Rotation Flaps
INTRODUCTION
Wounds that are too tight to close in one direction can frequently be repaired by redirecting tension vectors away from the primary motion. Rotation is the simplest method of redirecting tension vectors and reducing wound closure tensions.1 The design of a traditional rotation flap utilizes a curvilinear incision along an arc adjacent to the primary surgical wound. As a rotation flap is executed, the direction of wound closure tension is effectively changed. Rotation flaps partially or completely redistribute and redirect closure tension from a primary defect to a secondary arciform defect.2,3 Laxity of the adjacent tissue allows the flap to be rotated into the primary defect, and the tension vector is reoriented in the direction of the secondary defect or secondary motion of the flap. Rotation flaps also allow for displacement of dog-ears to more favorable locations. Well-designed rotation flaps create scar lines that are hidden along facial boundaries or within relaxed skin tension lines. There are few repairs as elegant and seemingly simplistic as a well-designed and well-executed rotation flap. In practice, flaps that utilize only rotational motion are uncommon, and a simplistically designed rotation flap rarely suitably repairs an operative wound.
Rotation flaps may involve pure rotation or combinations of rotation and advancement. A common clinical misconception is that rotation flaps borrow lax tissue from a curvilinear donor area. While laxity along the sweep of flap rotation is integral to the mechanics of the design, the crucial planning involves anticipation of tension vectors generated from closure of the secondary defect created as the primary defect is closed. The pedicle of a rotation flap and the mobility of the point of pivotal restraint are the key determining factors of the success or failure of a given repair. In any rotation flap, tension vectors may exist in multiple directions and depend on intrinsic tissue properties, orientation, design, and execution. The uniqueness of rotation flap biomechanics is, therefore, a calculated alteration of the direction of major closure tension forces.
Historically, the rotation flap was a workhorse for plastic surgeons who utilized the flap to repair large defects following pilonidal cyst removal and for the repair of finger wounds. In the past several decades, rotation flaps have found a greater use for the reconstruction of facial wounds.
BIOMECHANICAL DESIGN
Basic Construct
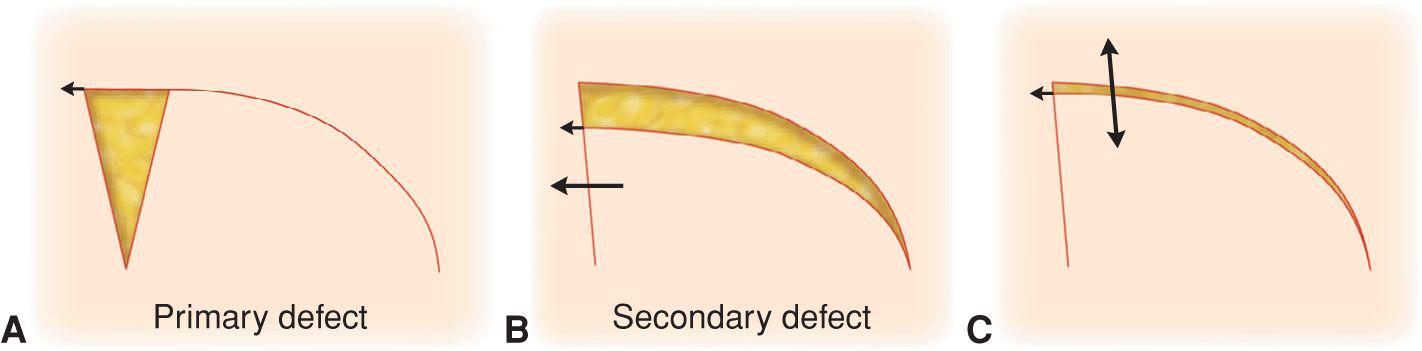
Rotation flaps may be conceptualized as involvinga primary defect, a primary tissue movement, a secondary defect, and a concomitant secondary tissue movement (Fig. 3.1). The primary defect is the original wound. The primary tissue movement involves partial or total closure of that wound by redraping of the rotated flap. As the primary defect is closed, usually under minor tension, a secondary defect is created along the curvilinear sweep of the flap. The closure of this novel secondary defect involves a unique secondary tissue movement. The bio-mechanical foundation of the rotation flap is the transfer, redistribution, and redirection of some fraction of tension from closure of the primary defect to closure of the secondary defect. This function comes into play when side-to-side closure of the primary defect is unachievable because of nonreducible tension, or when side-to-side closure has the potential to distort anatomic structures.
Figure 3.1 Classic rotation flap. As the primary defect is closed, a secondary curvilinear defect is created. Secondary flap movement closes this operative wound. (A) Classic rotation flap design with a triangulated defect and arciform closure. (B) Primary motion closes some of the original operative wound and creates a secondary defect. (C) The second defect is closed with secondary flap movement
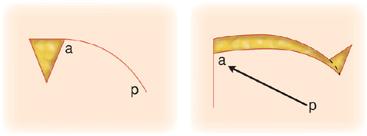
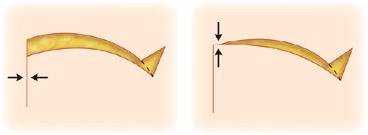
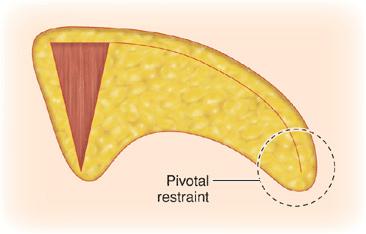
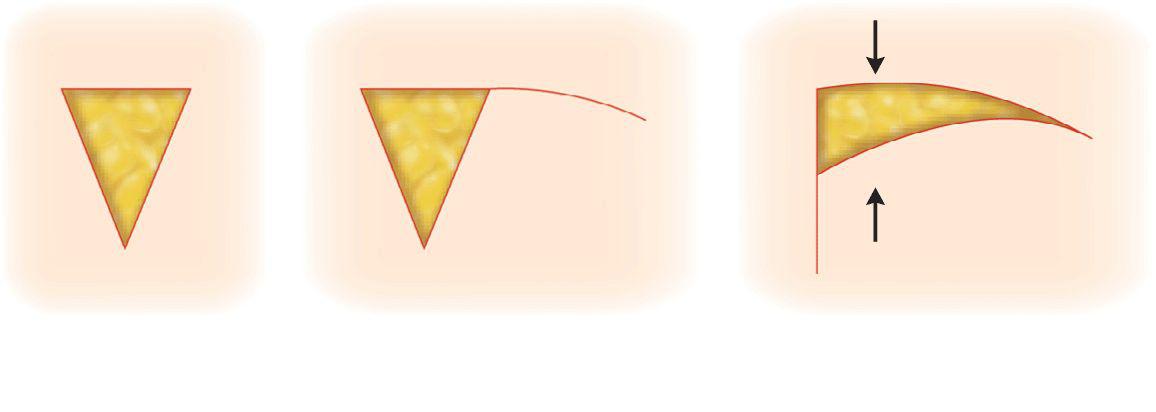
To conceptualize the dynamics of the rotation flap, it is best to start with the classic design, incorporating a triangulated defect with a smooth curvilinear flap sweep. The flap is elevated and rotated into place so that no tension exists on the leading angle, or tip, of the flap. This is known as the primary motion of the flap. Because of restraint from the pivot point of the pedicle, the flap tip will only move under minimal tension to a point below the angle designed to receive that tip (Fig. 3.2).4,5 A crescent-shaped secondary defect is now created. The closure tension is partially transferred from the vectors of the primary defect to the vectors of the secondary defect, which are directed differently from the original closure forces. If the flap tip is moved to entirely close the receptor angle, the flap movement now involves not only rotation but also upward tip advancement (Fig. 3.3). This may lead to flap tip ischemia if the surrounding skin is immobile and cannot partially move down to meet the tip. If the surrounding tissue is mobile, one must anticipate this movement since anatomic structures may be pulled or distorted. To eliminate the compensatory movement of the surrounding skin toward the flap, the leading edge of the flap can be modified so that it is longer than the defect (Fig. 3.4).6 Following this maneuver, there may be a need to trim a small amount of excessive flap tissue where it overlaps the defect superiorly. The secondary defect is subsequently closed with the appropriate adjustment of redundant tissue.
Figure 3.2 If a rotation flap is rotated under minimal tension, the flap tip does not reach the intended closure site and a secondary defect develops. This results from pivotal restraint at point p
Figure 3.3 With a standard rotation flap design, the operative defect is only closed with a combination of primary motion and secondary motion (upward advancement)
Figure 3.4 (A) The leading edge of a flap may be elongated to compensate for pivotal restraint. (B) This maneuver decreases the secondary motion needed to close the operative wound
Adjustment of Primary Tension: Release of Pivotal Restraint
Rotation flaps can successfully eliminate all or most tension along a primary tension vector. However, depending on restraint from the pivot point, the classical rotation flap may not be able to achieve primary defect closure under low tension. If the flap is restrained at its pivot point, the tip may only reach to a low point on the triangulated defect edge. While a forcible advancement of the flap tip can close the primary wound, undue tension risks tissue ischemia or distortion of adjacent anatomic structures.
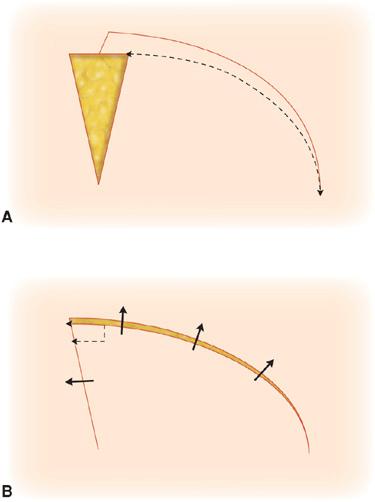
Two maneuvers assist in diminishing rotation flap tension. Undermining the flap can release deep restraint, and incorporating a backcut can release surface restraint. In order to release the pivotal motion of the flap from deep restraint, undermining must be employed beneath the flap pedicle. Rotation flaps require undermining not only of the flap pedicle but also of the point at the far extent of the rotation curvature. This point functions as a pivotal restraint and hinders both rotation and advancement components of the flap closure (Fig. 3.5). For rotations elevated above fascia, simple undermining will usually free the pivotal restraint. When a flap contains fascia, the pivotal restraint may be hindered. With caution, the fascia may be incised to allow for a greater rotational mobility. The key to remember is that, if the area of pivotal restraint remains “hung up,” the flap risks compromise or places tension in unwanted locations. Careless undermining of the pedicle may compromise the blood supply of the repair by interrupting vertically perforating vessels, but the release of restraint accomplished by appropriate undermining is integral to flap motion.
Figure 3.5 Undermining not only the flap pedicle but also the point of pivotal restraint will allow for more facile wound closure
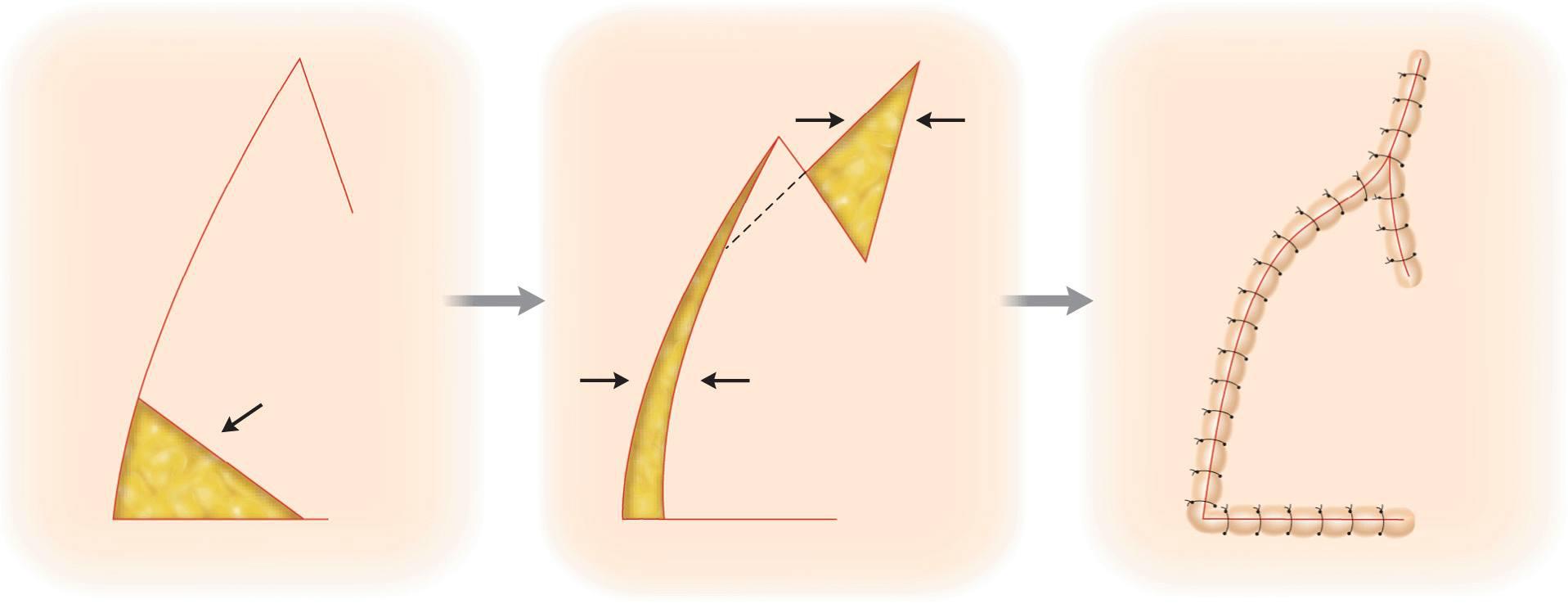
Once the subcutaneous pull is minimized, attention is directed to cutaneous factors. Tethering from the lateral pull of the pivot area may be diminished by a backcut into the flap pedicle (Fig. 3.6).7 The use of a backcut must be tempered by the fact that this maneuver may also diminish blood supply to the pedicle, this time from the horizontally oriented vascular plexus. The extent of the backcut that is safe cannot be precalculated. A more ample deep pedicle will allow for a more extensive backcut. If the deep pedicle contains large caliber vessels, the cutaneous portion of the pedicle can be substantially narrowed and an extensive backcut can be employed.
Figure 3.6 A flap backcut allows for greater release of tension and easier rotation. In this example, the backcut is closed in a V-Y fashion
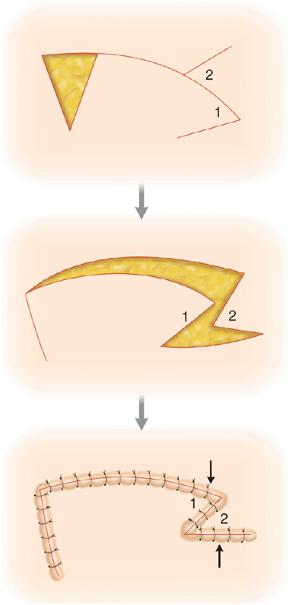
The defect created by a backcut may be closed in one of two ways: a V-to-Y closure or a Z-plasty. The traditional method used to handle backcuts is to close trailing portion of the secondary defect with a V-to-Y closure. As the flap rotates into the secondary defect, the backcut is trimmed and sutured into place, creating a “Y”-shaped closure. An alternative approach is to use a Z-plasty to close the trailing portion of the secondary wound (Fig. 3.7).8 The tension needed to transpose and bring the two triangular flaps of the Z-plasty together is perpendicular to the closure of the primary defect and coincides with the vectors of closure of the secondary defect. In order for the Z-plasty closure to be executed properly, all limbs of the Z-plasty must be equivalent in length. The Z-plasty angles are best constructed at 60°. Textbooks occasionally portray closure of the backcut by draping surrounding skin around the triangular tip. This is only a viable alternative if the surrounding tissue is substantially lax.
Figure 3.7 A backcut may be closed with a Z-plasty
The length and curvature of a rotation flap are to a certain extent designed empirically, but there is some logic that predicts the successful length and arc of a rotation.
Flap Length
Tension redistribution is a function of rotation flap length. The secondary defect created by flap rotation is both a transformation and translocation of the primary defect. The geometric configuration of the secondary defect is determined by flap length. A longer flap creates a longer secondary operative wound. The surface area of the secondary defect is equivalent to the surface area encompassed by closure of the primary operative wound. A longer secondary wound is, by definition, a narrower one, and the narrower the secondary defect, the less the tension that is required to close it (Fig. 3.8).2 Therefore, the longer the rotation, the less the tension required to close the secondary defect. A second advantage of a longer flap is a greater redistribution of tissue redundancy with less dog-ear formation. The downside of a longer flap is the size of the resultant repair. Because rotation flaps require long incision lines to achieve appropriate flap motion, in many facial locations, there are other flap repairs that are more palatable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree