Alopecias and Hair Restoration in Women
Valerie D. Callender
Cherie M. Young
Alopecia is a common cosmetic concern in women of color. Epidemiological data addressing the true incidence of alopecia in women of color is lacking, but dermatologic practices with high proportional numbers of ethnic patients have found that there are increasing numbers of female patients with alopecia presenting for treatment.1 Halder et al. reported alopecias as the fifth most common dermatosis seen in a dermatologic private practice that treats mainly African American patients.2 Although the most common form of alopecia in women is female pattern hair loss (FPHL), chemical alopecia and traction alopecia were identified as the top forms of hair loss in this study of patients with darker skin types.
There are several causes of hair loss in women of color (Table 30-1). The unique characteristics of black hair, along with the plethora of hairstyles and hair-grooming practices, have been associated with the traumatic forms of alopecia; however, the exact etiology has not been proven in the majority of cases.1 This chapter will focus mainly on the causes of alopecia that are most often treated by hair restoration in black women: FPHL, traction alopecia, and central centrifugal cicatricial alopecia (CCCA). In the majority of cases, a tetrad of therapeutic options for these patients is critical for success and combines medical therapy, cosmetic camouflage, surgical correction, and patient education on hair grooming. Hair restoration, a popular procedure performed primarily in men, has shown to be a viable option for hair loss in women.3 Although the surgical technique of hair restoration is similar in men and in women, there are special considerations for women of color that will be discussed.
Female Pattern Hair Loss
(FPHL), also known as androgenetic alopecia (AGA), is the most common form of alopecia in women (Fig. 30-1). The true incidence varies from 6% to 25% of women before the age of 50.4 The incidence of frontoparietal hair loss has been reported to be 13% in premenopausal women compared with 37% in postmenopausal women.4
The emotional and psychological reaction to hair loss in women is far greater than in men.5,6,7 A study of 58 women with FPHL demonstrated negative self-esteem in 75% of the cases and social problems in 50%.8 The quality of life in women with hair loss was as low as with psoriasis patients. Although there are no published clinical studies involving the impact of hair loss in women of color, similar quality-of-life issues may be present and, in some cases, even more severe.
The age at onset for FPHL peaks in the 20s and 40s, perimenopausally, or at times of hormonal change.9 AGA is caused by the susceptibility of hair follicles to miniaturize in the presence of androgens.9 There is limited data on the genetics of this type of hair loss, but proposed theories include autosomal dominance with incomplete penetrance and polygenic inheritance.9 FPHL is a nonscarring type of alopecia and clinically appears as diffuse thinning over the frontoparietal scalp with preservation of the frontal hairline. The Ludwig pattern of hair loss is used to stage the extent of disease in patients with FPHL, with stage 1 consisting of mild hair loss and stage 3 consisting of extensive hair loss.10
Histologically, FPHL is characterized by follicular miniaturization, a decreased anagen-to-telogen ratio, and a decreased follicular density in long-standing cases.9 Perifollicular inflammation and dermal fibrosis may be observed and are associated with a potentially worse prognosis.9
The most common treatment for FPHL is topical minoxidil 2% solution twice daily. Minoxidil is a potassium channel opener and vasodilator, but its mechanism of action on hair growth is unknown. In a 32-week clinical study in 550 women, the minoxidil-treated women had significantly higher hair counts than the women who received placebo.11,12 In another 32-week study, hair weight was the primary end point. The average hair weight increased by 42.5% in the minoxidil group as compared with 1.9% in the placebo group.13 Another study compared the use of minoxidil 2% solution with minoxidil 5% in the treatment of FPHL for 48 weeks. In this study, the use of minoxidil 5% was superior to minoxidil 2% using nonvellus hair counts and investigator and patient assessments of hair growth. An increased occurrence of side
effects, such as pruritus, local irritation, and hypertrichosis, was also observed in those using minoxidil 5% when compared with the minoxidil 2% and placebo groups.14 Topical minoxidil solution is applied twice daily to the scalp; topical minoxidil 2% in petrolatum (rather than the solution) can be used in black female patients with natural hairstyles or thermally straightened hair.1 Other treatments for FPHL include oral antiandrogens, such as spironolactone, cyproterone, and oral contraceptives. These are used mainly in premenopausal women. Oral finasteride has also been used as treatment for patients with FPHL, particularly in Europe, with some success.15
effects, such as pruritus, local irritation, and hypertrichosis, was also observed in those using minoxidil 5% when compared with the minoxidil 2% and placebo groups.14 Topical minoxidil solution is applied twice daily to the scalp; topical minoxidil 2% in petrolatum (rather than the solution) can be used in black female patients with natural hairstyles or thermally straightened hair.1 Other treatments for FPHL include oral antiandrogens, such as spironolactone, cyproterone, and oral contraceptives. These are used mainly in premenopausal women. Oral finasteride has also been used as treatment for patients with FPHL, particularly in Europe, with some success.15
Table 30-1 Causes of alopecia in black women | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Women with Ludwig stages 1 and 2 are excellent candidates for hair transplantation, especially when combined with minoxidil.16 Those patients with Ludwig stage 3 are generally not considered for surgical correction of their hair loss because of insufficient hair density in the donor area of the scalp.17 Some authors report that all patients with FPHL are candidates as long as the goal of increased density is realistic and there is sufficient donor area to perform one to three hair transplant sessions of 800 to 1,200 grafts each.3
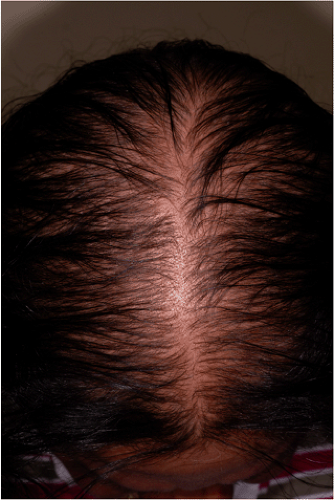 Figure 30-1 Female pattern hair loss (also known as androgenetic alopecia) is the most common form of alopecia in women. |
Traction Alopecia
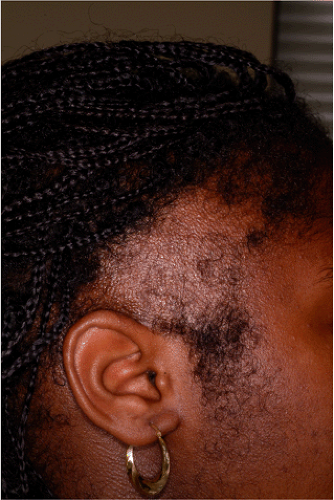
Traction alopecia is a common form of hair loss in black women (Fig. 30-2). This form of traumatic alopecia has been associated with long term use of ponytails,18 hair rollers,19 tight braids,20,21,22 and hair weaves.22 The etiology
of traction alopecia is thought to be secondary to chronic tension or pulling of the hair, leading to a mechanical loosening of the hairs from the hair follicle. A perifolliculitis occurs, and eventually a permanent alopecia develops.23 Clinically, there is a symmetrical loss of hair in the temporal areas, anterior and superior to the ears, which, in severe cases, extends along the frontal and occipital hairlines (ophiasis pattern). Characteristically, vellus hairs are usually spared, and broken hairs are seen scattered within the areas of hair loss.24
of traction alopecia is thought to be secondary to chronic tension or pulling of the hair, leading to a mechanical loosening of the hairs from the hair follicle. A perifolliculitis occurs, and eventually a permanent alopecia develops.23 Clinically, there is a symmetrical loss of hair in the temporal areas, anterior and superior to the ears, which, in severe cases, extends along the frontal and occipital hairlines (ophiasis pattern). Characteristically, vellus hairs are usually spared, and broken hairs are seen scattered within the areas of hair loss.24
Histologically, in the early stages of traction alopecia, the most prominent finding is increased number of terminal catagen and/or telogen hairs.25 If the telogen hairs are increased in number, this is referred to as fibrous “streamers”.25 In the end stage of traction alopecia, there is a marked decrease in the total number of follicles and terminal follicles with retention of vellus hairs.25 There are also fibrous tracts found at the sites of former follicles, normal dermal collagen, intact sebaceous glands, and no significant inflammation.25
Traction alopecia can be prevented if diagnosed early.1,26 Discontinuance of any hairstyle that produces tension on the hair is the most important step in the treatment of traction alopecia. Medical management includes topical and oral antibiotics, topical and intralesional corticosteroids, and topical minoxidil.1,26 Surgical correction with hair transplantation by punch grafting and/or flap rotation24 and minigrafting, micrografting, and follicular-unit transplantation (FUT) has been reported to be successful.1,27
Central Centrifugal Cicatricial Alopecia
CCCA is an inflammatory scarring form of alopecia that is commonly seen in black women (Fig. 30-3). It has been referred to as hot-comb alopecia,28 chemical alopecia,21 pseudopelade,29 chemically induced cosmetic alopecia,30 follicular degeneration syndrome,31 and, more recently, CCCA.32 The North American Hair Research Society–sponsored workshop on cicatricial alopecia has further classified CCCA and other forms of cicatricial alopecias based on their clinical and pathologic findings.33 This classification system was developed to guide the clinician and researcher on treatment monitoring as well as to facilitate clinical trials on epidemiology, pathophysiology, and therapeutic effectiveness in patients with scarring alopecia.
Although the etiology of CCCA remains unclear, the association of hot combs or chemical relaxers may contribute to CCCA in black women, and the end result is permanent destruction of the hair follicles. The course of CCCA is progressive and can be divided into early (inflammatory) and late (scarring) stages of disease. Initially, the scalp may appear normal clinically, may exhibit circular patches of broken short hairs (author’s personal observation), or may exhibit partial hair loss involving the crown and/or vertex measuring only a few centimeters in diameter.34 The affected area gradually increases in size centrifugally. At any stage of the disease, patients may experience pruritus and/or tenderness of the scalp. Erythema, scaling, and occasional pustules may also be noted clinically. Characteristically, late disease presents with lack of follicular ostia and irreversible alopecia.35
 Figure 30-3 Central centrifugal cicatricial alopecia (CCCA) is an inflammatory scarring of alopecia that is commonly seen in black women. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree