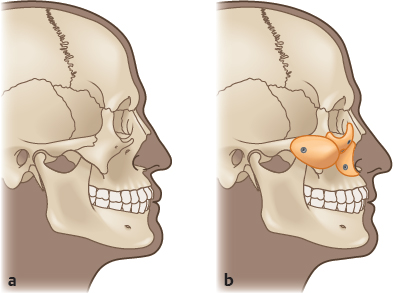
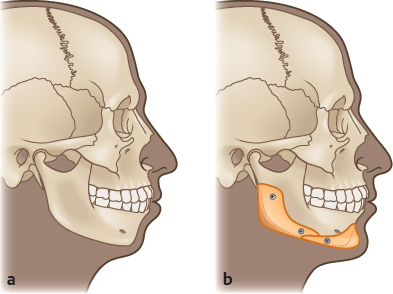
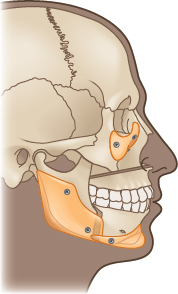
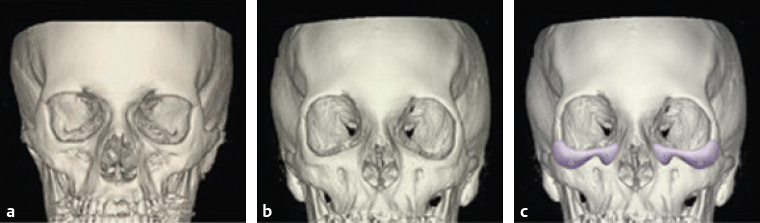
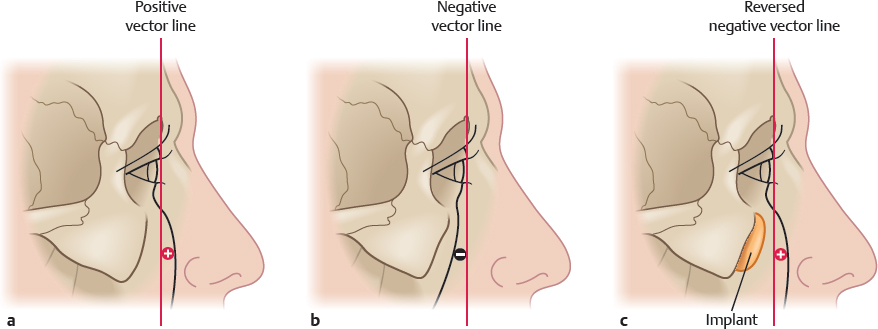
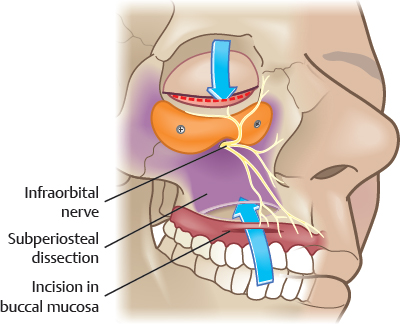
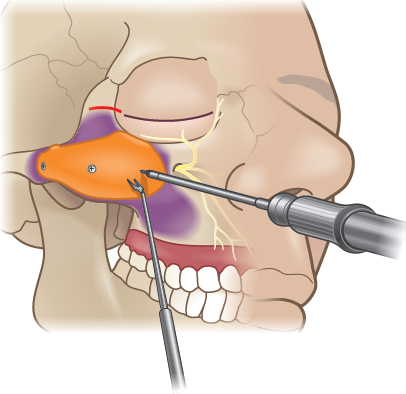
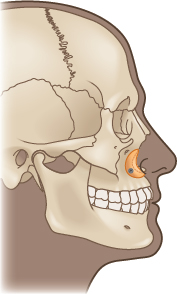
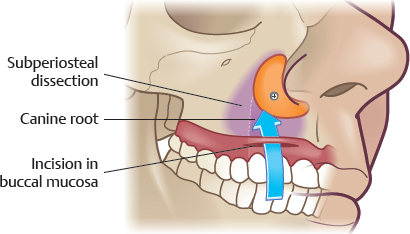
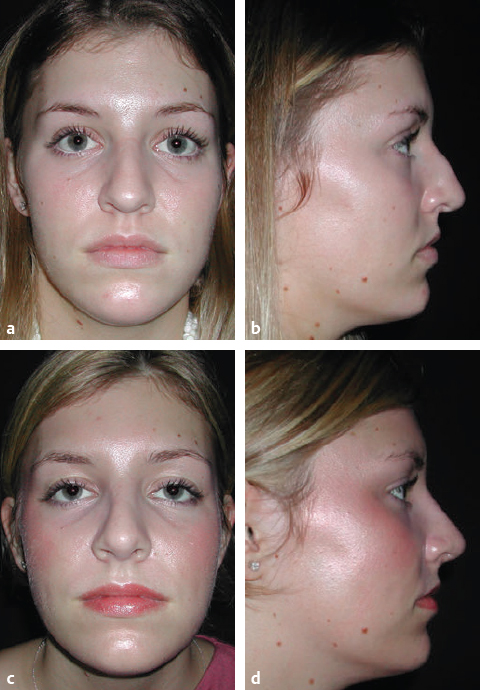
CHAPTER The use of alloplastic implants to restore or improve contour of the facial skeleton was introduced in the 1960s and 1970s when surgeons used alloplastic materials such as silastic sponges and solid polyethylene to reconstruct posttraumatic, postablative, and congenital defects. Because they were often used in compromised soft tissue environments, visibility, extrusion, and infection were not uncommon. At the same time, craniofacial techniques that advocated extensive osteotomies and the liberal use of autogenous bone as both interpositional and onlay grafts were being developed and popularized. In the 1970s and 1980s, Terino, Flowers, and Whitaker saw the potential of skeletal augmentation with alloplastic materials as an important element of aesthetic facial enhancement. Using remote incisions to place biocompatible materials under well-vascularized soft tissues, they developed techniques to alter the contours of the facial skeleton reliably. In the 1990s, I (A.Y.), with a background in craniofacial surgery, used the concepts of wide exposure and rigid fixation for alloplastic implants to enhance the facial skeleton. Although alloplastic facial skeletal augmentation can be a powerful tool to reconstruct or rejuvenate the facial skeleton, it is not without risks and complications. A thorough understanding of the facial anatomy and surgical concepts will help to minimize and eliminate these unfavorable outcomes. Summary Box Problems and Complications Associated with Alloplastic Facial Skeletal Augmentation • Skin asymmetry, malposition of implant • Contour deformity • Visibility of implant • Implant extrusion • Nerve injury • Soft tissue injury • Postoperative hematoma • Postoperative infection The problems and complications associated with alloplastic facial skeletal augmentation are listed. As in any other surgical procedure, avoidance of unfavorable outcomes starts with thorough patient assessment, selection, and careful preoperative planning. Patients with normal, deficient, surgically altered, or traumatically deformed anatomy may all benefit from implant augmentation of their craniofacial skeleton. Most often, facial skeletal augmentation is performed to enhance facial appearance in patients whose skeletal relationships are considered within the normal range but prefer more definition and angularity to their appearance. Other patients desire to “balance” their facial dimensions. Midface and mandibular hypoplasia are common facial skeletal variants. These patients have normal occlusion or have been compensated by orthodontics, with no respiratory or ocular compromise. Skeletal repositioning would necessitate additional orthodontic tooth movement. Such a time-consuming, costly, and potentially morbid treatment plan appeals to few patients. In these patients, the appearance of skeletal osteotomies and rearrangements can be simulated through the use of facial implants1 (Figs. 26.1 and 26.2). Alloplastic implants can enhance the results of certain orthognathic surgery procedures, including the LeFort I maxillary advancement, the sagittal split mandibular osteotomy, and the sliding genioplasty.2 The Le Fort I advancement may fulfill its functional role by creating an appropriate occlusal relationship but inadequately treats midface hypoplasia since only the lower half of the midface is advanced. Patients in whom the infraorbital and malar region were also deficient before Le Fort I osteotomy will continue to have these deficiencies postoperatively. The rim deficiency in the parasagittal plane may be accentuated by the more advanced position of the tooth-bearing Le Fort segment. This may result in a convexity confined to the lower half of the midface. Alloplastic augmentation of the infraorbital rim with or without malar implants can create the more aesthetic, convex midface. Posterior mandible implants can camouflage osteotomy-induced irregularities along the mandibular border as well as malpositions of the mandibular angles after bilateral sagittal split osteotomy. Chin implants with lateral extensions or specially designed and strategically placed implants can correct mandible border contour irregularities after sliding genioplasty1 (Fig. 26.3). Fig. 26.1 (a) Midface concavity and compensated occlusion. (b) Multiple midface implants provide the same visual effect as a Le Fort III osteotomy and advancement but do not alter occlusion. Fig. 26.2 (a) Mandibular deficiency with compensated occlusion. (b) The visual effect of sagittal split osteotomy and horizontal osteotomy of the chin with advancement has been simulated with mandible and chin implants. Note that the class I occlusion is unchanged. The border irregularities inherent with skeletal osteotomies are avoided when implants are used. Fig. 26.3 Infraorbital rim implants create upper midface convexity to compensate for lower midface advancement. Posterior mandible implants can camouflage osteotomy-induced irregularities along the mandibular border as well as malpositions of the mandibular angles. Chin implants can correct mandible border contour irregularities after sliding genioplasty. Fig. 26.4 The placement of infraorbital rim implant on an aged orbit creates contours that mimic a youthful orbit. (a) Computed tomography of a youthful face and orbit. (b) Computed tomography of an aged orbit. (c) Implant augmentation of the infraorbital rim restores a youthful orbital contour. (Reproduced from Yaremchuk MJ, Kahn DM. Periorbital skeletal augmentation to improve blepharoplasty and midfacial results. Plast Reconstr Surg 2009;124(6):2151–2160.) Graves’ ophthalmopathy is a chronic autoimmune condition that usually affects both orbits and involves all orbital tissue compartments, including the extraocular muscles, periorbital connective fatty tissue, and lacrimal gland. The clinical signs and symptoms of Graves’ ophthalmopathy reflect the mechanical consequences of increased orbital tissue volume and pressure within the orbit. These consequences lead to an abnormal and symptomatic protrusion of the globes from the orbits. Clinical findings are proptosis, impaired ocular motility, diplopia, lid retraction, and impaired visual acuity up to optic neuropathy, with menacing blindness. In cases of moderate to severe proptosis, favoring severity (when the relationship of the anteriormost point of the cornea to the malar eminence is of a significant negative vector), augmentation of the craniofacial skeleton with an infraorbital rim implant and a subperiosteal mid-face lift at the malar eminence effectively increase orbital volume and globe lid coverage (reversing the negative vec tor), which prove to be of substantial symptomatic relief and improved periorbital aesthetics.3 Traditional concepts of periorbital and midface aging and rejuvenation focus on the soft tissues. Recently, senescent changes in the supporting facial skeleton have been investigated. Findings in these studies revealed retrusion of the midface skeleton and mandible. This diminution in projection would hasten the gravitational-induced descent of their overlying and now less-supported soft tissue envelope.4 Alloplastic skeletal augmentation can both restore skeletal contours and support the overlying soft tissue envelope5 (Fig. 26.4). Provision of these functions supports the concept of selective alloplastic augmentation of the facial skeleton as part of the algorithm for facial rejuvenation and enhancement. Selective augmentation of the infraorbital rim and malar and piriform aperture of the aging mid-face skeleton can mimic the contours of its youthful counterpart. Selective augmentation of the chin and mandible can restore youthful contours of the lower jaw. Both the soft tissues and the facial skeleton contribute to facial contour and are affected by the aging process; therefore soft tissue augmentation (free fat grafting, fillers) and alloplastic skeletal augmentation can be used to restore youthful facial contours. However, these two modalities are not equivalent in their impact on facial appearance. Free fat grafting and the injection of various fillers are intuitive for the restoration of soft tissue volume from senile atrophy. They have a limited role in simulating the effect of an increase in skeletal projection. Whereas augmenting the facial skeleton results in an increase in the projection of the skeleton, augmenting the soft tissue volume results in an inflation of the soft tissue envelope and blunting of the contours of the skeleton. Overly aggressive augmentation of either component makes this point obvious: If excessively large implants were placed on the skeleton, the appearance would be too defined and, ultimately, skeletal. If too much fat were placed in the soft tissue envelope, an increasingly spherical and otherwise undefined shape would result. For patients who present with reconstructive problems, implant surgery is performed to return the involved area to its original appearance, or, if that is not possible, to create a face that is symmetrical and accepted as normal. For patients presenting for aesthetic enhancement, the surgical goal is more arbitrary. Because implant augmentation of the facial skeleton results in measurable changes in facial dimensions and proportions, it is intuitively advisable and appropriate to use facial measurement and proportion to evaluate the face and to help guide surgery. Physical examination remains the most important element of preoperative assessment and planning. Reviewing life-size photographs with the patient can be helpful when discussing aesthetic concerns and goals as well as demonstrating the asymmetries common to all faces. The recognition of facial asymmetries is important to the surgeon in preoperative planning and to the patient in anticipating the postoperative result. Facial asymmetries are more complex than relative skeletal deficiencies or excess; rather, they reflect three-dimensional differences that are most easily conceptualized as “twists” of the facial skeleton that can only be partially compensated for with surgery. For the purposes of painting and sculpture, Renaissance scholars and artists formulated ideal proportions and relations of the head and face based largely on classical Greek canons. Although frequently referenced in discussion of facial skeletal augmentation, these idealized neoclassical canons have a limited role in surgical evaluation and planning. When the dimensions of normal males and females were evaluated and compared with these artistic ideals, it was found that some theoretic proportions are never found, and others are one of many variations found in healthy normal people, or those determined more attractive than normal.6 The neoclassical canons do not account for facial dimensions that are known to differ with sex and age. Most of these canons of proportion (e.g., the width of the upper face is equal to five eye-widths) are interesting but hold for few individuals and cannot be obtained surgically or, if obtainable, only with extremely sophisticated craniofacial procedures. For these reasons, we have found it more useful to use the anthropometric measurements of normal individuals to guide our selection of implants for facial skeletal augmentation. Normal-dimensioned faces are intrinsically balanced; that is, the relations between the various areas of the face relate to one another in a way that is not distracting to the observer. By comparing a patient’s dimensions to the average, the surgeon has some objective basis as to what anatomic areas may be amenable to augmentation, and by how much. In general, the decision as to the size and position of the implant are largely aesthetic judgments, and most aesthetic procedures are done without preoperative radiology assessment. Cephalometric radiographs are most often used for planning chin and mandible augmentation surgery. These studies define skeletal dimensions and asymmetries as well as the thickness of the chin pad. With the advent of patient-specific custom implants using computer-assisted design (CAD) and computer-assisted manufacturing (CAM) technology, preoperative medical computed tomography (CT) or office-based cone beam CT (CBCT) is obtained for each patient to reconstruct a virtual three-dimensional model of the facial skeleton. This allows for millimeter assessment of the contour deformity: symmetry, height, width, projection, and its relationship to the entire facial skeleton. By applying knowledge of the normal skeletal relationship and aesthetic criteria, virtual surgery can be performed, and patient-specific custom implants are designed to provide the optimal surgical result. Implant materials used for facial skeletal augmentation are biocompatible—that is, there is an acceptable reaction between the material and the host. In general, the host has little or no enzymatic ability to degrade the implant, with the result that the implant tends to maintain its volume and shape. Likewise, the implant has a small and predictable effect on the host tissues that surround it. This type of relationship has an advantage over the use of autogenous bone or cartilage, which, when revascularized, will be remodeled to varying degrees, thereby changing volume and shape. The alloplastic implants presently used for facial reconstruction have not been shown to have any toxic effects on the host.7 The host responds to these materials by isolating the implant in the form of a fibrous capsule around the implant. The most important implant characteristic that determines the nature of the encapsulation is the implant’s surface characteristics. Smooth implants result in the formation of smooth-walled capsules. Porous implants allow varying degrees of soft tissue ingrowth that result in a less-dense and less-defined capsule. It is a clinical impression that porous implants, as a result of fibrous incorporation rather than encapsulation, have a lower tendency to erode underlying bone or migrate due to soft tissue mechanical forces and, perhaps, are less susceptible to infection when challenged with an inoculum of bacteria. The most commonly used, commercially available materials for facial skeletal augmentation are solid silicone, which has a smooth surface, and porous polyethylene (MEDPOR, Stryker: Kalamazoo, MI; OMNIPORE, Matrix Surgical: Atlanta, GA). Solid silicone and the silicone rubber used for facial implants are a vulcanized form of polysiloxane, a polymer created from interlinking silicone and oxygen with methyl side groups. Silicone implants have several advantages: they are easily sterilized by steam or irradiation; they can be carved with either scissors or scalpel; and they can be stabilized with a screw or suture. There are no known clinical or allergic reactions to silicone implants. Because they have a smooth surface, there is no soft tissue ingrowth, allowing them to be easily removed. Disadvantages to silicone implants include the tendency to cause resorption of underlying bone, the potential to migrate if not fixed to the underlying skeleton, and the likelihood of visibility of the fibrous capsule when placed under a thin soft tissue envelope. Polyethylene is a simple carbon chain of ethylene monomer. Polyethylene used for facial implants is porous, with intramaterial porosity between 125 and 250 µ m, which al lows fibrous tissue growth into the surface of the implant. This porous characteristic has both advantages and disadvantages. Soft tissue ingrowth decreases the tendency for the implant to migrate and to erode underlying bone. Porosity also allows some flexibility and adaptability of the implant. However, porosity causes soft tissue to adhere to the implant, making placement more difficult and requiring a larger pocket to be made than with smooth implants. The soft tissue ingrowth also makes implant removal more difficult. The firm consistency of porous polyethylene allows it to be easily fixed with screws and contoured with a scalpel or power equipment without fragmenting. The external shape of the implant should mimic the desired shape of the bone it is augmenting. Its posterior surface should mold to the bone to which it is applied. The implant margins must taper imperceptibly into the native skeleton so that they are neither visible nor palpable. Although some surgeons prefer to place implants in a soft tissue pocket, clinical experience has led us to adopt a sub-periosteal approach. Placement in a subperiosteal pocket involves a dissection that is safe to peripheral nerves and is relatively bloodless. It allows visualization and, therefore, more precise augmentation of the skeletal contour. The size of the pocket will be determined by the type of implant used and its method of immobilization. The long-standing teaching for using smooth silicone implants is to make a pocket just large enough to accommodate the implant and, therefore, guarantee its position. Porous implants require a larger pocket because they adhere to the soft tissues during their placement. Whether using smooth or porous implants, I (A.Y.) dissect widely to visualize the complex three-dimensional topography of the skeletal anatomy being augmented. This panoramic exposure allows more precise, symmetrical implant positioning. Facial implants should be immobilized. Although it is common practice to stabilize the implant by suturing it to surrounding soft tissues or by using temporary transcutaneous pull-out sutures, screw fixation of the implant to the facial skeleton is preferred. Screw fixation prevents any movement of the implant and also ensures application of the implant to the surface of the bone. Because each facial skeleton has a unique and varying surface topography, a nonconforming implant will leave gaps between the implants and the skeleton. Gaps are problematic for two reasons. The space between the implant and the skeleton is equivalent to an additional augmentation. This can lead to unanticipated increased augmentation and asymmetry. Gaps are also potential dead space for hematoma and seroma formation. Screw fixation allows for final contouring with the implant in position. This final contouring is particularly important where the implant interfaces with the skeleton. Any step-off between the implant and the skeleton will be palpable and visible in patients with thin soft tissue cover. Virtually all aesthetic augmentation is performed on the middle and lower thirds of the facial skeleton. The midface is best conceptualized as having three zones: the infraorbital rim, the malar area, and the piriform aperture. Each zone is amenable to augmentation alone or in combination. Indications for infraorbital rim implants include patients who are “morphologically prone”8 to lower lid malposition because of a retrusive upper midface skeleton and patients with a negative vector relationship between the globe and infraorbital rim as described by Jelks and Jelks.9 Infraorbital rim augmentation can “reverse the negative vector” (Fig. 26.5) and is part of the strategy for normalizing the appearance in morphologically prone patients who are first seeking improvement in their periorbital appearance or for those whose lid malposition and round-eye appearance have been exaggerated by previous lower blepharoplasty.10,11 Fig. 26.5 Jelks categorized globe–orbital rim relationships by placing a line or “vector” between the most anterior projection of the globe and the malar eminence and lid margin. (a) In the youthful face with normal globe-to-skeletal rim relations, the cheek mass supported by the infraorbital rim lies anterior to the surface of the cornea. The position of the cheek prominence beyond the anterior surface of the cornea is termed a positive vector. (b) In patients with maxillary hypoplasia, the cheek mass lies posterior to the surface of the cornea. The position of the cheek prominence beyond the anterior surface of the cornea is termed a negative vector. (c) Alloplastic augmentation of the infraorbital rim can “reverse” the negative vector. Fig. 26.6 Overview of operation to increase projection of infraorbital rim and “reverse the negative vector” in patients with upper midface skeletal deficiency. A transconjunctival retroseptal incision (broken red line) and, if necessary, the lateral extent of a lower lid blepharoplasty incision (solid line) are preferred to expose the infraorbital rim. This approach preserves the integrity of the lateral canthus and hence the palpebral fissure. Transcutaneous blepharoplasty or transconjunctival blepharoplasty with lateral canthotomy incisions are alternative approaches that provide greater exposure but are accompanied by a greater risk of palpebral fissure distortion. An intraoral incision is used to access the lower midface skeleton and to identify and protect the infraorbital nerve. The lower lid and midface soft tissues are freed by subperiosteal dissection. The implant is immobilized with titanium screws. The infraorbital rim and adjacent anatomy must be exposed sufficiently to ensure ideal implant placement, imperceptible implant–facial skeleton transition, and screw fixation. We prefer to use a transconjunctival incision together with an intraoral sulcus incision to expose the entire midface skeleton in the subperiosteal plane. The infraorbital nerve is identified as it exits from the infraorbital foramen, which is located about 1 cm below the margin of the orbit in the midpupillary line.12 The implants are carved to fit the specific needs of the patient and are fixed with titanium screws. The cheek soft tissue mass is often resuspended by sutures tied to the rim implant (subperiosteal midface lift). This technique is summarized in1 Fig. 26.6. A clinical example is shown in Fig. 26.7.5 Malar implant augmentation is often performed because full cheeks are associated with a youthful look and prominent malar bones are considered attractive. Patients with malar hypoplasia may also benefit from malar augmentation. However, the lack of anthropometric and cephalometric landmarks precludes the availability of normative data, making analysis and augmentation of the malar area largely subjective. Malar deficiency is often part of a generalized midface deficiency for which malar augmentation alone may be inadequate or even inappropriate treatment. Clinical experience has shown that when malar projection is deemed inadequate, malar augmentation is most effective when it re-creates the contours of a normal skeleton with prominent anterior projection. Fig. 26.7 (a,b) This 52-year-old woman had undergone previous browlift, rhytidectomy, and upper and lower lid blepharoplasty. Lower lid retraction was treated by multiple canthopexies, spacer grafts, and full-thickness skin grafts. Dry eye symptoms persisted. Infraorbital rim augmentation, midface lift, and lateral canthopexy resolved her symptoms. Her brows and hairline were repositioned. (c,d) The procedure transformed the preoperative negative vector to a positive vector globe–rim relationship. The vertical lines define the globe–rim relationship. (Reproduced from Yaremchuk MJ, Kahn DM. Periorbital skeletal augmentation to improve blepharoplasty and midfacial results. Plast Reconstr Surg 2009;124(6):2151–2160.) Malar augmentation can be performed through intraoral, coronal, or eyelid incisions or combinations thereof. I (A.Y.) prefer to access the malar midface through an intraoral approach (an upper sulcus incision). Transconjunctival and crow’s-feet incisions are often performed to ensure proper placement of the superior aspect of the implant. Care is taken to identify the infraorbital nerve. Subperiosteal dissection is carried over the malar eminence and onto the zygomatic arch almost up to the zygomaticotemporal suture. The pocket size should allow precise insertion of the implant to the area of the skeleton desired for augmentation. The implants can be stabilized with screw fixation to the underlying skeleton (Fig. 26.8). A clinical example is shown in Fig. 26.9.1 The face of individuals of Western European descent is typically convex. A relative deficiency in lower midface projection may be congenital or acquired, particularly after cleft surgery and trauma. Patients with satisfactory occlusion but lower midface concavity can have their aesthetic look improved with piriform aperture augmentation, which simulates the visual effect of Le Fort I advancement and other skeletal manipulations. Piriform aperture augmentation also increases the projection of the nasal base, thereby opening the nasolabial angle.13 Finally, it lessens the depth of the nasolabial fold by effacing it from below (Fig. 26.10).1 Fig. 26.8 Overview of the operative technique for malar augmentation. The upper sulcus incision is at least 1 cm above the apex so that sufficient tissue is available for closure. Transconjunctival and crow’s-feet incisions ensure proper placement of the superior aspect of the implant. The infraorbital nerve is identified, and the subperiosteal dissection is carried over the malar eminence and on to the zygomatic arch just beyond the zygomaticotemporal suture. Registration tabs on the implant rest on the lateral aspect of the infraorbital rim and superior aspect of the zygomatic arch and decrease the likelihood of asymmetrical implant placement. Implants are fixed with titanium screws for immobilization and for obliteration of the dead space between the posterior surface of the implant and the anterior surface of the facial skeleton. The implants are contoured so that they are identical in size and shape, are appropriate for the area to be augmented, and merge imperceptibly with the native skeleton. A trochar-attached suction drain is placed. It exits through the temporal hair-bearing scalp or the postauricular area. The colored area denotes the area of subperiosteal dissection. The implant usually extends from the temporozygomatic suture on the zygomatic arch to just below the foramen of the infraorbital nerve. An intraoral incision is made approximately 1 cm above the sulcus, the medial extent of which is made just lateral to the piriform aperture to avoid placing incisions directly over the implant. Subperiosteal dissection exposes the area to be augmented, and the infraorbital nerve is identified and preserved. The patient’s anatomy will determine whether the entire crescent, or just the horizontal or vertical limb of the crescent-shaped implant, will be used. The root of the canine should be avoided if the implant is immobilized with screws. The implant may compromise the nasal airway if positioned over the piriform aperture. The technique is illustrated in Fig. 26.11.1 A patient who underwent aesthetic rhinoplasty and augmentation of the piriform aperture area is shown in Fig. 26.12.1 Fig. 26.9 This 48-year-old woman underwent an infraorbital rim, malar, chin, and mandible implant augmentation, together with a browlift reversal and midface lift. (a) Preoperatively, the patient had already undergone a browlift, blepharoplasty, and rhytidectomy. (b) Result at 1 year postoperatively. (Reproduced from Yaremchuk MJ. Skeletal augmentation. In: Neligan P, ed. Plastic Surgery, Vol 2. 3rd ed. London: Elsevier; 2012.) Fig. 26.11 Overview of paranasal implant surgery. The purple area indicates the area of subperiosteal dissection. Note proximity of infra-orbital nerve. Note that the root of the canine tooth lies below the area to be augmented. It must be avoided during screw immobilization of the implant. Fig. 26.12 (a,b) This 20-year-old woman underwent rhinoplasty and paranasal augmentation. (c,d) The skeletal augmentation increased the nasolabial angle. Because midface concavity tends to increase the relative projection of the nose, creating midface convexity tends to lessen the relative projection of the nose. (Reproduced from Yaremchuk MJ. Skeletal augmentation. In: Neligan P, ed. Plastic Surgery. Vol 2. 3rd ed. London: Elsevier; 2012.) A review of the literature shows that there is a high incidence of revision surgery after alloplastic malar augmentation.14–16 Asymmetry is the most common complaint after malar implant augmentation (Fig. 26.13), followed by malposition of the implants where they are placed too low.17 Although treatment consists of secondary surgery to replace or reposition the malar implants, such unfavorable results can be minimized by obtaining adequate skeletal site exposure during primary surgery to ensure accurate implant placement and screw fixation. More recently, implant designs include registration tabs that rest on the lateral aspect of the infraorbital rim and superior aspect of the zygomatic arch (see Fig. 26.8). Placement of the implants on fixed anatomic landmarks decreases the likelihood of asymmetrical implant placement. Patients with midface hypoplasia often require augmentation of both the infraorbital rim and malar eminence. The advent of custom implants using CAD–CAM technology allow precise preoperative planning, better fit, and more predictable postoperative facial contour than stock implants. A clinical example is shown in Fig. 26.14. Visibility of malar implants results from an improper implant size or encapsulation of a smooth-surface implant by the host’s foreign body response. Although implants with greater projection are available, we rarely use malar implants with more than 4 mm of augmentation at the point of maximum projection. Larger implants may become obvious with time as the overlying soft tissues atrophy and sag. The capsule formation that accompanies smooth-surface implants further exaggerates the tendency toward implant visibility. In my (A.Y.) experience, implants with large surface areas do not mimic natural skeletal topography and cause unnatural implant-dictated contours. The operative strategy for visible malar implants is largely determined by the patient’s concerns and the interval between implant placement and patient presentation. If revision surgery is pursued within weeks to months of the original surgery, implant removal, repositioning, or replacement alone may be appropriate.18 When implants have been in place long enough to be visually encapsulated, revision surgery becomes more complex. The capsule, scar tissue mimicking the contours of the implant, permanently distorts the soft tissue envelope. Its impact on the appearance of the cheek will depend on the size and projection of the implant, and the thickness of the overlying cheek soft tissue will become thinner. Moreover, the contour distortion may be exaggerated implant-induced bone erosion, with subsequent loss of skeletal projection. In these cases, after removing the offending malar implants and replacing them with ones of appropriate size and shape, the soft tissue distortion is then treated by repositioning of the midface soft tissues via a subperiosteal midface lift.17,19 A clinical example is shown in Fig. 26.15.
26
Alloplastic Implants for Facial Contouring
Avoiding Unfavorable Results and Complications Associated with Alloplastic Facial Skeletal Augmentation
Patient Selection
Skeletal Enhancement
Alternative to Orthognathic Surgery
Adjunct to Orthognathic Surgery
Graves’ Ophthalmopathy
Rejuvenation
Skeletal Versus Soft Tissue Augmentation
Preoperative Assessment and Planning
Physical Examination
Neoclassical Canons and Facial Anthropometries
Radiology
Implant Materials
Silicone
Polyethylene
Requisites of Implant Shape, Positioning, and Immobilization
Shape
Positioning
Immobilization
Midface Skeletal Augmentation
Infraorbital Rim
Surgical Technique
Malar Area
Surgical Technique
Piriform Aperture
Surgical Technique
Unfavorable Outcomes and Complications of Midface Skeletal Augmentation
Asymmetry or Malposition of the Implant
Visibility of Implant
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine