■ Additional imaging studies may be required depending on the functionality of the tumor (metaiodobenzylguanidine [MIBG] for some pheochromocytoma patients, adrenal vein sampling for hyperaldosteronism, etc.).
■ Fine needle aspiration or core biopsy is not recommended if adrenocortical carcinoma is questioned. FNA may be useful if metastasis to the adrenal gland is in the differential and the adrenal tumor is the most accessible site of metastasis in the setting of multiple sites of metastatic disease. If biopsy is performed, it is imperative to first biochemically rule out pheochromocytoma.
SURGICAL MANAGEMENT
■ Adrenal tumors, if benign appearing by imaging criteria, nonfunctional, and therefore not requiring resection, should be reevaluated with at least one additional CT scan or MRI 6 to 12 months after the initial imaging study to ensure stability in size and internal imaging characteristics. Some advocate for a longer period of follow-up imaging for 2 years with reevaluation of biochemistry for 4 years.1
■ Functional tumors leading to hormone excess, indeterminate masses, and those suspected of being adrenocortical carcinoma or isolated metastatic disease from another primary tumor without evidence of widespread metastatic disease should be removed.
Preoperative Planning
■ The surgeon must evaluate available imaging studies for possible adrenocortical carcinoma or tumor involvement of adjacent organs, vessels, and lymphadenopathy. An open posterior approach is not optimal for removing adrenocortical carcinomas or large tumors, as the working space is limited by the rib cage and does not allow for multivisceral resections. These types of tumors should be approached by an open anterior or thoracoabdominal approach.
■ The surgeon should evaluate the position of the adrenal gland with respect to the overlying rib that will need to be resected as well as any visible vasculature supplying or draining the adrenal gland.
■ The risks, benefits, and alternatives to surgery are discussed with the patient including potential need for steroid supplementation in the postoperative setting. Patients with pheochromocytomas should be adequately alpha blocked and volume replete. Beta blockade may also be necessary. A potassium level should be checked the morning of surgery and treated as necessary in patients with Conn’s syndrome (hyperaldosteronism).
■ Routine prophylactic antibiotics and deep vein thrombosis (DVT) prophylaxis are administered prior to surgery, and sequential compression devices are applied.
■ A general endotracheal anesthetic is administered.
■ Common to all approaches, skin preparation with clipping rather than shaving is prepared, and the surgical area is prepped and draped in a sterile fashion.
Positioning
■ Patients are intubated and a Foley catheter is placed prior to placing the patient in a modified prone position. Several methods for positioning may be used, including use of the Wilson frame, the Cloward surgical saddle, gel rolls, and flexion of the table (FIG 2). All of these have the common goal of creating a gentle flexion of the spine. Space is also created for the abdominal contents to shift away from the retroperitoneum.

■ All pressure points are padded appropriately.
TECHNIQUES
LEFT ADRENALECTOMY
Exposure
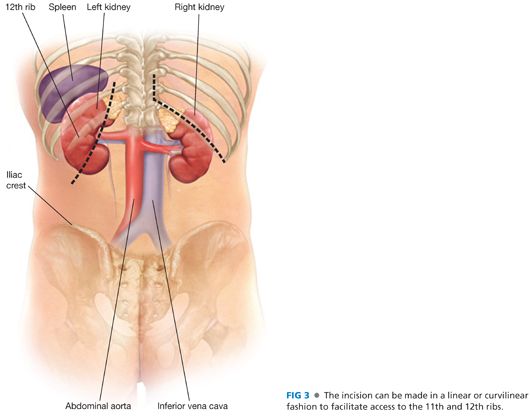
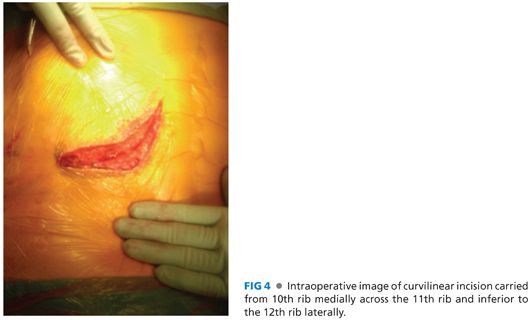
■ A curvilinear incision is made from a paramedian position (4 to 5 cm from the spine) over the left 10th rib and carried inferolaterally toward the iliac crest. Alternatively, a straighter incision over the 11th or 12th rib, depending on the position of the gland on CT scan, with a more vertical upward incision medially may be made (FIGS 3 and 4).
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








