Advancement
INTRODUCTION
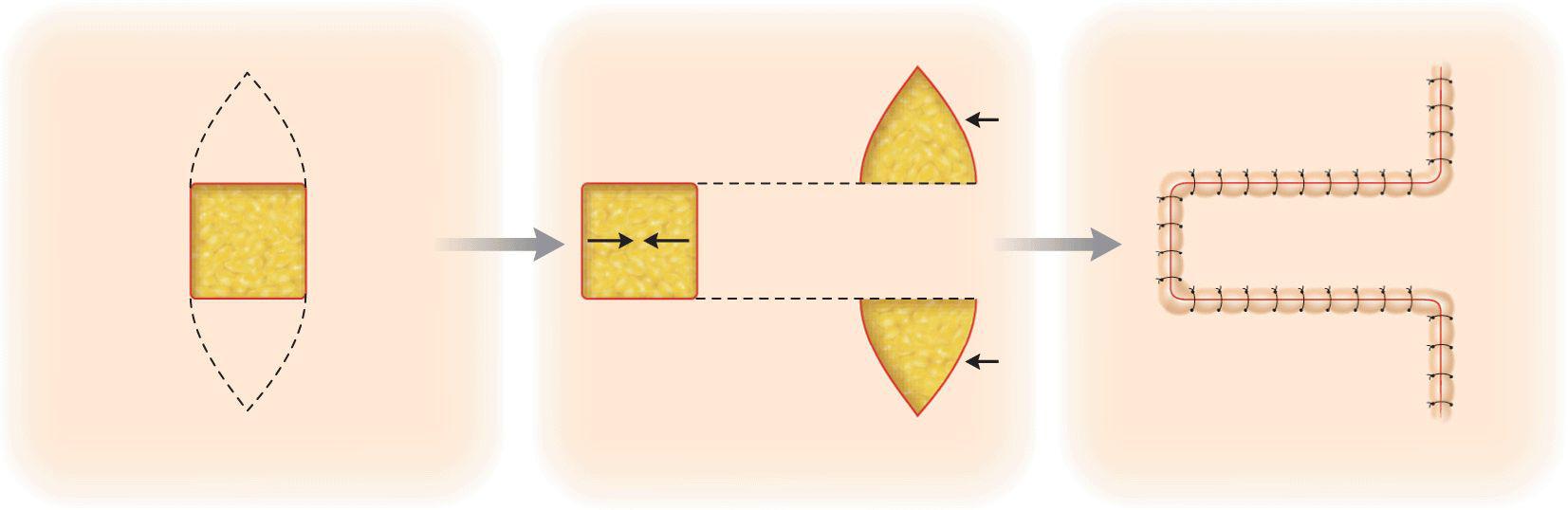
The advancement flap is the oldest and most straightforward type of adjacent tissue transfer, since it is basically a geometric and biomechanical extension of the fusiform or lenticular closure (Fig. 2.1). As compared to primary side-to-side closure, the advancement flap provides a small amount of additional tension release and no tension redistribution. The unique attribute of the advancement flap is the ability to redistribute and selectively position collections of tissue redundancy termed dogears when they are generated by wound closure.1 Advancement flaps have widespread utilization in the repair of facial operative wounds, and despite their relative simplicity, they are the most common type of nonlinear reconstruction utilized by most surgeons. Their design and execution is enhanced by a thorough understanding of the principals of tissue motion. Interestingly, less literature attention has been paid to the design of advancement flaps than to their more complex cousins, transposition, and rotation.
Figure 2.1 An advancement flap transposes the dog-ears of a fusiform closure to a site away from the operative wound
BIOMECHANICS
An advancement flap moves tissue linearly from a site of origin to a recipient destination. The tension vector of closure is the same, or nearly the same, as would be the case if the wound were closed linearly. From an undermining standpoint, there is little mechanistic difference between the creation of an advancement flap and the execution of an elliptical closure. The edges of a primary closure may be undermined for a distance equivalent to that of a flap, generating equal degrees of deep tension release. Following appropriate undermining, the mobility of both advancement flaps and fusiform closures is primarily limited by a tension vector directed 180° away from the direction of the advancement. Nonetheless, there are subtle changes in mobility effected by the creation of an advancement flap.
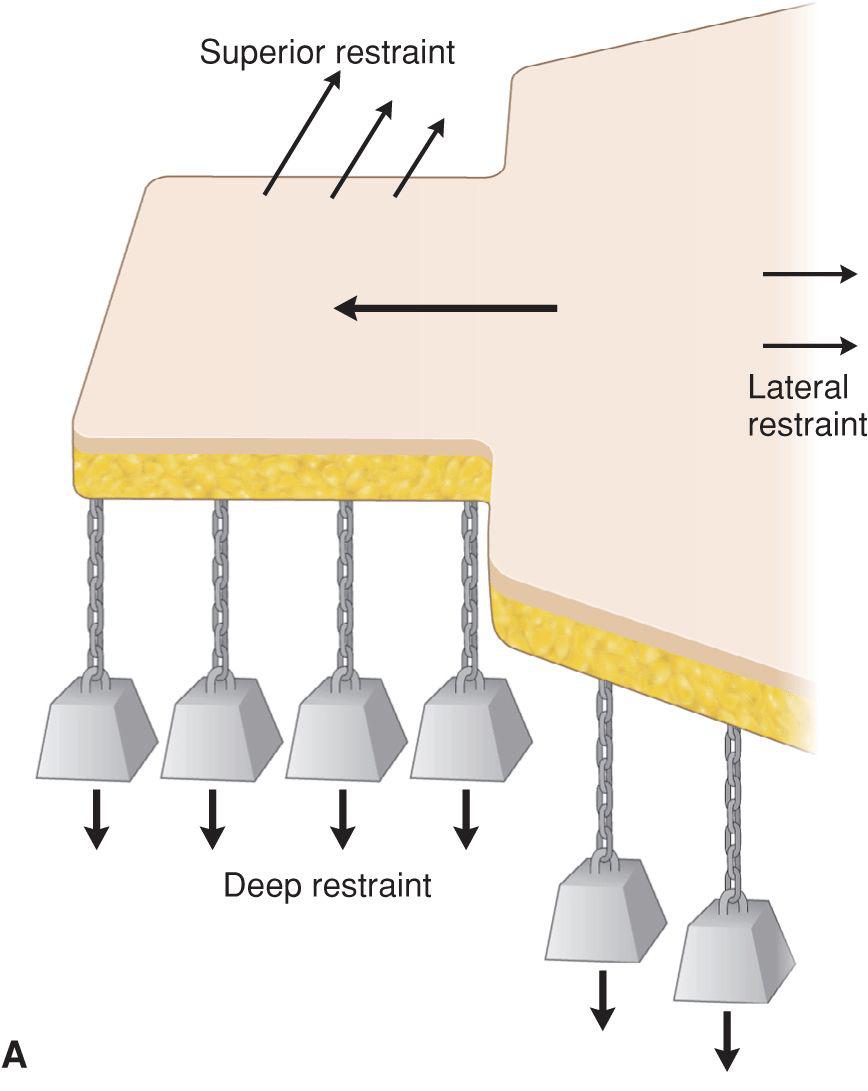
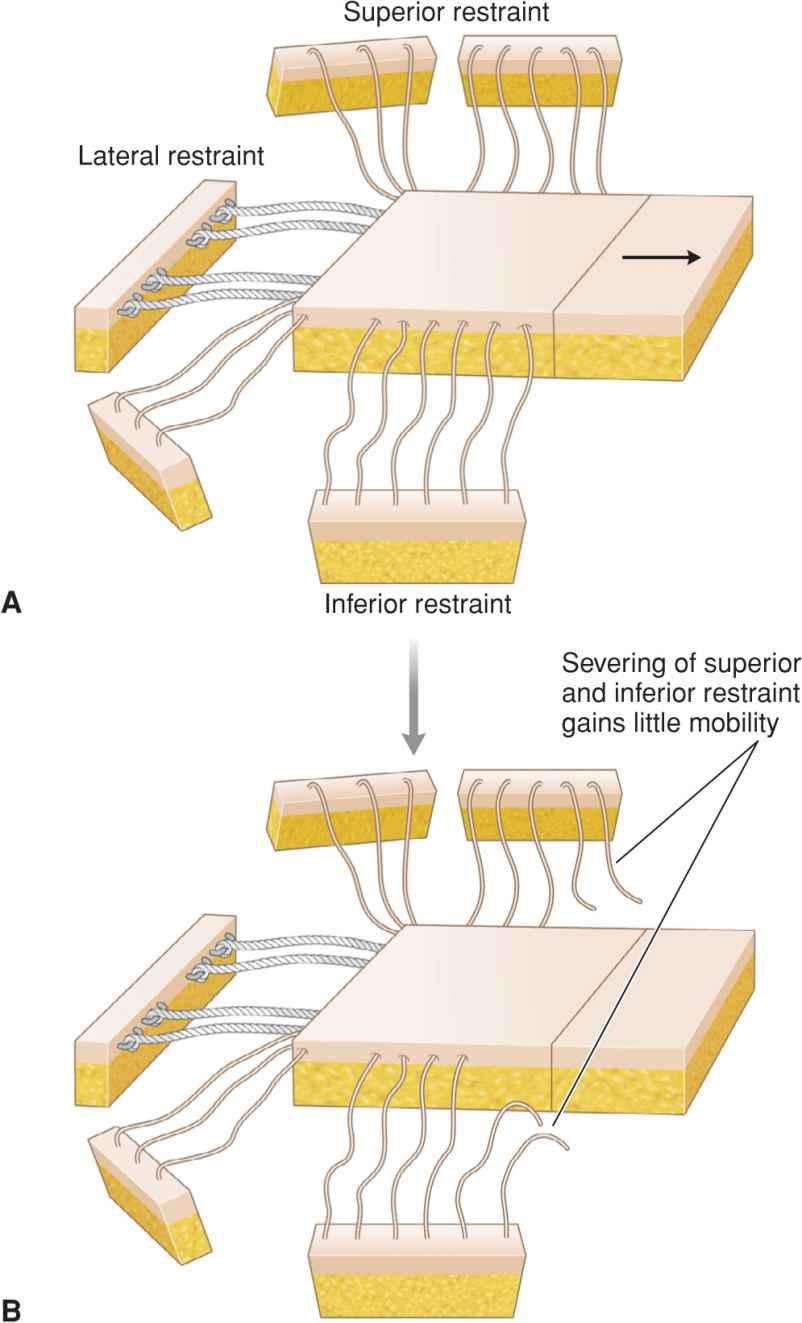
The amount of tension release achieved in any side-to-side closure is a function of intrinsic tissue properties, flap length, and undermining.2,3 Two undermining components exist: (1) undermining from the leading edge of the flap back to the pedicle and (2) undermining beneath the pedicle. These maneuvers release the advancing flap from the restraint of the underlying host bed (Fig. 2.2). Such deep restraint is transmitted via the intralobular septae of the fat from other limiting structures such as the fascia, muscle, or bone. The greater the undermining, the more motion may be achieved. Undermining does disrupt the vertical perforating vessels which nourish the flap. A balance must therefore be reached between tension release and vascular deprivation.
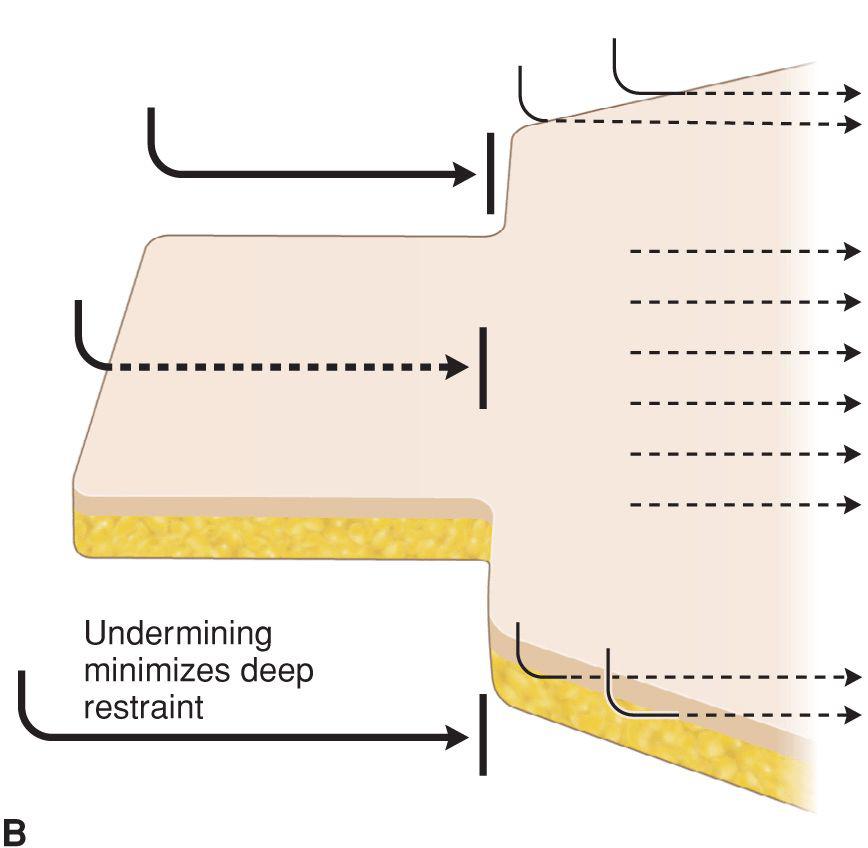
Figure 2.2 (A) External restraints on an advancement flap include lateral, deep, and superior/inferior tension vectors. (B) Undermining beneath the flap releases deep restraint. Undermining the pedicle increases tension release to a smaller degree
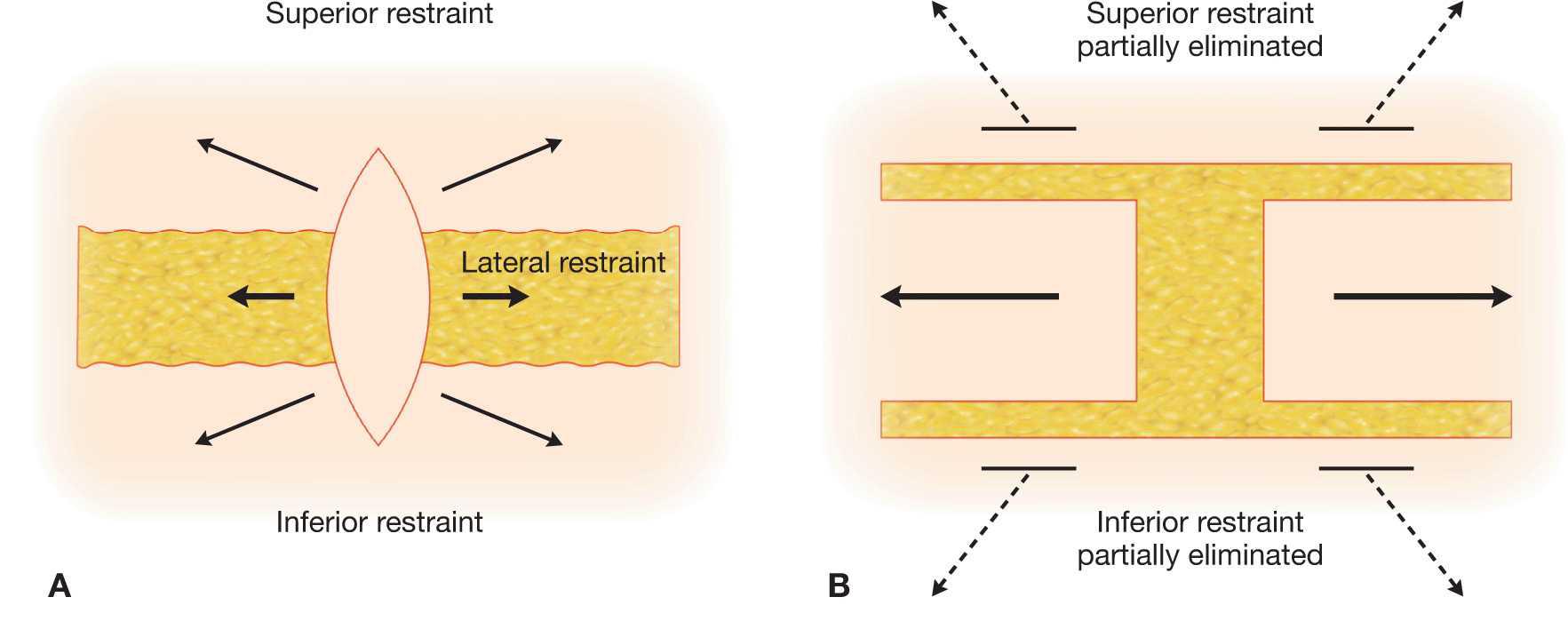
The unique tension release afforded to the advancement flap occurs through the partial elimination of the tissue drag or restraint existing superior and inferior to the flap. Fusiform closures have broad pedicles and are limited by lateral tension vectors and by restraint generated by tissues superior and inferior to the closure defect. These restraint vectors are significantly smaller in magnitude than the primary 180° lateral restraint vector but are distributed along the entire length of the fusiform tissue edge. They are eliminated along the length of the advancement flap edge by the incisions used to create the flap. The vectors re-exert their influence, however, on the flap pedicle and on points proximal to the pedicle location (Fig. 2.3). These secondary force vectors are eliminated along the length of an advancement flap. It is intuitive that a longer flap achieves a greater degree of superior and inferior tension release, and this has been born out in experimental models. The clinically relevant question is whether increasing the length of an advancement flap in vivo will significantly increase mobility. If the contribution of lateral restraint is overwhelming as compared with superior and inferior restraint, further flap lengthening will have little or no effect.
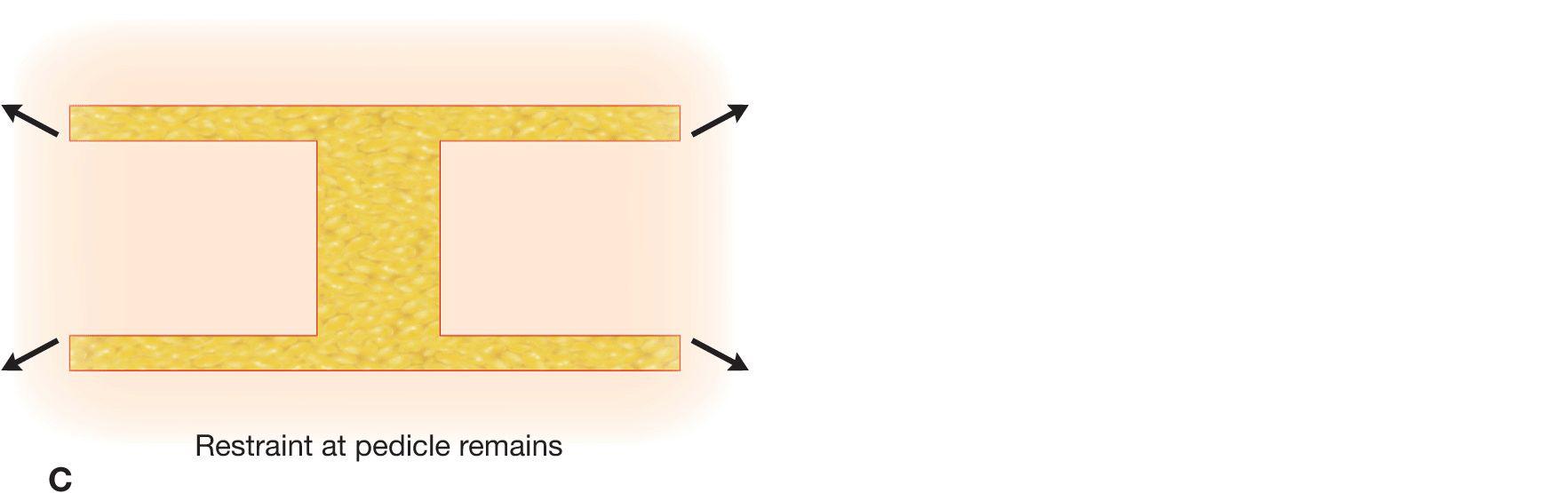
Figure 2.3 (A) An elliptical closure is restrained by lateral and superior/inferior tension vectors. (B) The incisions that create an advancement flap release superior and inferior tethering. (C) The pedicle of an advancement flap is still restrained superiorly and inferiorly
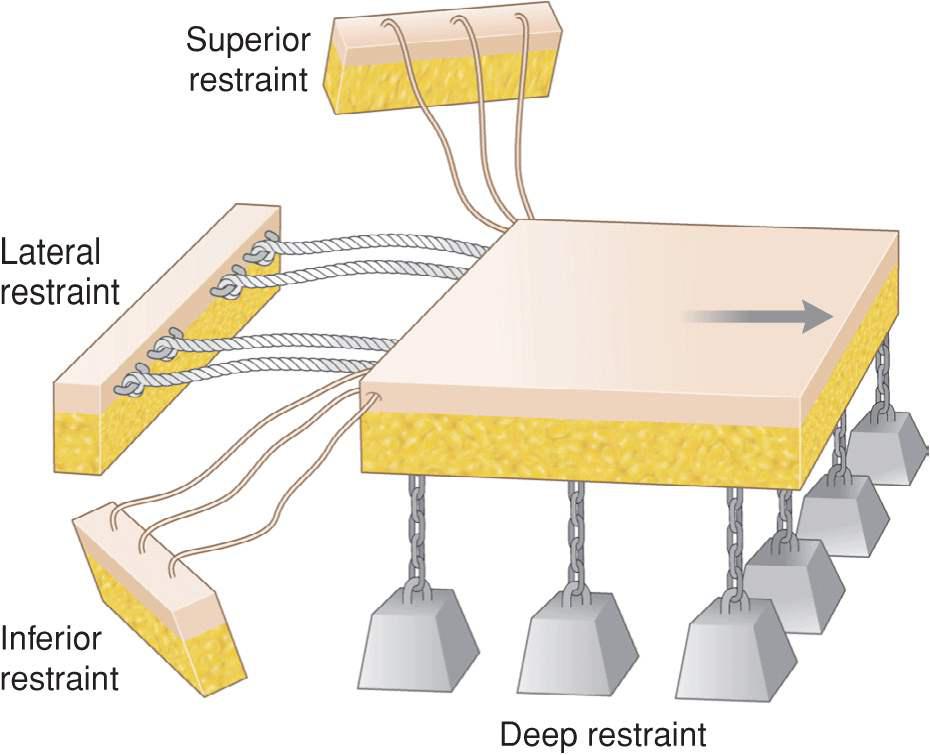
An advancement flap is biomechanically restrained by three extrinsic elements: (1) lateral restraint, (2) deep restraint, and (3) superior and inferior restraint (Fig. 2.4). The intrinsic elasticity or inelasticity of the flap tissue must also be factored into the mobility evaluation. Often, in terms of force magnitude, lateral restraint is of primary importance, deep restraint is the next most significant, and superior and inferior restraint is limited. This is of course site specific. Lateral restraint cannot readily be diminished and is the same as would be encountered with a direct linear closure. Deep restraint is freed by appropriate undermining. Superior and inferior restraint may be decreased by judiciously increasing flap length—up to a point (Fig. 2.5).
Figure 2.4 Mechanical model of advancement flap. Lateral and deep restraints are typically more significant than superior/inferior restraint
Figure 2.5 As an advancement is lengthened, elements of superior/inferior restraint are severed
For any set flap thickness, there exists a noncalculable limiting flap length beyond which a flap becomes nonviable. Although the accepted length-to-width ratio of 3:1 is generally useful, it is not inviolate. One may not progressively increase flap length by proportionally increasing flap width, unless the vascular flow input is geometrically rather than linearly increased. When this unpredictable site-specific maximum length is reached, extension of length is only achievable by including deeper tissues in the flap pedicle. This adds large caliber vessels to the flap pedicle, which in turn increases blood flow by a factor related to the fourth power of the radius of this vessel.4
From a practical perspective, there is an element of empiricism in how an advancement flap should be designed and elevated. The flap pedicle width is generally defined by the operative defect size. By pushing the defect edges in a side-to-side fashion with firm finger pressure, the feasibility of using advancement flaps is determined. If the wound cannot be mostly closed with forceful pushing, the lateral restraint may be overwhelming and an alternative closure needed. If advancement closure appears feasible, a choice should be made between using a fusiform maneuver and an advancement flap.
An advancement flap should be considered primarily as a mechanism to redistribute dog-ears, with a secondary lesser component of increased tissue mobility. The initial flap length is chosen to selectively translocate the dog-ears or minimize their visibility by suturing, using the rule of halves. For a classic unilateral rectangular advancement, the 3:1 length-to-width ratio may be gingerly approached but rarely exceeded. If vascular viability is in question, the level of flap undermining and concomitant flap thickness may be deepened to add larger caliber vessels to the pedicle; however, inclusion of fascial layers may actually inhibit mobility.
Once the flap has been delineated, undermining is carried out to the base of the pedicle. Closure tension is tested. If further release is required, undermining beneath the pedicle is performed in small increments. Once the extent of deep release is established, the superior and inferior release may be tested by incrementally increasing flap length. Since increasing the length of the flap only releases superior and inferior tension, flap lengthening should only be attempted if superior and inferior restriction contributes to the limitations on mobility or if dog-ear displacement takes precedent. In many instances, lateral restraint is so great that minimal or no tension exists on the superior and inferior vectors, and the purpose of the superior or inferior incision is solely for dog-ear redistribution (Fig. 2.6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree