20 Airway issues and the deviated nose
Synopsis
 A thorough history and physical examination are required. History of nasal trauma, prior nasal surgery, airway complaints, and allergies are ascertained.
A thorough history and physical examination are required. History of nasal trauma, prior nasal surgery, airway complaints, and allergies are ascertained.
 Three-dimensional evaluation as well as cephalometric analysis of life-size photographs is performed in order to evaluate the location and severity of asymmetry.
Three-dimensional evaluation as well as cephalometric analysis of life-size photographs is performed in order to evaluate the location and severity of asymmetry.
 A detailed evaluation of the upper nose (nasal bones and upper lateral cartilages), septum, lower lateral cartilages, anterior nasal spine and medial crural footplates will give an accurate assessment of asymmetry.
A detailed evaluation of the upper nose (nasal bones and upper lateral cartilages), septum, lower lateral cartilages, anterior nasal spine and medial crural footplates will give an accurate assessment of asymmetry.
 The open rhinoplasty is the preferred approach for correction of the deviated nose. It provides the widest exposure and the best opportunity to anatomically realign the deviated structures.
The open rhinoplasty is the preferred approach for correction of the deviated nose. It provides the widest exposure and the best opportunity to anatomically realign the deviated structures.
 A rare unilateral nasal bone asymmetry can be corrected with an onlay graft, but it is not the optimal choice.
A rare unilateral nasal bone asymmetry can be corrected with an onlay graft, but it is not the optimal choice.
 The mid-vault deviation is invariably associated with a septal deviation and a successful correction will require a problem oriented septoplasty.
The mid-vault deviation is invariably associated with a septal deviation and a successful correction will require a problem oriented septoplasty.
 When correcting the deviated mid-vault, it is almost always necessary to separate the upper lateral cartilages from the septum.
When correcting the deviated mid-vault, it is almost always necessary to separate the upper lateral cartilages from the septum.
 The upper lateral cartilages should not be trimmed until the nasal bones have been repositioned.
The upper lateral cartilages should not be trimmed until the nasal bones have been repositioned.
 Deviation of the caudal third of the dorsum may require a septal rotation suture.
Deviation of the caudal third of the dorsum may require a septal rotation suture.
 Deviation of the base of the nose is invariably associated with asymmetric lower lateral cartilages, the correction of which is essential to a successful elimination of asymmetry from this part of the nose.
Deviation of the base of the nose is invariably associated with asymmetric lower lateral cartilages, the correction of which is essential to a successful elimination of asymmetry from this part of the nose.
 Another integral component of the caudal nasal deviation is the dislodgement of the cartilaginous septum to one side of the vomer bone. Removal of the redundant and overlapping portion of the cartilage is paramount to the straightening of the columella and the base of the nose.
Another integral component of the caudal nasal deviation is the dislodgement of the cartilaginous septum to one side of the vomer bone. Removal of the redundant and overlapping portion of the cartilage is paramount to the straightening of the columella and the base of the nose.
 Longstanding deviation of the septum to one side is invariably associated with enlargement of the opposing inferior and sometimes the middle turbinate.
Longstanding deviation of the septum to one side is invariably associated with enlargement of the opposing inferior and sometimes the middle turbinate.
Introduction
Anatomy
Nasal anatomy is covered in Chapter 17. Specific anatomy, as it relates to the airway, can be organized into soft tissue and osseocartilaginous categories. Although less commonly involved in nasal airway disorders, the soft tissue envelope with its underlying perinasal musculature plays a vital role in maintaining the patency of the valvular mechanism.
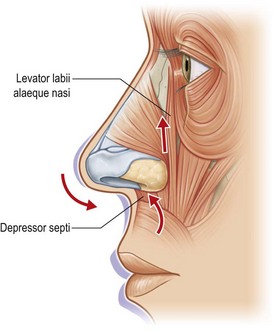
The perinasal musculature can be divided into an intrinsic (having both origin and insertion within the perinasal area) and an extrinsic group containing three paired muscles.1,2
The three paired muscles of the extrinsic group include the levator labii superioris alaeque nasi, zygomaticus minor, and the orbicularis oris. Of these, the levator labii superioris alaeque nasi is the most important dilator with the zygomaticus minor providing lateral wall stability (Fig. 20.1).
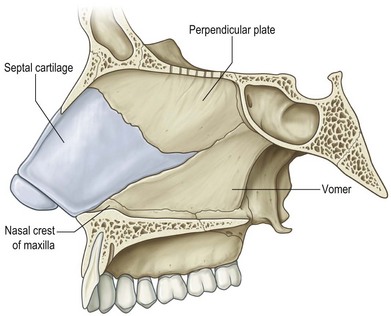
When considering the structures of the osseocartilaginous vault, the most important central support for the nose is the septum (Fig. 20.2). The perpendicular plate of the ethmoid articulates with the posterior edge of the quadrangular (septal) cartilage and both structures articulate with the vomer inferiorly. The vomer then lays directly on the maxillary crest. The anterior-caudal most portion of the septal cartilage also rests on the maxillary crest, however, in a tongue-and-groove relationship. This point of articulation is unique in that the perichondrium of the cartilage is only partially contiguous with the periosteum of the crest allowing a decussation of fibers which joins the contralateral perichondrium.2 This crossed configuration can make a seamless submucoperichondrial dissection less than facile. It also lends this portion of the septum susceptible to post-traumatic displacement out of the groove of the crest.
The upper and lower lateral cartilages also play a significant role in nasal support. The point at which the caudal margin of the upper lateral cartilages and the cephalic rim of the lower lateral cartilages overlap is defined as the scroll area. Cartilaginous overlap in this region has been shown to enhance support at this level.3 Superiorly, another area of overlap occurs at the junction between the cephalic upper lateral cartilages and the nasal bones. This makes up the keystone area and is characterized by a firm adherence between these structures. Subsequently, trauma to the nasal bones can shift this entire unit. In addition, the upper lateral cartilages are fused to the septum in the mid-vault region and separate as one moves caudally. This is clinically important during placement of spreader grafts, as this region will require sharp dissection to release the upper lateral cartilage from the septum.2
Although not of structural significance, the inferior turbinate occupies a large portion of the nasal airway and can account for up to two-thirds of the total airway resistance.4 It is composed of dense lamellar bone taking origin from the medial wall of the maxilla bilaterally. The turbinates are covered with an erectile mucosal tissue composed of pseudostratified ciliated columnar epithelium. The submucosa contains large quantities of seromucinous glands and vascular channels containing cavernous sinusoids. These channels are under the influence of the autonomic nervous system and thus serve as the end target for decongestant medication. The sympathetic system regulates the resistance vessels (and therefore blood flow) and the parasympathetic system regulates the capacitance vessels (and therefore blood volume) of the nasal mucosa. The submucosa also contains large numbers of mast cells, eosinophils, plasma cells, lymphocytes, and macrophages. Thus, chronic inflammation, secondary to stimulation of these abundant pro-inflammatory cellular constituents can lead to fibrous deposition and chronic hypertrophy of the turbinate.2
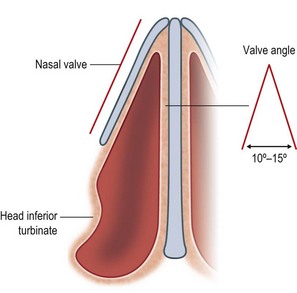
The internal nasal valve accounts for approximately 50% of the total airway resistance and is the narrowest segment of the nasal airway.5,6 It is formed by the angle between the junction of the nasal septum and the caudal margin of the upper lateral cartilage and is typically 10–15° (Fig. 20.3).
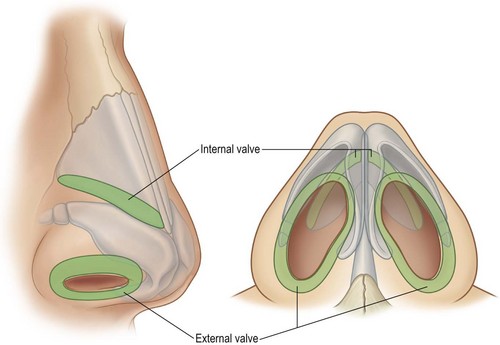
The external nasal valve is formed by the caudal edge of the lateral crus of the lower lateral cartilage, the soft tissue alae, the membranous septum, and the sill of the nostril and serves as the entrance to the nose. This is an occasional site of obstruction secondary to extrinsic factors, such as foreign bodies, or intrinsic factors, such as weak or collapsed lower lateral cartilages, a loss of vestibular skin, or cicatricial narrowing (Fig. 20.4).7
Physiology
As described in Eugene Courtiss et al.’s overview on nasal physiology, the nose has seven basic functions: respiration, temperature regulation, humidification, particulate filtration, olfaction, phonation, and as a secondary sex organ. The most vital of these functions is respiration and can be described using some basic laws of physics.8
When there is a pressure differential between the external nasal vestibule and the nasopharynx, a gradient is formed and air flows through the nose. Thus, an increase in nasal resistance (decreases in nasal airflow) can result from such structural limitations as hypertrophied turbinates, septal deviations, valve incompetence, or intranasal masses. The magnitude of nasal airway resistance cannot be underestimated and, in fact, is responsible for approximately half of the total respiratory tree resistance.5,6
Bernoulli’s principle defines flow through a tubular structure such that the flow at the two ends is constant. In addition, areas of constriction increase flow and areas of dilation decrease flow. In these areas of increased flow, the pressure is decreased and vice versa in areas of decreased flow.8 This becomes clinically evident in the incompetent internal or external nasal valve. Because these are areas of narrowing/constriction, airflow is increased at the level of the valve, leading to a decrease in pressure. This effectively generates a collapsing force on the valves and is exacerbated upon heavy inspiration or sniffing.2
Bernoulli’s principle can be mathematically substantiated using Poiseuille’s law. This law provides that flow is directly proportional to the difference in pressure multiplied by the radius raised to the fourth power and inversely proportional to the length of the tube.8
This demonstrates that the longer the tube (nose), the less the flow. Even more dramatic is that a minimal increase in the size of the tube causes an exponential (r4) increase in flow. This has clinical implications as the cross-sectional area varies throughout the nose. It is narrowest at the internal nasal valve, larger at the level of the mid-turbinates, and largest at the level of the posterior choanae. As a result, minimal changes at the level of the internal nasal valve can have profound changes on nasal airflow and is subsequently cited as the most common cause of nasal airway obstruction.9–11
An understanding of laminar and turbulent flow is also essential to a complete understanding of respiration and nasal airflow physiology and dynamics. When laminar flow exists, air moves through a straight tube in a predictable fashion. Air near the walls of the tube is virtually still, whereas flow in the center moves rapidly. This is in contrast to turbulent flow, where the airflow follows a random path and forms eddy currents and whorls. To overcome turbulence, a greater pressure gradient must be generated. In other words, the less laminar the airflow, the higher the resistance and the lower the airflow. For example, during quiet respiration where pressures are low and under 1.5 cm of water, nasal airflow is considered to be laminar.12 During inspiration, the main airflow is directed through the middle meatus with a smaller amount coursing through the inferior meatus and an even smaller amount up toward the cribriform plates.13,14
Finally, another less well understood factor in nasal airflow is the nasal cycle (cycle of Minz). Approximately 80% of the population experiences cyclical swelling and contraction of the nasal mucosa. While one airway is enlarging, the other is constricting.15,16 The process requires 30 min to 5 h to complete and total airflow and resistance remains constant throughout this period.17
Temperature regulation and humidification
The physiologic nasal regulatory system is so efficient that inspired air is heated almost to body temperature before it even reaches the larynx. Even air at temperatures of −5°C is brought to between 31°C and 37°C. This function typically requires 70–100 calories per day.10,18
Regardless of the ambient temperature or humidity, approximately 90% humidification is achieved during inspiration before the air reaches the lungs. This requires 1 liter (L) of water per day.19 A small amount of this water is recovered during exhalation secondary to cooling of the exhaled air, however a net balance of −250 mL to −500 mL per day still exists.20
Particulate filtration
Four mechanisms have been described by which the nasal cavity achieves adequate filtration of inspired air. These include impingement, electrostatic charge, vibrissae, and the mucociliary blanket. Impingement is a phenomenon that occurs when particles suspended in a gas become deposited on the walls of a tube downstream from a bend or constriction. Two such bends exist within the nasal cavity: the internal nasal valve, where the airflow is changed from a column into a sheet, and at the posterior nasopharynx, where the airflow is sharply deflected inferiorly. These two anatomic impingement points are responsible for the deposition/filtration of 85–90% of particulate matter ≥5 µm.18 The electrostatic charge of the walls of the nasal cavity is positive and produced by the mucociliary blanket. Thus, the negatively charged inspired foreign particles are attracted to the nasal walls and prevented from traveling distally to more sensitive areas of the respiratory tract. Larger particles are trapped within the vibrissae, which are found just within the nasal vestibule. The mucociliary blanket is composed of two layers: the deeper layer is thinner and less viscous and surrounds the cilia, while the superficial layer is thicker and more viscous and houses the cilia tips. As a whole, the mucociliary blanket is a thin, sticky, adhesive sheet with a pH slightly more acidic than serum. It is produced by serous and mucous glands and by the goblet cells of the mucosa at a rate of about 250 mL per day. This blanket ultimately functions, in a rhythmic fashion, to sweep particulate matter to the posterior nasopharynx.2,18
Olfaction
Olfaction clearly enhances our sense of taste and aids in memory association. It may also play a protective role by warning of potential environmental dangers when noxious odors are perceived. Causes for an olfactory disturbance are many and include infection, trauma, mechanical obstruction, endocrine disorders and medications to mention a few. In addition, nasal septal surgery can infrequently lead to anosmia; fortunately, this is most often temporary.8,21
Phonation
It is well known that the voice is produced via vibrations of the vocal cords with the passage of air. However, the quality of the voice depends on the resonance of air through the mouth, pharynx, and nose. As a resonance chamber, the nose is a necessary component in the formation of certain vowels and consonants alike. Patients may therefore ask if nasal surgery will alter the sound of their voice. To that end, they can be counseled that post-surgical changes in the sound of ones’ voice have not been substantiated. Septal perforations, however, change airflow resistance and thus, may change voice quality and/or create a nasal whistle with inspiration.8
Secondary sex organ
It has been known for some time that mucosal engorgement occurs during sexual arousal.16 A relatively recent discovery in nasal physiology is the vomeronasal organ (Jacobson’s organ, Ruysch tube). It is composed of bilateral blind ducts in the mucosa of the anterior third of the human septum.22–25 Their role is not fully understood, but it is felt that they play a part in reproductive behavior by acting as pheromone chemosensory receptors. The external opening of the ducts can be found in the septal mucosa just posterior to the columellar base and 1 mm above the maxillary groove.25
Basic science/disease process
Rhinitis
Rhinitis can be the result of a number of different causes including infectious, allergic, vasomotor, atrophic, rhinitis medicamentosa, postoperative, hypertrophic, and miscellaneous. It has even been cited as the number one cause of nasal obstruction.9
Infectious rhinitis is the most common type, and presents in two forms: viral and bacterial. Viral rhinitis is more common than bacterial etiologies and is usually the result of the rhinovirus. Bacterial rhinitis is mostly caused by Gram-positive isolates. Regardless of the etiology (viral or bacterial), there is significant mucosal edema during infection and this can last for several weeks leading to a narrowed nasal airway with subsequent obstruction.26,27
Allergic rhinitis is said to have prevalence of between 14% and 31% in the United States alone.28 True allergic rhinitis is mediated by immunoglobulin E in response to an antigen-antibody reaction. This most commonly presents in a seasonal form from environmental factors such as an air-borne pollen or spore. Associated symptoms include sneezing, urticaria, and mucosal swelling.
Vasomotor rhinitis arises when the balance between the sympathetic and parasympathetic nervous systems is disrupted, such that the parasympathetic system is hyperactive. This leads to copious amounts of watery rhinorrhea and mucosal congestion. Although most commonly idiopathic in nature, other potential causes include pregnancy, and endocrine and emotional disorders.2
Atrophic rhinitis is a rare condition with its typical onset in puberty and characterized by a slow, progressive atrophy of the nasal mucosa. This results in crusting and often foul smelling drainage.5 Several organisms have been isolated from patients affected by this condition, however their exact mechanism in the pathogenesis remains unclear.29,30 A subcategory of atrophic rhinitis, is “empty nose syndrome”. This is a poorly understood and highly debated iatrogenic disorder which results from the destruction of normal nasal tissue; specifically the turbinates. The most commonly reported symptoms include a paradoxical nasal obstruction and feeling of intranasal fullness.
Rhinitis medicamentosa (RM) occurs frequently in patients who present with nasal airway obstruction. It is seen with prolonged use of sympathetic agonists such as Afrin or Neo-Synephrine and leads to a rebound phenomenon of mucosal engorgement and profuse rhinorrhea. Patients often try increasing both the dose and the frequency of nasal sprays upon the onset of RM, worsening the condition. The swelling of the nasal passages caused by rebound congestion may eventually result in permanent turbinate hyperplasia.31
Miscellaneous causes of rhinitis may include such medications as oral contraceptives, antihypertensives (beta-blockers), and antidepressants. Other causes include Wegener’s granulomatosis, polymorphic reticulosis, cystic fibrosis, syphilis, hypothyroidism, and poorly regulated diabetes.5,32
The septum
The septum and the nasal bones control the direction of the nose and thus, deviation of the nose can result from malalignment of one or the other or a combination of both. Often, the nasal bones follow the direction of the deviated septum, however these structures may move independently. Mid-vault deviation consistently accompanies at least anterior and commonly mid and posterior septal deviation. Deviation of the lower nose may involve the caudal septum, anterior nasal spine and lower lateral cartilages. In all types of septal deviation, the middle and/or inferior turbinates may be enlarged. The enlargement is usually juxtaposed to the concave side of the septum. Previous studies have detailed and categorized the types of septal deviation.33–36
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree