Chapter 18 Aesthetic classification of the abdomen
• Abdominal contour surgery represents a group of procedure options available for esthetic improvement of the abdomen.
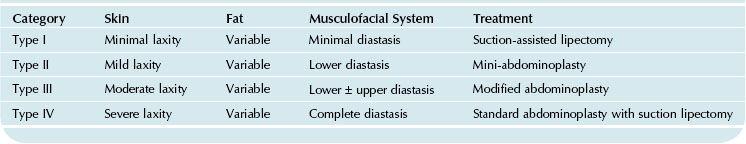
• The abdominolipoplasty system of classification and treatment (type I-suction-assisted lipectomy (SAL); Type II & III – limited abdominoplasties; Type IV abdominoplasty with or without liposuction) provides the framework on which procedure selection is based (Fig. 18.1 and Table 18.1).
• The appropriate procedure is based on reconciling the patient’s anatomic findings with their goals; and taking into considering such factors as their tolerance for the length of the lower abdominal scar and an umbilical scar.
• Overall, liposuction of the abdomen is the most frequent abdominal contour procedure. As surgeons have become familiar with incorporating liposuction with a full abdominoplasty, abdominoplasty with liposuction referred to as Lipoabdominoplasty has become more mainstream. This and abdominoplasty alone without liposuction (conventional abdominoplasty) represent the most common types of “open” options for the abdomen.
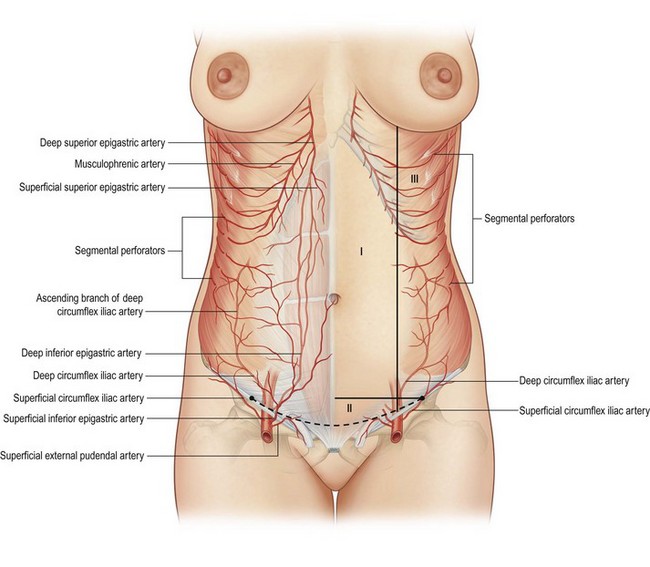
• Lipoabdominoplasty is an operation based on the principles of preserving the maximum blood supply to the anterior abdominal wall (Fig. 18.2) and of creating a narrow tunnel of undermining (zone of complete undermining) to the xiphoid in order to access the rectus diastasis with a surrounding zone of selective undermining and a zone of discontinuous undermining (Fig. 18.3).
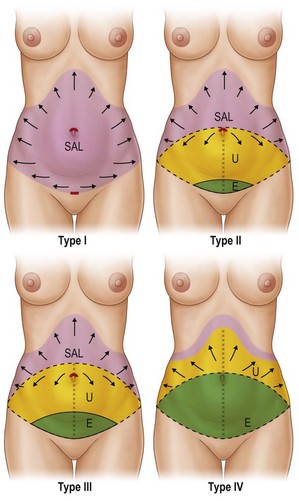
FIG. 18.1 The abdominoplasty system of treatment and classification is based on evaluating the treatable soft tissue layers of the abdomen. Type I (upper lift) is liposuction alone; Type II (upper right) is mini-abdominoplasty; Type III (lower left) modified abdominoplasty (or lower abdominoplasty or marriage abdominoplasty); Type IV (lower right) a full abdominoplasty without or with (lipoabdominoplasty) liposuction. (Pink = liposuction, yellow = undermining, green = excision).1

FIG. 18.3 Lipoabdominoplasty is based on the principle of undermining to the xiphoid in a narrowed tunnel leaving intact intercostal (Huger zone III) blood supply. Surrounding this is a zone of selective undermining that is done sharply to free any excessive skin bunching that occurs after rectus fascia plication. The zone of discontinuous undermining results from the blunt dissection of the liposuction cannula.3
![]() For additional online content visit http://www.expertconsult.com
For additional online content visit http://www.expertconsult.com
1. Abdominoplasty in the presence of nonmidline pre-existing upper abdominal scars or flank scars.
2. When the goal is also to achieve a narrower waistline.
3. Downstaging to a less invasive alternative in patients not willing or able to have a more invasive operation.
4. Obese patients who require a panniculectomy with extensive SAL (also known as liposuction with lower skin resection or lower abdominoplasty or modified abdominoplasty).
5. Abdominoplasty in a patient who previously had liposuction.
6. Secondary full abdominoplasty.
7. Removing the old umbilical site in long-waisted individuals.
8. Converting a prior limited (possibly that had an umbilical float) abdominoplasty to a full abdominoplasty.
9. Bariatric plastic surgery (massive weight loss patients).
Preoperative Preparation
Surgical markings are made in conjunction with the patient so that stab wound incisions for liposuction are well hidden and abdominoplasty incisions are confined to the limits of their undergarments. The abdominal excision is essentially an ellipse of tissue removal between the umbilicus and the mons pubis (Fig. 18.4). The length of the abdominoplasty incision is determined by locating the ends of the pannus’ skin creases, which are determined in a sitting position and noting the ends of the skin folds.
The lower incision is then marked between those two points, approximately 6 to 7 cm superior to the vulva cleft and incorporating removal of any lower (Pfannenstiel, cesarean, etc.) scars. The upper incision is then drawn across the top of the umbilicus from hip-point to hip-point, joining the lower incision and completing the ellipse. The ability to remove the lower abdominal skin pannus from umbilicus to pubis is verified by the surgeon grasping the skin and their fingers meeting. In an abdominoplasty it is preferable to remove enough tissue so that the old umbilicus site is removed with it. In the operating room the markings are verified by placing long silk sutures (after any liposuction is performed) in the midline at the xiphoid and pubis and overlapping them at multiple points on the upper and lower incision in order to ascertain symmetry between sides of the incision (Fig. 18.5).
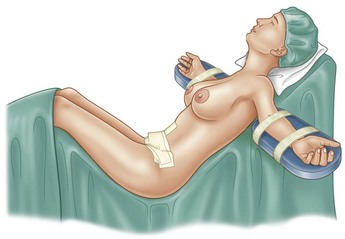
All procedures are undertaken with systemic anesthesia (spontaneous ventilation GA, or spinal/epidural) administered by an anesthesiologist. The operative field is injected with approximately 1 liter of super-wet anesthesia (1 liter of Ringer’s lactate, 20 ml of 1% lidocaine, 1 ml of 1 : 1000 epinephrine). Limiting the wetting solution allows safe injections to any additional operative sites, by avoiding potentially toxic doses of lidocaine or epinephrine (0.07 mg/kg of 1 : 1000 epinephrine) and excess fluid would ultimately encumber electrocautery use during surgery. In “open” procedures 20 ml of 1% Marcaine is injected at various points in the muscle layer. A Foley catheter is inserted for open (non-SAL only) procedures. The arms are symmetrically placed on arm boards while avoiding pressure points and secured with curlex wraps. Preoperatively the bed is checked to verify that it can reach a maximum beach chair position, which is necessary for wound closure and removing the old umbilical site (Fig. 18.6).
Options
Table 18.2 illustrates the patient’s potential anatomic issues that can affect procedure selection.
TABLE 18.2 Anatomic Characteristics
| Skin | Laxity, striae gravidum, tone, thickness |
| Fat | Subcutaneous, visceral |
| Muscle | Extent of rectus muscle diastasis and the quality of the muscle Hernia (peri/umbilical or hernias elsewhere) |
| Prior surgery | Circumscribed umbilicus, limited abdominoplasty with a floated umbilicus, liposuction, presence of nonmidline upper abdominal scars, flank scars or inframammary scars |
Box 18.1 illustrates some of the issues that influence patient decisions about which abdominal contour procedure they are interested in undertaking.
Box 18.1
Sample of Factors that Commonly Influence the Procedure that Patients Select
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 of an inch) on their waistlines. Women over 40 years old would need to exercise over 1 hour a day to just retain the appearance of their earlier figure.
of an inch) on their waistlines. Women over 40 years old would need to exercise over 1 hour a day to just retain the appearance of their earlier figure.