Ablative Lasers, Chemical Peels, and Dermabrasion: Introduction
|
Years of damaging ultraviolet light exposure manifest clinically as a sallow complexion with roughened skin surface texture and variable degrees of dyspigmentation, wrinkling, and laxity.1,2 Other cutaneous insults such as scars from acne, trauma, or surgery also affect the appearance of the skin. Histologically, these extrinsic aging and traumatic effects are usually limited to the epidermis and upper papillary dermis and, thus, amenable to treatment with a variety of ablative and nonablative lasers, chemical peeling agents, and dermabrasion. The armamentarium of lasers and chemical peeling agents available to treat cutaneous photodamage, and textural irregularities is larger than ever. The most appropriate treatment technique is dependent on the severity of the photodamage or scarring, the expertise of the dermasurgeon, and the expectations and lifestyle of the individual patient.
Ablative Laser Skin Resurfacing
For years, fully ablative laser skin resurfacing (LSR) with the carbon dioxide laser (CO2) was the gold standard in skin resurfacing. Developed in the mid-1990s, traditional multipass ablative LSR with a CO2 laser demonstrated excellent efficacy for the treatment of rhytides, photodamage, and scars.3–6 However, popularity of the procedure waned due to the extended postoperative recovery required, the inability to treat nonracial areas, and the significant risk of side effects and complications including persistent erythema, permanent hypopigmentation, and scarring.7,8
To mitigate the problems associated with traditional ablative LSR, nonablative laser devices were subsequently introduced.9–30 The 532-nm-potassium titanyl phosphate (KTP),18,19 585- to 595-nm pulsed dye,11,12 1,064- and 1,320-nm Neodymium:yttrium-aluminum-garnet (Nd:YAG),17–21 and 1,450-nm diode lasers,9,10,25,26 and a 550- to 1,200-nm intense pulsed light device (IPL)12–15 were developed to stimulate dermal neocollagenesis without epidermal injury or significant recovery. Each of these systems demonstrated histologic changes in dermal collagen, a series of treatments often yielded limited clinical improvement. Nonablative LSR is described in detail in Chapter 252.
A novel concept in skin resurfacing, termed fractional photothermolysis, was developed by Manstein and colleagues in 2004.31 Fractional photothermolysis involves the creation of microscopic thermal wounds regularly interspersed within areas of nontreated skin. The intact nontreated skin forms bridges between the microscopic treatment zones (MTZ), thereby leading to rapid healing. The wound healing response differs from fully ablative techniques because the epidermal tissue that is spared between the thermal zones contains viable transient amplifying cells that are capable of rapid re-epithelialization.
Fractional photothermolysis devices include a 1,550-nm erbium-doped fiber, 1,540-nm erbium glass, and 1,320-nm or 1,440-nm Nd:YAG laser.32–37 Their midinfrared wavelengths target water-containing tissue to effect photocoagulation of narrow columns of skin at depths of 200–500 μm at intervals of 200–300 μm. Histologic evaluation of skin immediately after treatment reveals thermal injury sharply confined to these narrow columns extending from the epidermis to the mid-dermis. Microscopic epidermal necrotic debris (MEND) exfoliate within days, producing a bronzed appearance to the skin. Since the stratum corneum has a low water content, it remains intact immediately after treatment. Although there is gradual exfoliation of the epidermis with resultant improvement in superficial dyspigmentation, these devices are considered nonablative due to the lack of significant epidermal disruption after treatment. As such, nonablative fractional laser resurfacing procedures offer patients a treatment option with little postoperative recovery. However, a series of treatments is required for the best results and, to date, nonablative fractional LSR demonstrates only modest improvement of severe photodamage, laxity, and rhytides compared to ablative LSR.38–41
A continued desire for superior clinical results while maintaining a manageable recovery and side effect profile gave rise to the combination of ablative laser devices that adhere to the concept of fractional photothermolysis. Ablative fractional resurfacing (AFR) with either a CO2 or erbium:YAG (Er:YAG) laser ablates a fraction of both the epidermis and dermis allowing rapid re-epithelialization with a favorable side-effect profile. Pedicles of thermally induced dermal coagulation extend to far greater depths than those delivered by nonablative fractional devices, thereby inducing greater tissue contraction and neocollagenesis. Due to the less invasive nature of AFR, nonfacial areas such as the neck, chest, and dorsal hands can be safely treated. In addition, the fractional characteristics of treatment reduces recovery time, postoperative discomfort, side effects, and complications associated with traditional multipass ablative LSR.43
The ideal patient for ablative cutaneous laser resurfacing has a fair complexion [skin phototype (SPT) I or II], rhytides, other signs of photodamage, or atrophic scars that are amenable to treatment, and realistic expectations of the treatment.3 Adequate preoperative patient evaluation and education are essential to optimize the clinical outcome (Table 251-1). Proper patient selection is paramount because ablative LSR can be complicated by a prolonged postoperative recovery, pigmentary alterations, or unexpected scarring. The patient’s emotional ability to tolerate an extended convalescence is an important factor in determining the most appropriate choice of laser. Although CO2 or modulated Er:YAG LSR produces the most dramatic clinical results, some patients may be unable to tolerate the intensive recovery period that is required. For patients who acquiesce to a moderate amount of recovery, AFR may be a more appropriate choice as intense erythema and serosanguinous drainage are evident for 2–3 days, followed by complete reepithialization and diminution of erythema by day 6 or 7 compared to fully ablative LSR in which re-epithelialization and intense erythema extends to 5–7 days and several weeks, respectively. For patients either unable or unwilling to tolerate more than 1 or 2 days of postoperative healing, a nonablative laser procedure may be a more suitable choice (see Chapter 252).
|
Currently, no consensus exists among laser experts regarding the most appropriate preoperative regimen for ablative LSR patients. The use of topical retinoic acid compounds, hydroquinone bleaching agents, or α-hydroxy acids for several weeks before ablative cutaneous resurfacing has been touted by some as a means of speeding recovery and decreasing the incidence of postinflammatory hyperpigmentation; however, others have shown that these preparations do little to affect postoperative pigmentation, in particular.44 Topical tretinoin enhances penetration of chemicals through the skin and has been shown to accelerate postoperative re-epithelialization after dermabrasion or deep chemical peels.45 Because ablative laser–induced wounds are intrinsically different from those created by physically destructive methods, laser skin penetration is not typically affected by the topical application of any of these medications.46
Due to the moist, de-epithelialized state of ablative laser–resurfaced skin and the possibility of bacterial contamination and overgrowth, many laser surgeons advocate oral antibiotic prophylaxis. This practice remains controversial, due to the findings of a controlled study that demonstrated no significant change in post–laser resurfacing infection rate in patients treated with prophylactic antibiotics.47
The first system developed for cutaneous laser resurfacing was the CO2 laser, which was approved by the US Food and Drug Administration (FDA) in 1996. The earliest systems were continuous-wave CO2 lasers, which were effective for gross lesional destruction; however, these systems could not reliably ablate fine layers of tissue because of their prolonged tissue-dwell times which were responsible for unacceptably high rates of scarring and dyspigmentation.48–52 With the subsequent development of high-energy pulsed lasers, it became possible to safely apply higher energy densities with exposure times that were shorter than the thermal relaxation time of water-containing tissue, thereby lowering the risk of thermal injury to surrounding nontargeted tissue.3,4,53
Two of the first high-energy pulsed-laser systems developed were the Ultra-Pulse 5,000 and SilkTouch lasers (Lumenis Corp., Yokeam, Israel). The UltraPulse emits individual CO2 pulses (ranging from 600 μs to 1 ms) with peak energy densities of 500 mJ, whereas the SilkTouch is a continuous-wave CO2 system with a microprocessor scanner that continuously moves the laser beam so that light does not dwell on any one area for more than 1 ms. The peak fluences delivered per pulse or scan range from 4–5 J/cm2, which are the energy densities necessary for complete tissue vaporization.5,6,50,54 Studies with these and other pulsed and scanned CO2 laser systems have shown that after a typical skin resurfacing procedure, water-containing tissue is vaporized to a depth of approximately 20–60 μm, which produces a zone of thermal damage ranging from 20–150 μm.6,50,55–57
The short-pulsed Er:YAG laser was introduced as an alternative to the CO2 laser for skin resurfacing in an attempt to minimize the recovery period and limit side effects while maintaining clinical benefit. The Er:YAG laser is a more precise ablative tool than is the CO2 laser and emits 2,940-nm light that corresponds to the 3,000-nm absorption peak of water. The absorption coefficient of Er:YAG light is 12,800 cm−1 (compared with 800 cm−1 for that of the CO2 laser), which makes it 12–18 times more efficiently absorbed by water-containing tissue than CO2 laser energy.58 The pulse duration (mean, 250 μs) is also much shorter than that of the CO2 laser, thereby resulting in decreased thermal diffusion, less effective hemostasis, and increased intraoperative bleeding that often hampers deeper dermal treatment. In addition, because of limited thermal skin injury, the amount of collagen contraction is also reduced with Er:YAG treatment compared with that observed to CO2 laser irradiation.5,59
The Er:YAG laser’s efficient rate of absorption, short exposure duration, and direct relationship between fluence delivered and amount of tissue ablated leads to 2–4 μm of tissue vaporization per Joule per square centimeter, which produces a shallow level of tissue ablation. Much narrower zones of thermal necrosis, averaging only 20–50 μm, are therefore produced.58,60–62
Conditions amenable to short-pulsed Er:YAG laser resurfacing include superficial epidermal or dermal lesions, mild photodamage, and subtle dyspigmentation. The major advantage of short-pulsed Er:YAG laser treatment is the shorter recovery period after therapy. Re-epithelialization is completed within an average of 5.5 days, compared with 8.5 days for multipass CO2 procedures.60–62 Postoperative pain and duration of erythema are reduced after short-pulsed Er:YAG laser resurfacing, with postoperative erythema resolving within 3–4 weeks. Because there is less thermal injury and trauma to the skin, the risk of pigmentary disturbance is also decreased, which makes the short-pulsed Er:YAG laser a good alternative in treating patients with darker skin phototypes.3,63 The major disadvantages of the short-pulsed Er:YAG laser are its limited ability to effect significant collagen shrinkage and its failure to induce new and continued collagen formation postoperatively.3,60,64 Because of this, the final clinical result is often less impressive than that produced by CO2 laser skin resurfacing for deeper rhytides.
Through the natural progression of technology, modulated Er:YAG lasers systems were developed to improve hemostasis and increase the amount of collagen remodeling produced.65 The Er:YAG–CO2 hybrid laser system delivers both ablative Er:YAG and coagulative CO2 laser pulses. The Er:YAG component generates fluences of up to 28 J/cm2 with a 350-μs pulse duration, and excellent hemostasis is provided by the CO2 component, which can be programed to deliver 1- to 100-ms pulses at 1–10 W of power. Zones of thermal necrosis measuring as much as 50 μm have been observed depending on the treatment parameters used, and significant increase in collagen thickness has been noted 3 months after four passes with a device using this hybrid technology.66 Another modulated Er:YAG device is a dual-mode Er:YAG laser that emits a combination of short (200- to 300-μs) pulses and long coagulative pulses to achieve tissue ablation depths of up to 200 μm per pass.65,66 The desired depth of ablation and coagulation can be programed through a touch-screen control panel. Several investigators have studied the histologic effects of dual-mode Er:YAG laser resurfacing and found a close correlation between the programed and actual measured depths of ablation.67,68 The actual zones of thermal injury correlate well with the first-pass parameters, with decreasing coagulative efficiency on subsequent passes. The variable-pulsed Er:YAG laser system delivers pulse durations ranging from 500 μs to 10 ms. Shorter pulse durations are used for tissue ablation and longer pulses are used to effect coagulation and zones of thermal injury as with the CO2 laser.69–71
Ablative Fractional Lasers
Since the introduction of the first fractional laser in 2004, numerous devices have been developed to apply the concept of fractional photothermolysis.72 Initially, ablative fractional treatments were simply traditional CO2 or Er:YAG lasers with software modifications to deliver smaller spot sizes and lower density scans. With advances in technology, there are currently a wide range of fractional ablative lasers that incorporate either a 10,600-nm CO2, 2,940-nm Er:YAG or 2,790-nm yttrium scandium-gallium-garnet (YSGG) wavelength. Differences in depth of ablation and coagulation, variation in available spot size and shape, application of energy (stamped vs. rolling), and ergonomics of the handpiece distinguish one laser from the other. Little difference in overall clinical improvement has been demonstrated using several different fractional ablative resurfacing lasers73; however, further investigation is necessary to elucidate the most appropriate treatment parameters and subsequently maximize clinical outcomes for each individual device.
Most ablative laser resurfacing is performed as an outpatient procedure in an ambulatory surgery facility. Regional laser skin resurfacing (perioral or periorbital) can be performed with local anesthesia with no additional analgesia. Full-face LSR often requires additional analgesia, including one or more of the following: oral sedation, nerve blocks, tumescent anesthesia, topical anesthetic creams, and intravenous (IV) sedation. Topical anesthesia protocols have been outlined using either lidocaine cream application for several hours before LSR to enhance tissue hydration and anesthetic penetration74 or a cream-based formulation that dries to a flexible membrane, which is peeled away from the skin before laser irradiation.75
Despite their obvious advantages, these topical regimens are frequently more time consuming and less uniformly effective. For this reason, deeper forms of anesthesia for full-face ablative laser procedures is often used, including regional nerve blockade and IV sedation to provide more complete anxiolysis, amnesia, and sedation.76 If IV sedation or general anesthesia is used, special precautions must be taken in the presence of oxygen. High-powered lasers have been reported to be the source of operating room fires, so care must be taken to eliminate exposure to flammable objects. A smoke evacuator also must be used to avoid inhalation of the laser plume.
The objective of ablative LSR is to vaporize tissue to the level of the papillary dermis. Limiting the depth of penetration decreases the risk of scarring and permanent pigmentary alteration. When choosing treatment parameters, several factors should be given consideration, including anatomic site to be resurfaced, the skin phototype of the patient, and previous skin treatments delivered.5,77 In general, thinner skin (e.g., periorbital) requires fewer laser passes and laser resurfacing of nonfacial skin (e.g., neck, chest) should be avoided due to the relative paucity of pilosebaceous units in these areas.77 To reduce the risk of excessive thermal injury during multipass procedures, partially desiccated tissue should be removed manually with wet gauze after each laser pass to expose the underlying dermis.78
The depth of ablation is directly correlated with the number of passes performed and usually is restricted to the epidermis and upper papillary dermis.79 However, stacking laser pulses by treating an area with multiple passes in rapid succession or by using a high-overlap setting on a scanning device leads to excessive thermal injury to the skin with subsequent increased risk of scarring.7,78 An ablative plateau is reached which results in less effective tissue ablation and increased tissue heating. This effect is most likely caused by reduced tissue water content after initial desiccation, thereby diminishing selective energy absorption.78 The avoidance of pulse stacking and incomplete removal of partially desiccated tissue is paramount to prevention of excessive thermal accumulation with the use of any laser system.
In an attempt to address many of the difficulties associated with multipass CO2 LSR, refinements in surgical technique have been developed. A minimally traumatic single-pass CO2 laser resurfacing procedure has been described that results in faster re-epithelialization and a more improved side effect profile than have been reported with the multiple-pass technique.80 Partially desiccated tissue is not removed (as is standard with multipass procedures); rather, the lased skin is left intact to serve as a biologic wound dressing. Additional laser passes can then be applied focally only in areas of more extensive involvement to limit unnecessary thermal and mechanical trauma to less involved skin. Subsequent reports have substantiated the improved side effect profile of this less aggressive procedure.81–83
The short-pulsed Er:YAG laser fluences used most often range from 5–15 J/cm2, depending on the degree of photodamage and anatomic location. On irradiation, laser-induced ejection of desiccated tissue from the target site produces a distinctive popping sound. Thermal energy is confined to the selected tissue, with minimal collateral thermal damage. Because little tissue necrosis is produced with each pass of the laser, manual removal of desiccated tissue is often unnecessary. The ablation depth with the short-pulsed Er:YAG laser does not diminish with successive passes because the amount of thermal necrosis is nominal. It takes three to four times as many passes with the short-pulsed Er:YAG laser to achieve similar depths of penetration as with one pass of the CO2 laser at typical treatment parameter settings.3,5 To ablate the entire epidermis with the short-pulsed Er:YAG laser using a fluence of 5 J/cm2, at least two or three passes must be performed, which increases the possibility of uneven tissue penetration. Treatment of deeper dermal lesions or areas of the face with extensive photodamage and dermal elastosis may require up to 9 or 10 passes of the short-pulsed Er:YAG laser, whereas the CO2 laser would effect similar levels of tissue ablation in 2 or 3 passes.6,50,58
Pinpoint bleeding caused by inadequate hemostasis and tissue color change after multiple short-pulse Er:YAG passes can impede adequate clinical assessment of wound depth. Irradiated areas whiten immediately after treatment and then quickly fade. These factors render it more difficult to determine treatment endpoints and, thus, require extensive knowledge of laser-tissue interaction on the part of the operator. Modified Er:YAG ablative laser resurfacing provides better hemostasis and visualization of the treatment area because of the added thermal effects on the tissue.84
Ablative Fractional Resurfacing
After appropriate informed consent, eye protection, and sedation are employed, ablative fractional laser skin resurfacing is best performed in a sequential fashion adhering to cosmetic units. Meticulous technique with placement of nonoverlapping rows will minimize bulk heating during treatment. Additional passes are delivered perpendicular to the previous pass until a desired number of passes has been reached. Optimal settings will vary depending upon the laser device used and the severity of the condition being treated. Average settings for a common fractional CO2 laser (Repair, Solta Medical Inc., Hayward, CA) range 40–70 mJ with a coverage density of 30% to 50%. Treatment of the periocular and neck skin require a decrease in both fluence and coverage density. Although patient satisfaction and clinical results may improve with the use of higher fluences, increased adverse events such as pain, erythema, and postoperative dyspigmentation are more often observed when higher treatment densities are applied.85 Ablative fractional lasers generally require only one treatment to achieve patient satisfaction; however, reappraisal of photodamage, rhytides, or scarring can be performed 6–12 months postoperatively to assess if additional treatments are clinically warranted.
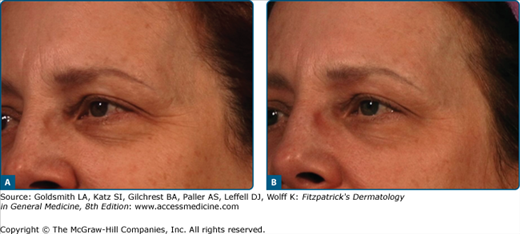
The clinical and histologic benefits of cutaneous laser resurfacing are numerous. With the CO2 laser, most studies have shown at least a 50% improvement over baseline in overall skin tone and wrinkle severity (Fig. 251-1).4,86–90 The greatest advantages associated with CO2 laser skin resurfacing are the excellent tissue contraction, hemostasis, prolonged neocollagenesis, and collagen remodeling that result. Histologic examination of laser-treated skin demonstrates replacement of epidermal cellular atypia and dysplasia with normal, healthy epidermal cells from adjacent follicular adnexal structures.50,56 The most profound effects occur in the papillary dermis, where coagulation of disorganized masses of actinically induced elastotic material are replaced with normal compact collagen bundles arranged in parallel to the skin’s surface.91,92 Immediately after CO2 laser treatment, a normal inflammatory response is initiated, with granulation tissue formation, neovascularization, and increased production of macrophages and fibroblasts.56
Persistent collagen shrinkage and dermal remodeling are responsible for much of the continued clinical benefits observed after CO2 laser resurfacing and are influenced by several factors.92,93 Thermal effects of laser irradiation of skin produce collagen fiber contraction at temperatures ranging from 55°C–62°C (131°F–143.6°F) through disruption of interpeptide bonds, which results in a conformational change to the collagen’s basic triple-helical structure.94,95 The collagen molecule is thereby shortened to approximately one-third of its normal length. Collagen fibers with laser-induced shrinkage may act as the contracted scaffold for neocollagenesis, which leads to subsequent production of the newly shortened form. In turn, fibroblasts that migrate into laser wounds after resurfacing may upregulate the expression of immune-modulating factors that serve to enhance continued collagen shrinkage.96
Because modulated Er:YAG lasers were developed to produce a greater thermal effect and tissue contraction than did their short-pulsed predecessors, investigators compared collagen tightening induced by the CO2 laser with that of the CO2–Er:YAG hybrid laser system.69 Intraoperative contraction of approximately 43% was produced after three passes of the CO2 laser, compared with 12% contraction after Er:YAG irradiation. At 4 weeks; however, the CO2 laser– and Er:YAG laser–treated sites were contracted to the same degree which highlights the different mechanisms of tissue tightening observed after laser treatment. Immediate thermal-induced collagen tightening was the predominant response seen after CO2 irradiation, whereas modulated Er:YAG laser resurfacing did not produce immediate intraoperative contraction, but instead induced slow collagen tightening.65,69
Fractional ablative lasers have been used to successfully treat facial and nonfacial photodamage and a variety of scars, including atrophic, hypertrophic, hypopigmented, and traumatic scars.43,73,97–100 (Figs. 251-2 and 251-3) Improvement in post-CO2 laser-induced hypopigmentation, residua from infantile hemangioma, and actinic cheilitis has also been reported.42,43 Others suggest a supportive role for fractional ablative lasers during Q-switched laser tattoo removal.101
Clinical improvement of photodamage and rhytides following AFR has been demonstrated in several published studies. A 2,940-nm Er:YAG fractional device was used to treat 28 patients with photodamaged skin. Two months after a single treatment, 75% of patients rated the results as good to excellent with improvement lasting 6–9 months.102 Another study using a fractional CO2 laser on 32 patients demonstrated more than 50% improvement in wrinkles, epidermal pigment, and solar elastosis 6 months after one treatment session.97 In a pilot study of 12 patients, 51% to 75% improvement of photodamage and acne scars after two successive fractional CO2 laser treatments was reported.103
Ablative fractional laser skin resurfacing has been used to improve skin topography in both atrophic and hypertrophic scars. In a study of 15 patients with SPT I-IV and moderate-to-severe atrophic scarring, an average of 66.8% improvement in scar depth after 2–3 fractional CO2 laser treatments was achieved.98 Good clinical improvement in 23 of 25 subjects with moderate-to-severe atrophic scarring who received up to 3 treatments with a fractional CO2 laser was demonstrated in yet another published report.99 Sustained improvement of atrophic scars and an overall improvement of clinical appearance including pigmentation and rhytides was noted. Quantitative volumetric improvement of nonacne atrophic traumatic or surgical scars has also been reported. Twenty-two atrophic scars received three fractional CO2 laser treatments with image analysis at 6 months demonstrating clinical and volumetric improvement as evidenced by mean reduction of scar volume and depth by 38% and 36%, respectively.100
Side effects associated with CO2 laser skin resurfacing vary and are related to the expertise of the operator, the body area treated, and the skin phototype of the patient (Table 251-2). Certain tissue reactions, such as erythema and edema, are expected in the immediate postoperative period and are not considered adverse events. Erythema can be intense and may persist for several months after the procedure. The degree of erythema correlates directly with the depth of ablation and the number of laser passes performed.3,104 It may also be aggravated by underlying rosacea or dermatitis. Postoperative erythema resolves spontaneously but can be reduced with the application of topical ascorbic acid, which may serve to decrease the degree of inflammation.105,106 It should not be used for at least 4 weeks after the procedure to avoid irritation. Likewise, other topical agents such as retinoic acid derivatives, glycolic acid, fragrance- or chemical-containing cosmetics, and sunscreens should be strictly avoided in the early postoperative period until substantial healing has occurred.104
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree