Transposition Flaps
INTRODUCTION
A transposition flap is elevated from an area of laxity, lifted over an adjacent area of tissue, and transposed into an operative wound. Even more so than with rotation, transposition flaps accomplish tension redirection and redistribution.1 Adjacent laxity is tapped into to mobilize and transfer tissue from an area of laxity to an area of “need.” Transposition flaps are able to redirect tension vectors completely perpendicular to the needed primary motion of the repair, and as such can literally push tissue into a wound in order to avoid tension on a crucial structure or free margin. The prototype of this flap group is termed the rhombic design.2–7 Other commonly utilized transposition flaps include the banner or unilobed flaps such as the single-staged nasolabial flap, the bilobed flap, the trilobed flap, and the 30° angle flap.
Transposition flaps are often able to close an operative wound with a smaller reconstruction than a rotation or advancement. The lines from transposition flaps tend to be broken up and multidirectional. This can be either an advantage or a detriment, depending on the application. In areas of great convexity such as the repair of a defect along the jaw line, the shift in direction of a transposition flap can ameliorate the transition over a sharp protuberance. In areas of concavity such as in the medial can-thus, the Z-shape of a transposition flap can redirect tensions and prevent tenting and web formation. Elsewhere, however, such as on the mid cheek, a transposition flap can leave a complex geometric pattern that can be highly distracting.
A transposition flap is, in essence, a logical modification of a rotation flap. The donor site for a transposition acts much as a back cut, and the flap transposes by rotational motion on a pedicle at its base. The same principles apply to transposition, and some of the same oversizing modifications discussed in Chapter 3 are applied herein.
RHOMBIC FLAP HISTORY
Although this is not a historical text, it is worth reiterating the contribution of Alexander Limberg who in 1963 published a treatise on the repair of rhomboidal surgical wounds with rhombic transposition flaps. Although in practice, there are some deficiencies in the Limberg design of the classic rhombic transposition, its development was at the forefront of modern surgical reconstruction and stands as a great achievement in the field of reconstructive surgery.
RHOMBIC FLAP BIOMECHANICAL DESIGN
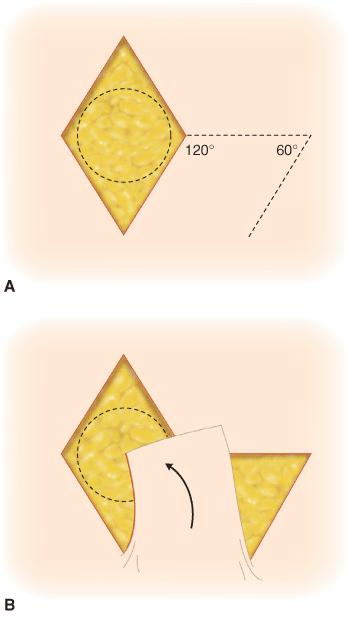
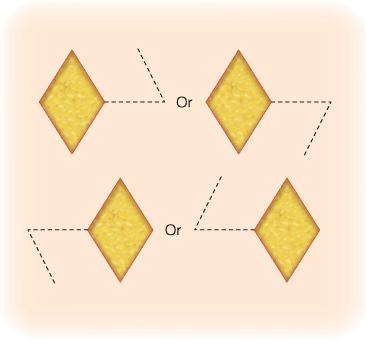
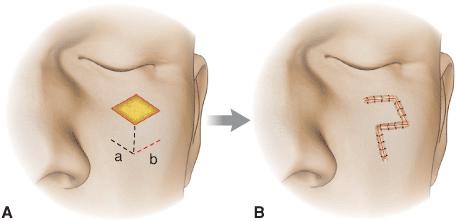
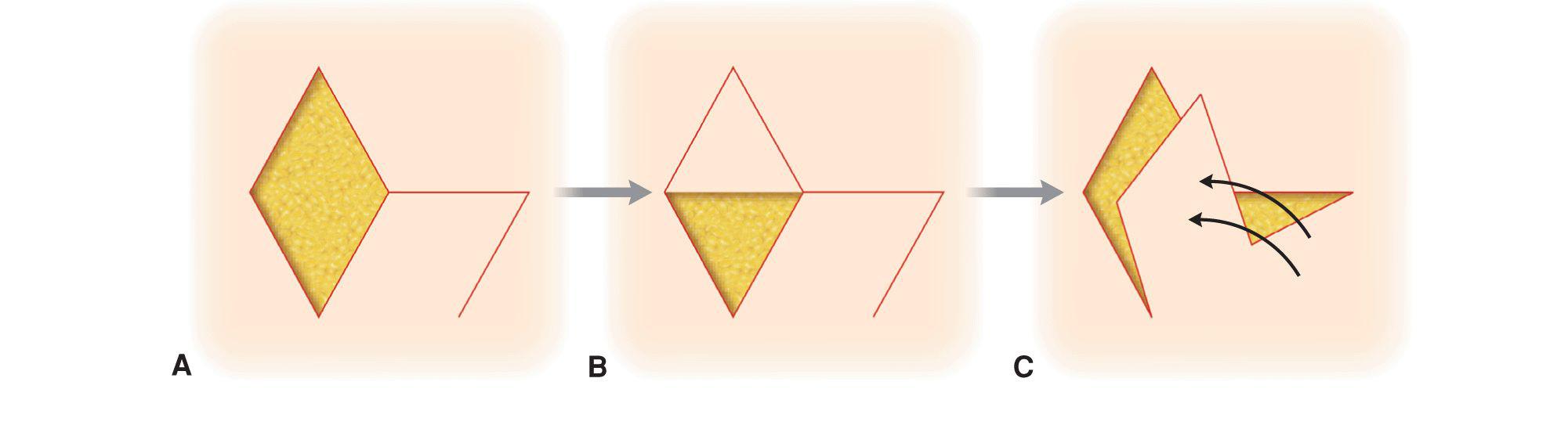
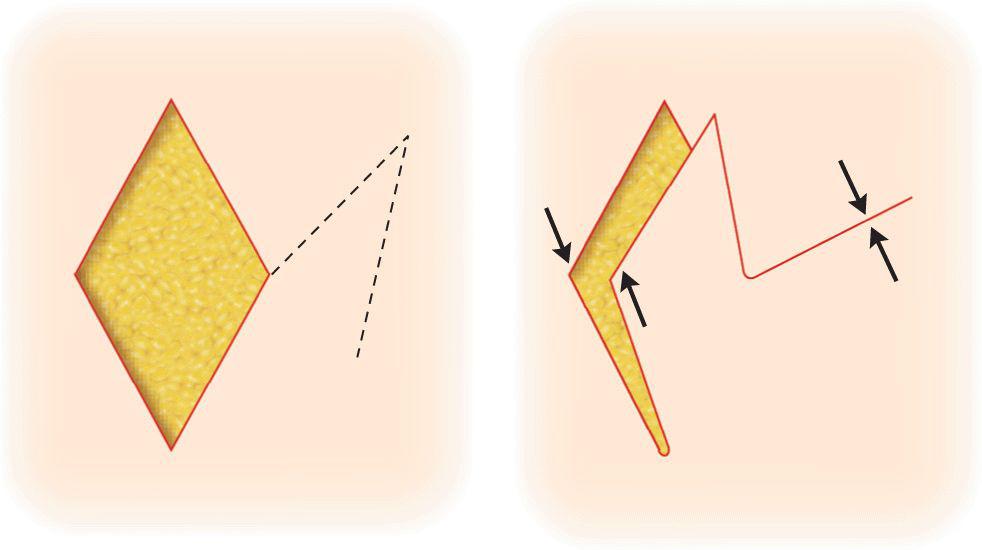
The classic rhombic flap (Fig. 4.1) is constructed around a geometric four-sided defect of equal side length, and tip angles equal to 60° and 120°. It is formed by extending the short diameter of the defect beyond the flap for a length equivalent to one of the sides. The flap is then created by drawing a line from the free end of the extended short diameter, parallel to one of the existing sides of the defect. In this manner, the first angle of the flap, or the takeoff angle, is 120° and the tip angle equals 60°. Therefore, for any rhomboid defect, four flaps are available for use (Fig. 4.2). The optimal rhombic flap will take advantage of regional laxity in closure of the donor defect and avoid anatomic distortion. This choice is decided by examining the favorable incision lines; otherwise known, for want of a better term, as relaxed skin tension lines (Fig. 4.3).8 Ideally, two sides of the rhombic defect are oriented perpendicular to the skin tension lines, thus, allowing the secondary operative wound to be closed along them. Two of the four possible flaps generated from the defect will close along favorable incision lines. Therefore, the defect with its two appropriate flaps and the mirror image of the defect, with two additional flaps, are available for use. The choice depends on which will minimize closure tension and distortion.
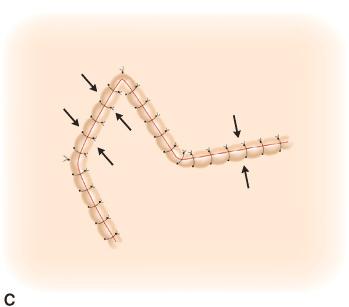
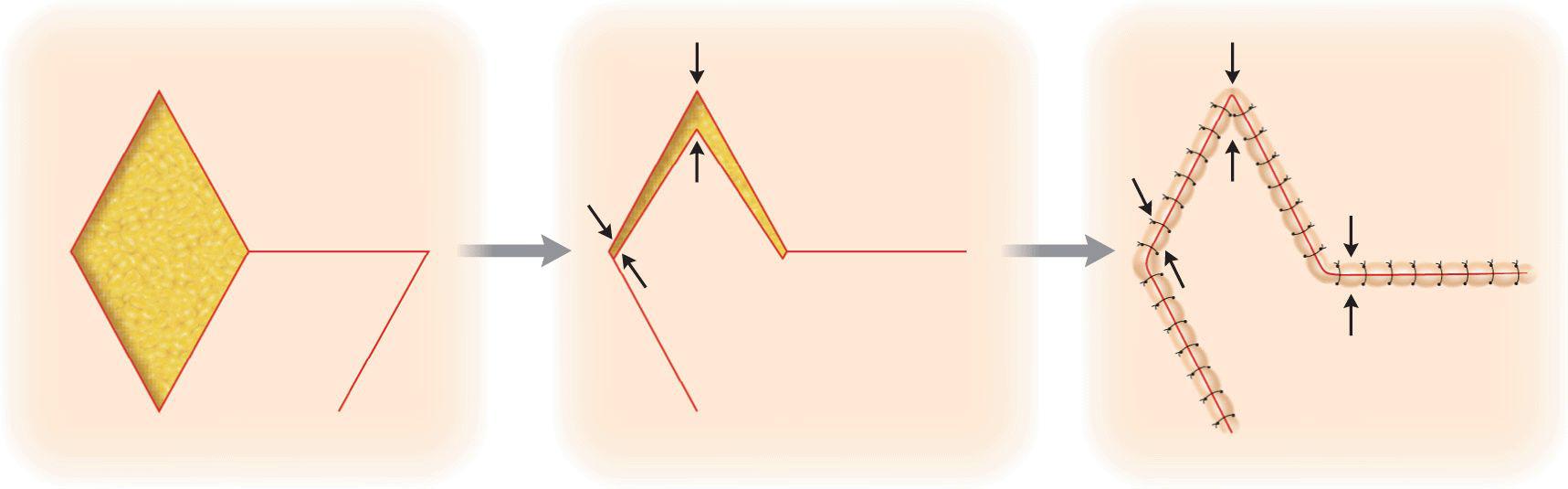
Figure 4.1 Classic rhombic transposition flap. (A) Classic rhombic flap design. (B) The flap is elevated and transposed into place. (C) Tension is redirected as the wound edges are approximated
Figure 4.2 For a given rhombic wound, four flap configurations are possible
Figure 4.3 When feasible, the secondary defect from a rhombic flap should be closed along relaxed skin tension lines. (A) Rhombic design “a” will close the secondary defects along relaxed skin tension lines (B). Closure is more facile in choice “a” due to lower tension vectors perpendicular to facial lines
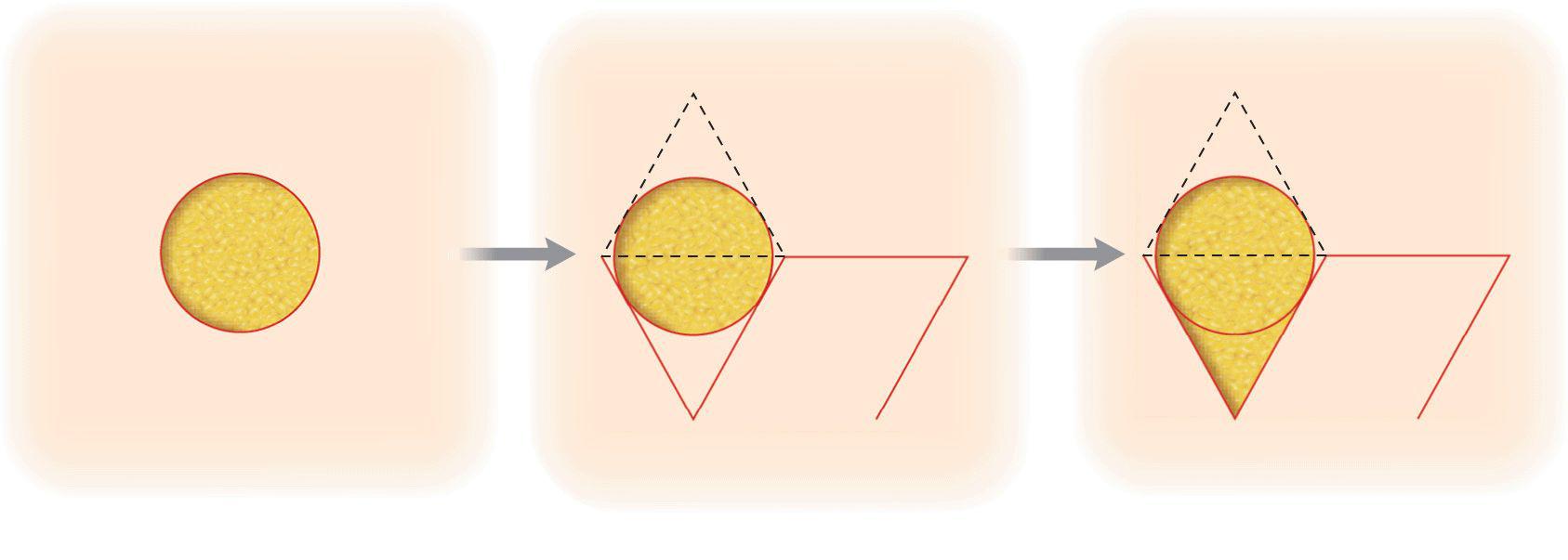
The popularity of the rhombic flap led, for a time, to the excision of lesions based on a rhombus. In other words, the reconstruction was predetermined and this in turn dictated the excision to be undertaken. This was a foolhardy approach and led to excess tissue excision, positive margins and repeat surgeries. Moreover, it led to the creation of flaps that were fundamentally challenging to close due to the complexities associated with the rigid rhombic repair design. Following modern methods of tumor extirpation, most operative wounds are round, oval, or irregular in shape. Such wounds are often closed readily without conversion of the defect to a rhomboid shape, and in many instances the wound is actually easier to close than a rhombus. A circular wound, for example, may be used with a 60° rhombic flap. The rhombic design may be drawn around the circular wound to allow planning and orientation of the flap. The triangular ends, however, are not excised unless dog-ear correction is required. Often, because of skin elasticity, the circular wound will drape around the flap tip and permit closure without significant skin excision (Fig. 4.4).
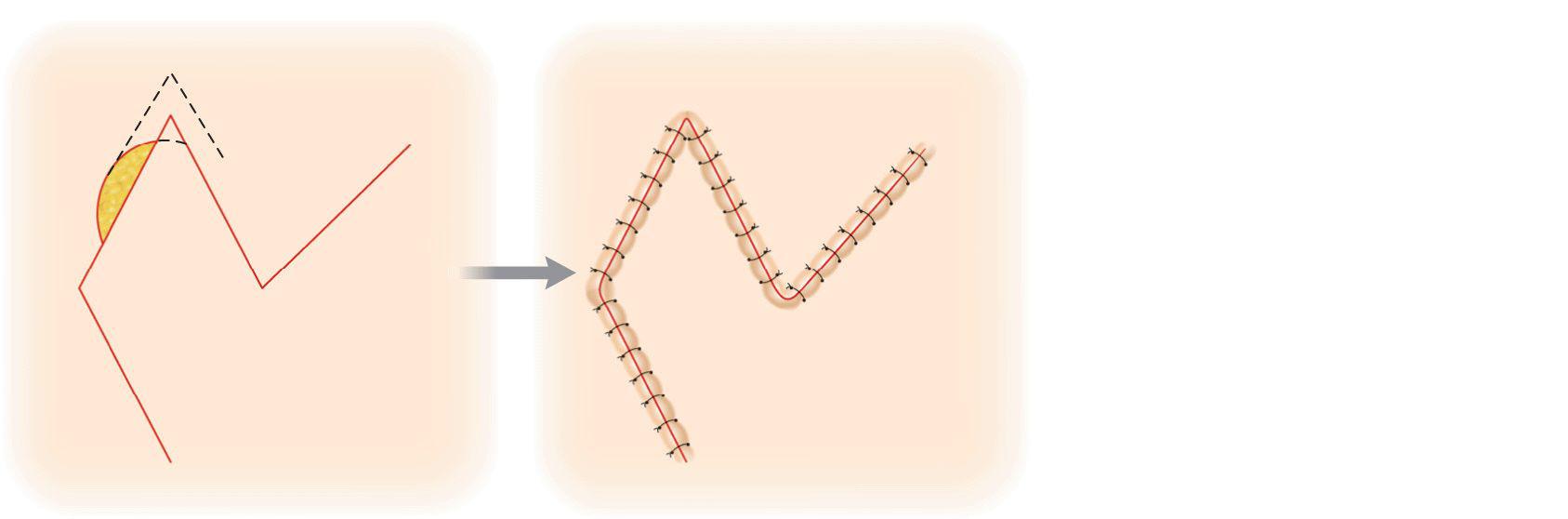
Figure 4.4 A rhombic flap may be constructed around a circular defect. The flap and/or defect is trimmed appropriately to achieve a good fit
While the design of a classic rhombic flap is complex, the dynamics of rhomboid flap motion are even more challenging to master. Although an unmodified Limberg flap is mathematically correct, the intrinsic properties of the skin do not usually allow for an effortless closure. Instinctively, one might assume that since flap and defect are of equivalent size and shape, one could place the flap in position without tension. However, the restraint on the flap by the pivot point at the pedicle prevents this from occurring (Fig. 4.5). Even though the flap motion is termed transposition, and indeed the flap is lifted and transposed over adjacent tissue, a primary motion of the flap is rotation based on a fixed pedicle. Elevation of the flap by closure of the donor defect does not eliminate the limitation of the rotating movement. Therefore, the rhombic flap is subject to some of the same movement restraint as a rotation flap. This means that the leading flap tip will not quite reach the recipient angle without some movement of the recipient tissue toward the flap. If this surrounding tissue is mobile, associated structures (eyelids, nasal rim, lips) will potentially be placed under traction. If the tissue is not moveable, the flap tip will be pulled forcefully into the angle that risks tip ischemia or necrosis. A limited and smaller recipient movement is necessary to oppose the secondary tip and angle. Therefore, with classic rhombic flap design and execution, two major and one minor forces are noted: (1) major tension closing the secondary operative wound, (2) significant tension on the site of closure of the leading tip and recipient angle of the flap, and (3) a small amount of tension on the secondary tip and angle.
Figure 4.5 Although rhombic flaps are geometrically correct, pivotal restraint (P) often keeps the two flap tips from reaching their destinations. Forcible advancement (arrows) is then needed to achieve wound closure
Tension Modifications
Modifications of transposition design and execution are able to overcome some of the potential drawbacks of the classic rhombic flap. To understand how the flap should be modified it is beneficial to reexamine the dynamics of a rotation flap. The mechanics may be distilled and simplified by considering the rhombic design as a variant of a rotation flap with a back-cut (Fig. 4.6). One may conceptualize the lower half of the rhombic defect as equivalent to the classic triangularized wound of the rotation flap. The upper portion of the rhombic is really a divot, or “receptacle,” to receive the triangular tip of the back-cut. Continuing this model analogy, the defect left by the back-cut (the rhombic donor defect) is closed primarily. This is the same mode of back-cut closure used in the dorsal nasal flap. The rhombic flap then goes through classic rotation. Although the back-cut tip transposes over surrounding skin, the dynamic motion of the flap is rotation. With classic design, as with a rotation flap, pivotal restraint will only allow the flap to reach its destination under some tension. Forcible advancements of the long flap tip and the secondary tip are required in most cases. In clinical practice, this tension is often visible as a clearly demarcated area of hypoperfusion of the flap extending across the flap (Fig. 4.7).

Figure 4.6 While technically a transposition flap, a rhombic flap can be conceptualized as a short rotation flap with a large back cut. (A) Rhombic flap design. The entire flap can be considered a large back cut. (B) The upper triangular portion of the Limberg variation is a recipient for the tip created by the back cut, and the lower shaded portion of the wound is closed by rotational motion. (C) The upper portion of the flap is being rotated and transposed over tissue, while the lower portion of the flap is undergoing rotational motion. (D) Clinical photos demonstrating rotational component of rhombic transposition. Note curvature of the preoperative straight lines as the flap transposes and rotates
Figure 4.7 Transient ischemia of distal rhombic flap is noted secondary to forcible advancement of both tip points
Reducing Primary Motion Tension Vectors
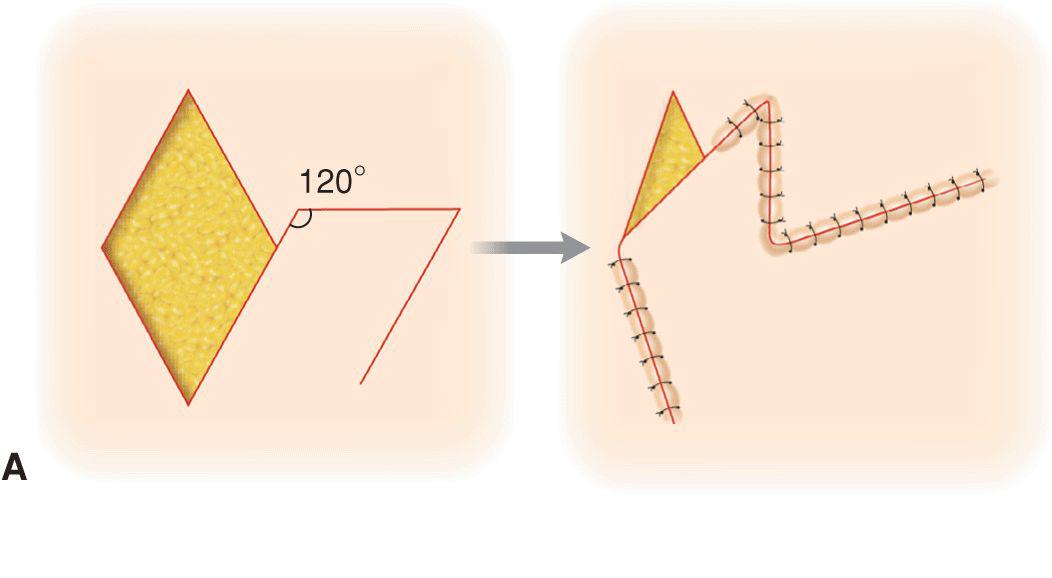
Several modifications of the standard rhombic flap allow for the primary operative wound to be closed under less tension. A straightforward design modification is to make the leading edge of the flap longer than would be geometrically predicted. If the leading edge of the rhombic flap is elongated, the flap tip meets its recipient angle without tension (Fig. 4.8). If only the first limb takeoff point is addressed, there is still pivotal restraint hindering the secondary tip from reaching its target. If the takeoff flap angle is made slightly more obtuse, that is greater than 120°, the secondary flap tip will close under less tension as well (Fig. 4.9). Similarly, if the secondary limb of the flap is extended in length, the secondary flap tip easily meets and may overshoot the secondary recipient angle, and some trimming of the flap as it overlaps the defect may be required. Effectively enlarging the flap eliminates tension on flap tips and recipient wound while creating a greater tension of secondary motion and tension. These modifications are valuable when the flap is elevated in a loose area of skin such that closure of the secondary operative wound is readily accomplished. Such oversizing of a flap can be particularly important when the defect is adjacent to a free margin such as the eyelid, and all tension must be directed perpendicular to the primary motion of closure.

Figure 4.8 (A) By oversizing the leading edge of the rhombic design, the tip of the flap can overcome pivotal restraint and may be transposed into place under little to no tension. The trade off is greater closure tension and a length mismatch in closure of the secondary operative wound. (B) Modified rhombic flap design on the temple. Note that when the secondary defect is closed the flap easily reaches, and in fact overshoots, its destination
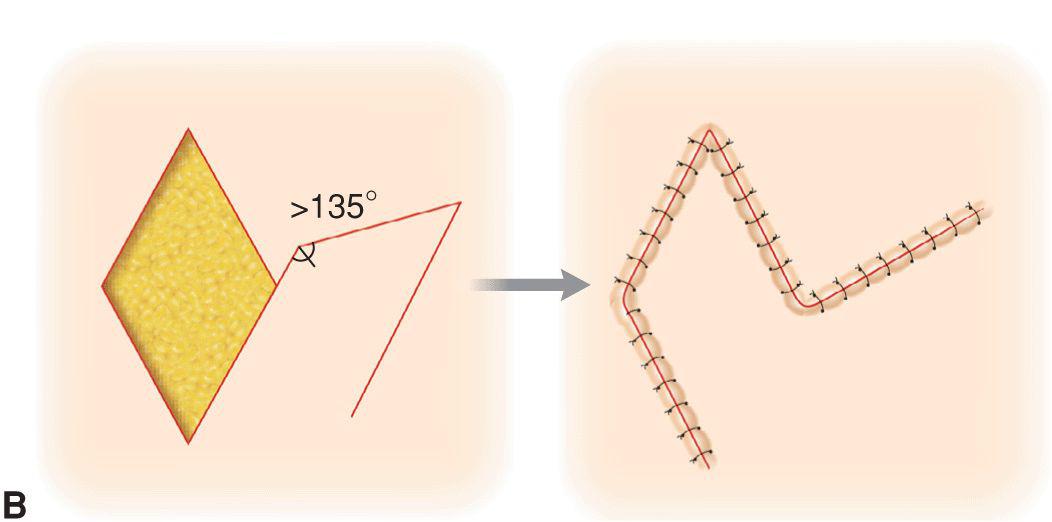
Figure 4.9 Effects of oversizing the leading edge and increasing the flap takeoff angle: (A) With leading edge elongated the first tip closes readily. The second tip still lags. (B) By increasing the flap length and the takeoff angle beyond 120°, both tips of the flap reach their destinations under less tension
Sharing Tension between Primary and Secondary Motions
Webster 30° angle flap
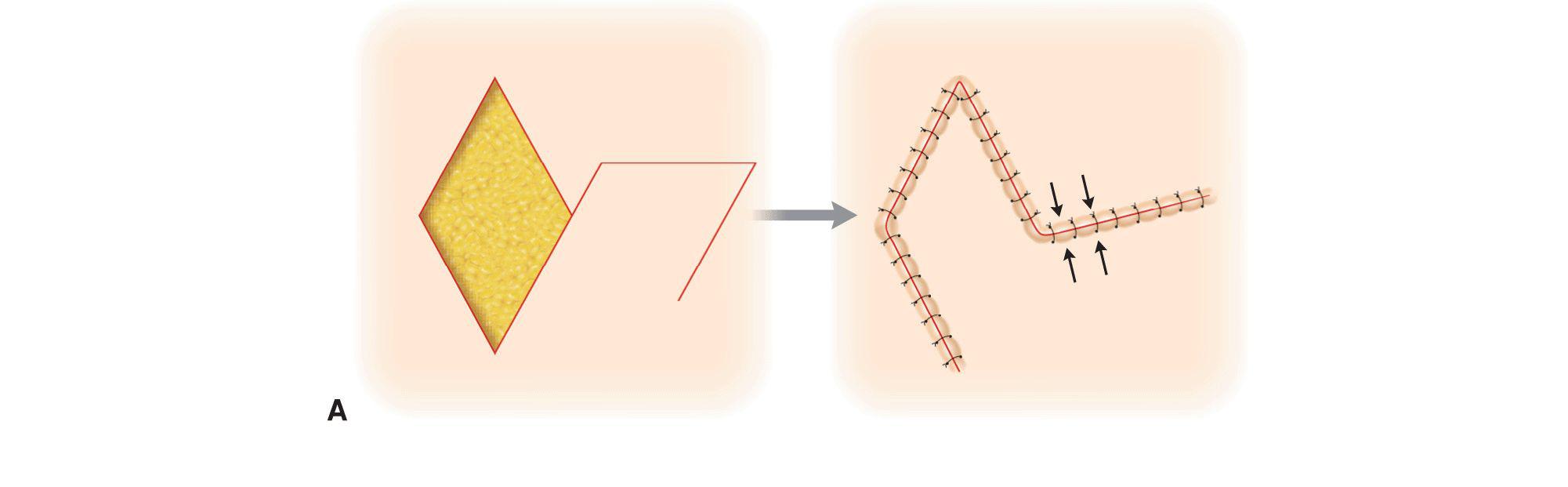
As noted, although imperfect in vivo, the classic Limberg flap does reduce tension on a primary closure by redirecting tension vectors to a secondary motion. If a recipient area is somewhat lax, and adjacent tissue motion will not pull on a free margin, tension may be more evenly dispersed over the primary and secondary operative wounds. This may be achieved by decreasing the apical flap tip angle, and the most common modification is the 30° angle flap.9 In this instance, the base of the flap is only about one-half the size of the recipient defect (Fig. 4.10). The 30° angle flap can reduce tensions from pivotal restraint and minimizes the formation of a redundant tissue cone, but tension is now exerted on the flap in a side-to-side manner as the original wound is closed. Because the flap pedicle width is shortened by decreasing the tip angle, side-to-side tension may lead to ischemia. Conversely, if laxity is present, simple fusiform closure of the original defect may have been the preferred option.
Figure 4.10 A 30° angle transposition flap is only about one-half as wide as the defect. This creates lateral tension on the flap at closure and is only feasible when the surrounding tissue can contribute to horizontal motion
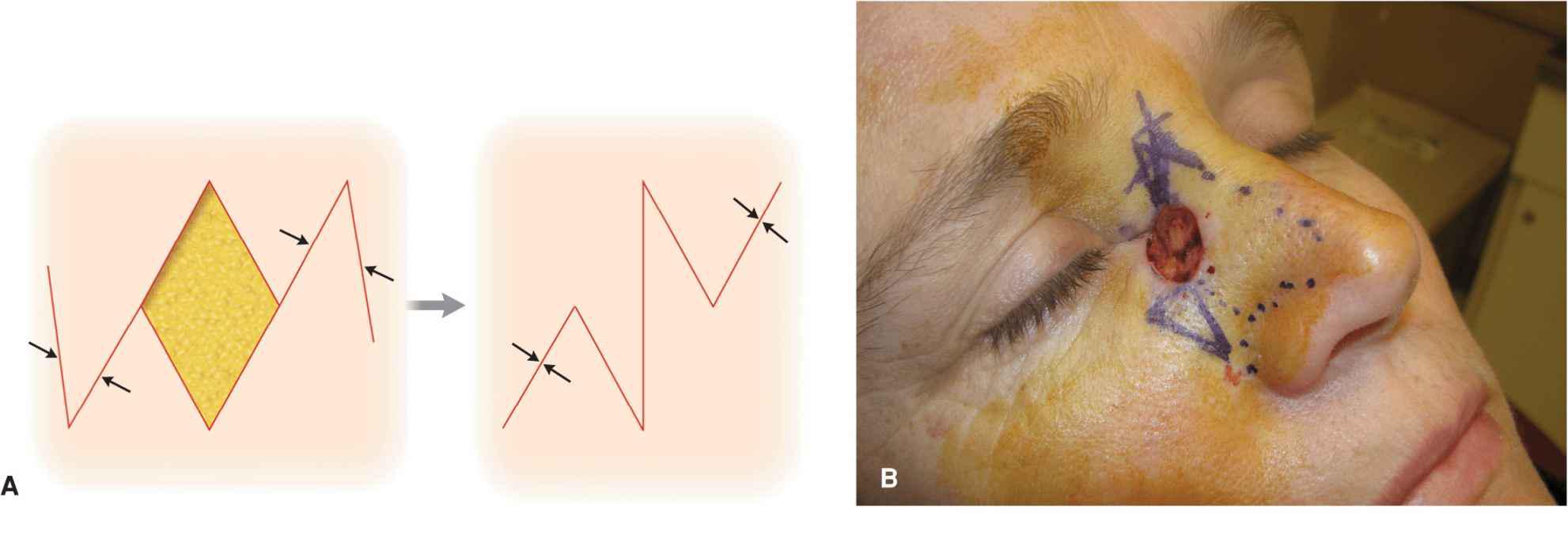
Flaps with a tip angle of less than 60° may be more useful when combined as opposing adjacent tissue transfers (Fig. 4.11). In cases where a single rhombic flap may not recruit adequate laxity, two flaps may be designed to draw from different tension vectors.10–14 Two opposing full size flaps may not be needed, and in such cases the angle of each flap may be narrowed from 60° to 30° as deemed appropriate.15 Each flap is needed to close only one-half of the defect. The tension forces on the donor defects are perpendicular and are drawn from different sources. The downside to a double transposition flap reconstruction is a substantially complex scar line.
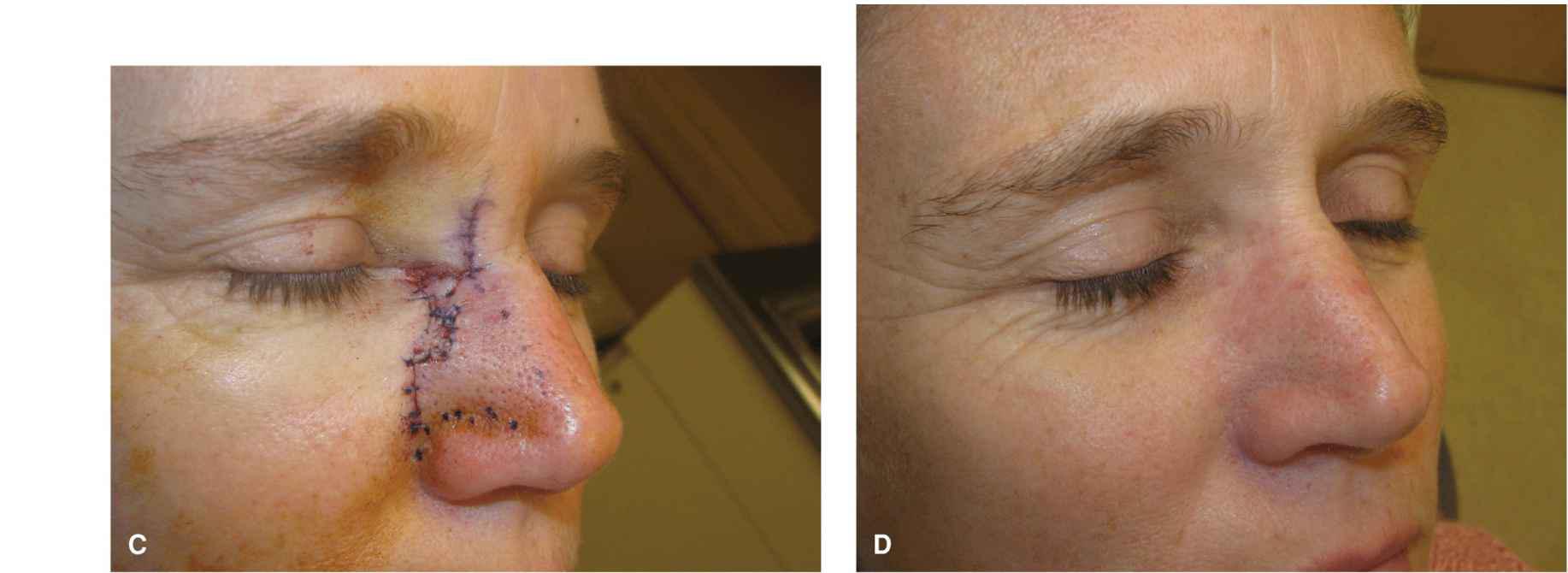
Figure 4.11 Bilateral opposed 30° transposition flaps may be used to close an operative wound. Each flap closes half of the wound. The advantages of such a repair are multidirectional tension redirection and tension redistribution, similar to an O-Z bilateral rotation flap. The complex resultant scar line is a detriment. (A) Diagrammatic representation of bilateral 30° angle flaps. (B) Operative wound and planned bilateral transposition flaps. (C) Immediate closure. (D) Repair at 6 months. There is no webbing present
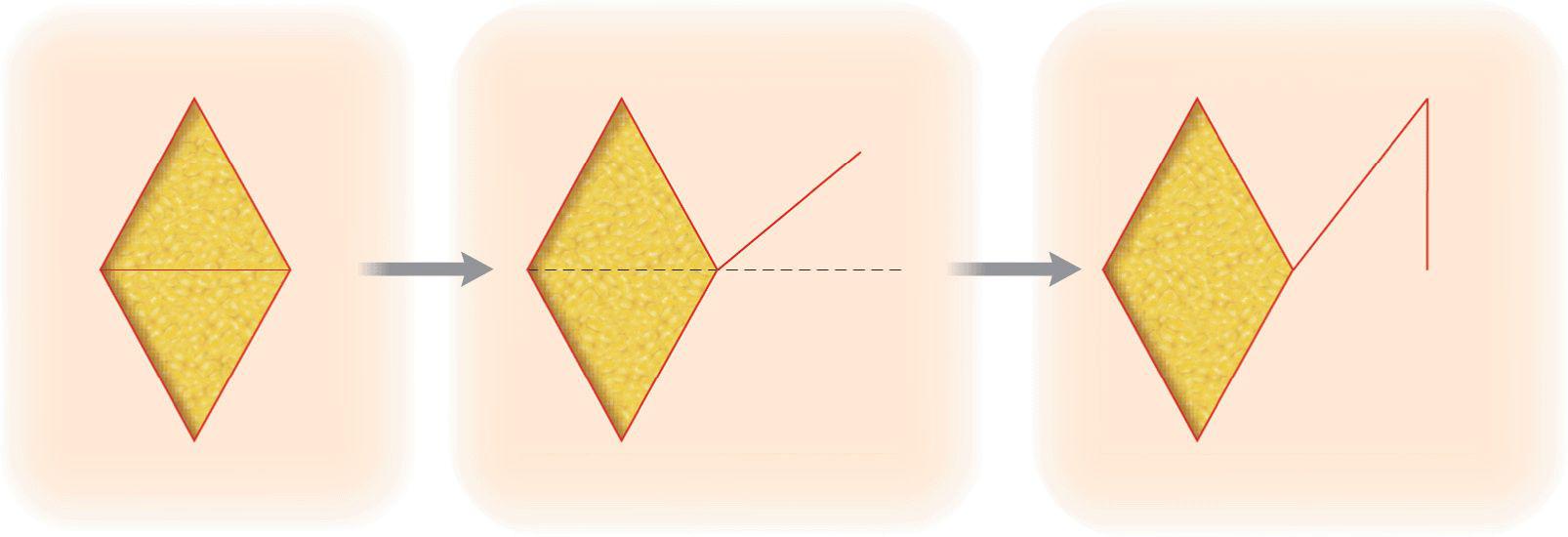
Dufourmentel flap
The Dufourmentel flap6,16 (Fig. 4.12) is a modified geometric rhomboid transposition flap that shares tension between the primary and secondary operative wounds. Its purpose is to decrease vertical tension by tolerating a higher degree of horizontal tension. The Dufourmentel flap is a complex repair to understand. The defect that receives the flap is again rhombic, that is, four sides of equal length with tip angles of 60° and 120° (two equilateral triangles sharing a common base). The first step in the Dufourmentel flap is to extend two lines from the rhombic defect. The first is an extension of the short axis or “diameter” by doubling. The adjacent side of the rhombus is then extended a similar length. The angle created by these two extended lines is bisected, and a line is drawn along this bisection for a distance equivalent to side length. From the end of this bisection line, a second line is dropped so that it is parallel to the long axis of the rhombic defect. This completes the flap.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree