
Access the complete reference list online at http://www.expertconsult.com
![]() IN THIS CHAPTER
IN THIS CHAPTER ![]() PowerPoint Presentation Online
PowerPoint Presentation Online
Introduction
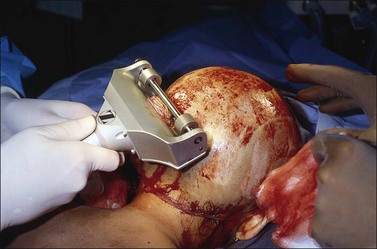
The skin envelope evolved to maintain a tightly controlled internal environment. When severely damaged, preservation of this critical milieu becomes impossible, leading to major physiologic derangements. The central component of burn care is to expeditiously replace damaged areas of the skin to restore physiologic homeostasis. An increasingly effective group of temporary and permanent alternative wound coverings are available to the burn team to help in this regard. Although these membranes are becoming increasingly capable, the definitive replacement material of choice remains the patient’s own skin (Fig. 16.1).
Physiologic considerations
Structure and function of the skin
Skin, the body’s largest organ, is incredibly complex. Functionally there are two layers with a highly specialized and effective bonding mechanism. Numerous appendages traverse the skin and a rich and reactive capillary network provides nutrient flow while controlling temperature. The epidermis, consisting of the strata basale, spinosum, granulosum, and corneum, provides a vapor and bacterial barrier. The dermis provides strength and elasticity. The thin epidermal layer is constantly refreshing itself from its basal layer, with new keratinocytes undergoing terminal differentiation over approximately 4 weeks to anuclear keratin-filled cells that make up the stratum corneum, which provides much of the barrier function of the epidermis. The basal layer of the epidermis is firmly attached to the dermis by a complex bonding mechanism containing collagen types IV and VII. When this bond fails, serious morbidity results, as demonstrated by the disease processes of toxic epidermal necrolysis1 and epidermolysis bullosa (Fig. 16.2).2
Consequences of loss of barrier function
Although it is an imperfect replacement, autologous split-thickness skin is closest to being the ideal skin substitute (Box 16.1). Because of the paucity of autologous donor skin available in patients with massive burn injuries, both the short-term and long-term problems of skin loss must be solved by alternative wound closure materials. Alternative materials can be used for either wound coverage which will be temporary or for permanent wound closure. Allogenic (cadaver) skin has been the most widely used alternative wound closure material. However, there are other choices. This is an exciting and fast-moving area which may profoundly change the care of patients with serious burns. The objective of this chapter is to review the currently available alternative skin closure materials, both temporary and permanent.
Temporary skin substitutes
• as a dressing on donor sites to facilitate pain control and epithelialization from skin appendages;
• as a dressing on clean superficial wounds for the same reasons;
• to provide temporary physiologic closure of deep dermal and full-thickness wounds after excision while awaiting autografting or healing of underlying widely meshed autografts; and
Human allograft
Human allograft is generally used as a split-thickness graft after being procured from organ donors. When used in a viable fresh or cryopreserved state, it vascularizes and remains the ‘gold standard’ of temporary wound closures.3–5 It can be refrigerated for up to 7 days, but can be stored for extended periods when cryopreserved. It is also used in a nonviable state after preservation in glycerol or after lyophilization; however, most existing data describe results when it is used in a viable state. Viable split-thickness allograft provides durable biologic cover until it is rejected by the host, usually within 3 or 4 weeks. Prolongation of allograft survival, through the use of antirejection drugs, has been advocated,6 but is not generally practiced for fear that antirejection drugs will increase the risk of infection.7
Human skin allografts are generally placed into frozen storage awaiting the return of numerous laboratory tests allowing one to safely exclude the possibility of viral disease transmission. When modern screening techniques are followed, the risk of viral disease transmission is exceedingly small. Allograft is also effectively used in combination with meshed autograft in patients with large burns, the interstices of the meshed graft being immediately closed by the overlying unexpanded allograft, possibly reducing metabolic stress and local wound inflammation (Fig. 16.3).
Human amnion
Human amniotic membrane is used in many parts of the world as a temporary dressing for clean superficial wounds such as partial-thickness burns, donor sites, and freshly excised burns awaiting donor site availability.8,9 Amniotic membrane is generally procured fresh and used after brief refrigerated storage.10,11 It can also be used in a nonviable state after preservation with glycerol. It has been treated with silver to facilitate control of bacterial overgrowth.12 Amnion does not vascularize but still can provide effective temporary wound closure.13 The principal concern with amnion is the difficulty in screening the material for viral diseases unless preservation methods can eliminate potential viral contamination. Without the ability to screen the material in this way, the risks of disease transmission must be balanced against the clinical need and the known characteristics of the donor.
Allogenic epithelial sheets
In many centers, particularly in Europe, sheets of allogenic and autogenous epithelium are used to dress partial-thickness wounds or to cover the interstices of meshed split-thickness autografts.14,15 These are generally applied as thin sheets placed on a gauze carrier for ease of handling. Cell suspensions in fibrin sealant have also been trailed. The concept is that the sheets will both prevent desiccation of underlying wounds and that the release of unknown growth-stimulating substances by the cells as they die will stimulate native wound healing.16 The concept is attractive, but controlled data are not available, particularly as regards any impact on long-term outcomes.
Xenografts
Although various animal skins have been used for many years to provide temporary coverage of wounds,17 only porcine xenograft is widely used today (Fig. 16.4). It has been used as primary temporary cover and as a scaffold for dermal regeneration efforts.18 Porcine xenograft is commonly distributed as a reconstituted product consisting of homogenized porcine dermis which is fashioned into sheets and meshed.19 Split-thickness porcine skin is also used fresh, after brief refrigeration, after cryopreservation, or after glycerol preservation. It effectively provides temporary coverage of clean wounds such as superficial second-degree burns and donor sites20 and has been used in patients with toxic epidermal necrolysis.1,21 Porcine xenograft has been combined with silver to suppress wound colonization.22,23 Porcine xenograft does not vascularize, but it will adhere to a clean superficial wound and can provide excellent pain control while the underlying wound heals.
Synthetic membranes
A number of semipermeable membrane dressings can provide a vapor and bacterial barrier and control pain while the underlying superficial wound or donor sites heal. These typically consist of a single semipermeable layer that provides a mechanical barrier to bacteria and has physiologic vapor transmission characteristics.24 Biobrane™ (Dow-Hickham, Sugarland, TX) is a two-layer membrane constructed of an inner layer of nylon mesh that allows fibrovascular ingrowth and an outer layer of silastic that serves as a vapor and bacterial barrier.25 It is widely used to provide temporary closure of superficial burns and donor sites.26 All synthetic membranes are occlusive and can foster infection if placed over contaminated wounds, especially in the presence of necrotic tissue.27 Appropriate monitoring is essential to their proper use.
Hydrocolloid dressings are generally designed with a three-layer structure: a porous, gently adherent inner layer; a methyl cellulose absorbent middle layer; and a semipermeable outer layer. They foster a moist wound environment while absorbing exudate. A moist wound environment has been found to favor wound healing.28 A variety of pastes and powders made from hydrocolloid materials are also widely available. These can be applied to superficial or deeper chronic wounds to absorb wound exudate while maintaining a moist wound environment.
Hydrofiber mats absorb wound exudate and have been used as temporary wound membranes. When combined with ionic silver (Aquacel-Ag, ConvaTec, Chester, UK), additional antimicrobial activity is seen. This membrane has been used successfully in some burn programs as an adjunct in the management of partial-thickness burns and donor sites.29