■ Additional imaging studies may be required depending on the functionality of the tumor (metaiodobenzylguanidine [MIBG] for pheochromocytoma in select cases, adrenal vein sampling for hyperaldosteronism, etc.).
■ Fine needle aspiration or core biopsy is not recommended if adrenocortical carcinoma is suspected but may be useful if metastasis to the adrenal gland is in the differential and the adrenal tumor is the most accessible site of metastasis for biopsy in the setting of multiple sites of metastatic disease. If biopsy is performed, it is imperative to first biochemically rule out a pheochromocytoma.
SURGICAL MANAGEMENT
■ Adrenal tumors, if benign appearing by imaging criteria, nonfunctional, and therefore not requiring resection, should be reevaluated with at least one additional CT scan or MRI 6 to 12 months after the initial imaging study to ensure stability in size and internal imaging characteristics. Some advocate for a longer period of follow-up imaging for 2 years with reevaluation of biochemistry for 4 more years.2
■ Functional tumors leading to hormone excess, indeterminate masses, and those suspected of being adrenocortical carcinoma or isolated metastatic disease from another primary tumor without evidence of widespread metastatic disease should be removed.
Preoperative Planning
■ The surgeon must evaluate available imaging studies for tumor involvement of adjacent organs, vessels, and lymphadenopathy. Invasion of major vessels (vena cava) or adjacent organs may require additional teams or different approaches to the tumor. As CT tends to overestimate invasion of adjacent vessels, MRI with magnetic resonance venogram can be especially helpful to assess for vena cava invasion or intracaval tumor thrombus.
■ The risks, benefits, and alternatives to surgery are discussed with the patient, including potential need for steroid supplementation in the postoperative setting. Patients with pheochromocytomas should be adequately alpha blocked and volume replete. Beta blockade may also be necessary. In patients with hyperaldosteronism, a potassium level should be checked the morning of surgery and treated if necessary.
■ Routine prophylactic antibiotics and deep vein thrombosis (DVT) prophylaxis is administered prior to surgery, and sequential compression devices are applied.
■ A general endotracheal anesthetic is administered and an epidural is often placed for postoperative pain management.
■ Common to all approaches, skin preparation with clipping rather than shaving is preferred, and the surgical area is prepped and draped in a sterile fashion.
Positioning
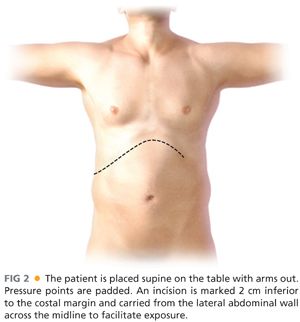
■ The patient is placed supine on the table with arms out to the side, and all pressure points are padded appropriately (FIG 2).
TECHNIQUES
RIGHT ADRENALECTOMY
Exposure
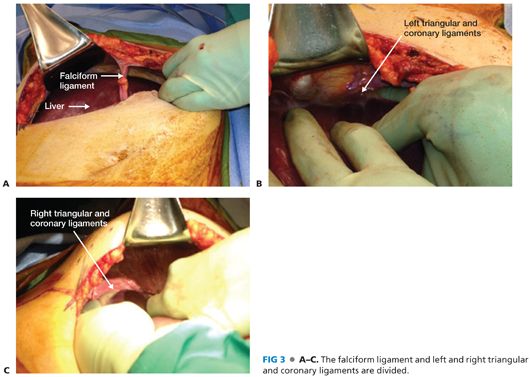
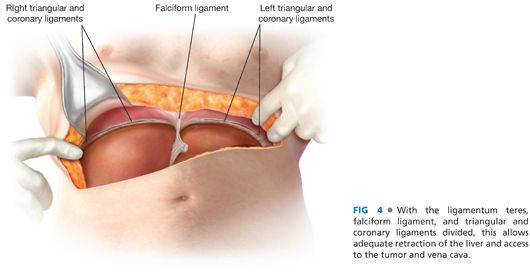
■ A wide right subcostal incision is made and carried across the midline to the midleft abdomen. The subcutaneous fat, fascia, abdominal wall musculature, and posterior fascia are incised with cautery. The peritoneum is entered sharply with scissors and the incision opened to its full length. The ligamentum teres is divided between sutures and the peritoneal cavity is inspected in a systematic manner, assessing for evidence of metastatic disease or other abnormalities. The falciform ligament, triangular, and coronary ligaments of the left and right lobes of the liver are divided to allow for full mobility of the liver during retraction (FIGS 3 and 4).
■ Ultrasound of the liver is also performed to assess for metastatic disease not identified on preoperative imaging, and the vena cava may also be evaluated sonographically for evidence of intracaval tumor thrombus or direct tumor invasion.
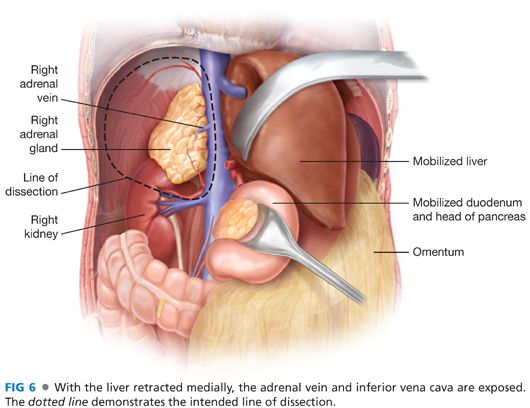
■ The hepatic flexure of the colon may need to be mobilized, and if a Kocher maneuver is needed, it should be done at this time. The right lobe of the liver is retracted medially to expose the retroperitoneum and allow access to the area of the tumor and vena cava. A retractor system is placed. The Omni retractor provides excellent retraction as well as the critically important ability to retract the costal margin and ribs as superiorly and anteriorly as possible. A large saline-soaked towel is placed against the bowel with retractors to not only provide exposure but also to exclude the rest of the peritoneal cavity and minimize potential seeding of the peritoneal cavity by a malignant tumor (FIG 5).

Dissection
■ The posterior peritoneal lining over the retroperitoneum is incised over the superior half of the right kidney and carried from medial to lateral out to the side of the abdominal wall. Medial dissection should proceed carefully to the vena cava, making sure not to divide branches of the renal artery supplying the upper portion of the kidney or venous branches draining to the renal vein. Small branches supplying and draining the adrenal gland should be carefully ligated and divided. Any lymph nodes posterior to the renal hilum should be included in the dissection (FIGS 6 and 7).

■ The fat overlying and just superior to the kidney is mobilized from inferior to superior, making this tissue the inferior margin, using cautery, silk sutures, and other hemostatic devices as needed, making sure not to create a nonexistent plane between the inferior aspect of the tumor and the superior aspect of the kidney. The peritoneal lining should remain intact over the anterior aspect of the tumor to serve as the anterior margin if not already invaded by the tumor (FIG 8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








