Vascular Surgery in Darker Racial Ethnic Groups
Parrish 0 Sadeghi
This chapter will focus on modalities used to treat visible lower-extremity venous diseases, such as spider veins and varicose veins. There is an absolute paucity of published data regarding the treatment of spider veins and varicosities in darker racial ethnic groups. Treatment modalities using sclerosing agents are similar in lighter and darker skin types.
Venous disease of the legs encompasses a variety of conditions affecting the veins, including visible disease—such as spider veins, varicose veins, trophic changes, or edema—and functional disease—such as reflux, obstruction, phlebitis, or thrombosis. Venous disease in the legs occurs very commonly in the general population of industrialized countries and is a substantial source of morbidity in the United States and the Western world.1,2 Many patients seek leg vein treatment for symptomatic relief, whereas others find varicose veins cosmetically unsightly and seek treatment for that reason. According to a 2005 survey by the American Society of Dermatologic Surgery, the eradication of leg veins was one of the most commonly reported procedures by dermasurgeons in the United States.3
Epidemiology and Risk Factors
Estimates of the prevalence of venous disease are varied. Although it is difficult to estimate the overall prevalence of venous disease worldwide, a large U.S. survey, the Framingham study, reported that 27% of the American adult population had some form of venous disease in their legs.4 There is evidence that geographic location and race can influence susceptibility to superficial venous disease. People living in North American and Western European countries seem to be at a greater risk for venous disease as compared with those who live in South America, India, the Far East, or Africa.1 Venous disease is less prevalent in African Americans, Hispanics, and Asians.5 It has been suggested that the low prevalence of varicose veins in Africans (1%–2%) may be associated with the higher number of venous valves in their lower extremities as compared with Caucasians.6
To date, most studies have investigated factors that influence susceptibility to superficial venous disease. The data suggest that female sex,7 increased age,8 pregnancy,9 and oral contraceptive use10 are risk factors for varicose veins. There are also reports that chronic venous disease is higher in those whose job involves prolonged standing and those working under conditions of high temperature and humidity.11,12 Although some studies have suggested that obesity is associated with varicose veins, a number of studies have not confirmed this finding.1,13 There is no evidence that there is a strong genetic component to these disorders.14
Clinical Presentation
The clinical presentation of patients with venous disease of the lower extremities can be variable. Visible venous disease can manifest as telangiectasias or varicose veins, whereas functional disease involves reflux or obstruction of the veins. Leg swelling has been shown to be the most specific predictor of visible and functional leg vein disease.15 Ankle edema is usually the first manifestation of chronic venous insufficiency (CVI) and can lead to venous stasis. Stasis dermatitis and pigmentary changes, resulting from extravasation of erythrocytes and hemosiderin deposition, are common sequelae of long-standing venous stasis. Recurrent or chronic cellulitis, ulceration, scarring, and malignant degeneration are more serious complications of leg vein disease.16
Many patients with visible venous disease have minimal to no symptoms, whereas others may report localized pain, burning, itching, or more generalized leg fatigue, aching, and swelling. Symptomatic varicose veins occur in approximately 15% of men and 25% of women;1 women are more likely to report symptoms than men.15,17,18
Anatomy
In the leg there are two systems of veins: the deep and the superficial. The deep venous system consists of veins that lie within the muscular system. The superficial venous
system has two main veins: the greater saphenous vein (also known as the long saphenous vein) and the lesser saphenous vein (also referred to as the short saphenous vein). The greater saphenous vein (GSV) originates at the medial side of the foot and runs superiorly along the medial aspect of the leg to empty into the femoral vein at the saphenofemoral junction. The lesser saphenous vein starts at the lateral aspect of the foot and runs along the back of the calf and typically joins the popliteal vein at the saphenopopliteal junction. The deep and superficial veins are connected via perforator veins. Veins in the same fascial plane are often interconnected by a complex of communicating veins.
system has two main veins: the greater saphenous vein (also known as the long saphenous vein) and the lesser saphenous vein (also referred to as the short saphenous vein). The greater saphenous vein (GSV) originates at the medial side of the foot and runs superiorly along the medial aspect of the leg to empty into the femoral vein at the saphenofemoral junction. The lesser saphenous vein starts at the lateral aspect of the foot and runs along the back of the calf and typically joins the popliteal vein at the saphenopopliteal junction. The deep and superficial veins are connected via perforator veins. Veins in the same fascial plane are often interconnected by a complex of communicating veins.
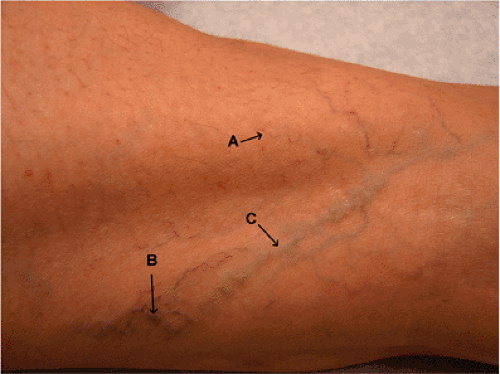 Figure 29-1 Telangiectasia (A), venulectasias (B), reticular veins (C), and varicose veins of the lower extremities. |
Venous valves are a significant part of the venous system, maintaining the blood’s upward flow. Valves are present between the superficial and deep systems at the saphenofemoral and saphenopopliteal junctions. More valves are located below the knee than above. Elevated venous pressure is most often the result of venous insufficiency with reflux through incompetent valves in the deep or superficial veins. Telangiectasias, venulectasias, reticular veins, and varicose veins represent the undesirable pathways by which venous blood refluxes back into the congested extremity (Fig. 29-1). Although most large varices arise from tributaries of incompetent truncal vessels, failed perforating veins or connecting veins can also give rise to independent varices in the greater saphenous distribution without involving the saphenous system itself.
Approach to a Patient with Varicose Veins
History and physical examination are important in the evaluation of patients with venous disease. Risk factors such as prior pregnancies, use of oral contraceptives, and history of superficial thrombophlebitis or deep venous thrombosis should be noted. A careful physical examination should be done to determine the nature, extent, and location of varicose veins. Photographs of the affected areas are helpful for tracking disease progression and response to treatment. Laboratory workup to evaluate hypercoagulability or bleeding risks may be appropriate if indicated by the patient’s history.
Extensive diagnostic imaging is often unnecessary before treating spider veins and venulectasias, however, for largely dilated (>4 mm) vessels or for more severe cases, imaging modalities are available and should be used to evaluate and determine the extent of the venous disease. Duplex ultrasound has become the most widely used mode of investigation for both arterial and venous disease. This noninvasive and inexpensive technique enables the physician to evaluate competence of the deep and superficial venous valves as well as the competence of the saphenofemoral and saphenopopliteal junctions. Photoplethysmography can be used to measure venous refilling time and distinguish between deep and superficial venous insufficiency.
Compression Therapy
Graded compression stockings are often prescribed for patients with varicose veins as a method of relieving symptoms. They may be prescribed either as a definitive treatment or temporarily after varicose vein treatment.19 Compression stockings are designed to provide a pressure gradient that is greatest at the ankle and decreases proximally, mimicking the normal hydrostatic pressures of the lower extremity.20 Therapy with compression stockings has been shown to improve venolymphatic drainage substantially in both healthy patients and those suffering from CVI.21 Most clinicians advocate the use of compression stockings after sclerotherapy; however, there are variations in the suggested duration of use, ranging from 48 hours to several weeks.
Sclerotherapy
For treatment of leg veins less than 4 mm in diameter, sclerotherapy has been considered to be the gold standard.22 Sclerotherapy involves the direct injection of a sclerosing agent into a visible vein or telangiectasia. The solutions are designed to either irritate, dehydrate, change the surface tension of, or completely destroy the venous endothelial cells, thereby creating a thrombus. Ultimately, the vein is permanently occluded as the thrombus is replaced by fibrosis. There are three types of sclerosant agents: osmotic agents, detergents, and chemical irritants. The most commonly used sclerosants in the United States are hypertonic saline, sodium tetradecyl sulfate, and polidocanol.
Osmotic agents
Osmotic agents, such as hypertonic saline or hypertonic saline with dextrose, cause thrombus formation through dehydration and disruption of the cell walls of endothelial cells and erythrocytes. Osmotic agents are best for treatment of smaller vessels and for low-flow vessels, because rapid dilution can diminish the efficacy of the sclerosant.23 Severe muscle cramping as a result of transient hyperosmolality induced by hypertonic saline may be experienced.23 A more serious potential complication—cutaneous ulceration and necrosis—can arise if these agents extravasate into surrounding tissue. One advantage of these agents is that there is a very low risk of allergenicity.
Hypertonic saline is used as a 23.4% solution of sodium chloride, and at this concentration, it can be directly injected into reticular veins and larger vessels.24 For treatment of smaller vessels, it can be diluted with either normal saline or bacteriostatic water to achieve a concentration of 11.7% solution.25 In very fine vessels or in vessels near the ankle, a solution of approximately 6% sodium chloride may be more appropriate.26
A solution composed of 10% saline, 5% dextrose, propylene glycol, and phenethyl alcohol is manufactured under the brand name Sclerodex. This product is not FDA approved in the United States, although it is approved in Canada. It has limited use because it can only be used in very small vessels (<1 mm in diameter).26 It is associated with a decreased incidence of muscle cramping, presumably because of the lower percentage of saline, but has an increased risk of pigmentation, allergenicity, and necrosis. The manufacturer recommends a maximum volume of 1 cc at any injection site, with a total per session of no more than 10 cc.
Detergents
Detergent sclerosants produce vascular injury by interfering with cell surface lipids and altering the surface tension around endothelial cells. This results in irritation of the vein intimal endothelium, endothelial cell death,27 and subsequent thrombus formation and vein fibrosis.
Sodium tetradecyl sulfate (STS), a long-chain fatty acid salt with strong detergent properties, is FDA approved for the treatment of varicose veins. Concentrations of 0.1% to 0.3% are commonly used for the treatment of telangiectatic veins from 0.2 to 1.0 mm in diameter, 0.5% to 1% for treatment of uncomplicated varicose veins that are 2 to 4 mm in diameter, and 1.5% to 3% for the treatment of larger varicose veins.28 At high concentrations, it is associated with an increased incidence of postsclerosing hyperpigmentation and cutaneous necrosis. Allergic reactions to STS have been reported and include generalized urticaria, bronchospasm, and anaphylactic shock.29
Polidocanol (POL), a synthetic fatty alcohol with detergent activity, is currently not FDA approved for use in the United States, but is used extensively in Australia and Europe. In a 2-year Australian study of the efficacy and safety of POL, POL appeared to be superior to STS and hypertonic saline in terms of efficacy and had fewer associated side effects.30 Other studies have shown comparable results between POL and STS28,31 or POL and hypertonic saline.32 POL has been used as an anesthetic and is therefore painless upon injection and well tolerated by patients for that reason.27




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








